Annual NHS Scotland Climate Emergency & Sustainability Report 2024
This year’s report shows how NHS Scotland is working to reduce its environmental impact and adapting its infrastructure and services to the address the risks presented by climate change. It also shows that many changes the NHS seeks to deliver have other potential benefits.
Part 1 – Progress Achieved
Leadership and Governance
NHS Scotland is part of a concerted drive to decarbonise health systems across the globe, including working with UK partners. The World Health Organisation’s Alliance for Transformative Action on Climate and Health (ATACH) has over 80 countries and areas, including the UK, that have made commitments at Ministerial level to strengthen climate resilience and/or reduce the emissions of their health systems.
NHS Scotland Climate Emergency and Sustainability Board
The NHS Climate Emergency & Sustainability Board (CE&S Board) brings together leaders from across the Scottish Government, NHS Scotland and the wider public sector to ensure that NHS Scotland becomes a net zero, environmentally sustainable organisation. It takes an oversight role in supporting NHS Scotland to becoming a more climate change resilient organisation.
Energy Transition Board
The NHS Scotland Energy Transition Board (ETB) was established in 2023 to assist NHS Scotland to decarbonise its energy use and reports to the CE&S Board.
Scottish Water and NHS Scotland Committee on Climate Change and Environment
The committee was established in 2023 to identify and take forward opportunities for Scottish Water and NHS Scotland to co-operate in achieving their legal duties to contribute to the achievement of Scotland’s greenhouse gas emission reduction targets, Scotland’s climate adaptation programme and to further the conservation of biodiversity.
Leading By Example: Medical Gases and International Recognition
NHS Scotland is a member of Health Care Without Harm Europe (HCWH), an organisation which exists to create a sustainable healthcare sector - one that does no harm to patients or our planet. In 2023, NHS Scotland won Health Care Without Harm’s European Sustainable Healthcare Project of the Year award for its work in reducing the climate impact of anaesthetic gasses. Following Scotland’s example, HCWH has been encouraging other countries across Europe to make similar changes to reduce climate emissions from anaesthesia.
Annual Delivery Plans and Medium Term Plans
Annual Delivery Plans (ADPs) are the mechanism by which Health Boards set out their priorities for delivery in the coming year. Medium Term Plans (MTPs) focus on a three-year period. 2022-2023 was the first year in which time-related, climate change and environmental objectives were put into these plans.
Climate Change Adaptation
Scotland’s climate is changing faster than expected according to research published by the James Hutton Institute in December 2023[2]. According to this research:
- “Between 1990 to 2019, February and to a lesser extent April have become wetter, particularly in the west, by up to 60%, exceeding the projected change by 2050 of 45-55%.”
- “Scotland is on track to exceed “a 2°C increase in temperature by the 2050s, with the months from May to November experiencing up to 4°C of warming over the next three decades (2020-2049).”
- “The number of days of consecutive dry weather – an indicator for drought and wildfire risk – are also expected to increase in drier months, such as September.”
Climate change exacerbates existing health risks and introduces new challenges, ranging from the spread of infectious diseases to the intensification of heatwaves and extreme weather events that will impact the health of the population, healthcare assets and services. NHS Scotland plays a pivotal role in safeguarding the life and health of communities by developing climate-resilient health systems capable of responding to these evolving threats.
NHS Boards have carried out Climate Change Risks Assessments (CCRAs) to identify the risks that could impact their healthcare assets and services and developed high-level Adaptation Plans with measures to address the risks identified.
Of NHS Scotland’s 22 NHS Boards:
- Twenty NHS Boards have completed Climate Change Risks Assessments; and
- Fifteen NHS boards have developed high-level adaptation plans.
A first analysis of Climate Change Risks Assessments by NHS Assure shows prevalent climate hazards, including higher average temperature, extended periods of hot weather, cold spells, combined climatic effects, flooding, heavy downpours and driving rain. These hazards pose significant threats to critical healthcare infrastructure such as hospitals, GP surgeries, community health centres and other core services.
As climate change intensifies, addressing these risks becomes imperative to enhance the resilience of Scotland’s healthcare system and ensure its ability to provide uninterrupted and effective services to the communities it serves. Recognising this urgency, NHS boards have identified adaptation measures such as enhancing critical site access, reassessing monitoring systems, formulating contingency plans and implementing renewable energy and nature-based solutions.
Example: Resilience and Adaptation – NHS Ayrshire & Arran
NHS Ayrshire & Arran is part of a multi-agency group, the Ayrshire Local Resilience Partnership (ALRP). This is made up of organisations such as Scottish Fire and Rescue Service, Police Scotland, Scottish Ambulance Service, the Scottish Environmental Protection Agency, the Met Office, Scottish Water and transport operators such as CalMac and Prestwick Airport.
The ALRP has a severe weather plan and this outlines the actions to be taken depending on the level of warning received. The ALRP will also co-ordinate volunteer groups if required during severe weather, for example the 4x4 vehicle volunteer group. West of Scotland Regional Resilience Partnership (WoSRRP) would delegate priority of these services to those with the greatest need.
Environmental Management Systems
An Environmental Management System (EMS) is an efficient way to reduce the environmental impacts of NHS Boards, comply with legislative requirements and find operational efficiencies. It comprises policies and procedures for:
- the management of resource use;
- energy and water consumption;
- waste generation;
- carbon emissions; and
- effectively supporting local biodiversity.
To support the development of EMS in Boards, a toolkit for EMS implementation is being developed at a national level, on a ‘Once for Scotland’ basis. Training sessions, on using the national EMS tool, and an EMS implementation workshop by the Institute of Environmental Management and Assessment (IEMA) were delivered in 2023 to help build knowledge and skills to use the tool and build confidence to implement EMS. Further training sessions and workshops for the staff involved in implementation are being planned.
Building Energy
Building energy emissions, from heating, lighting, and hospital activity, are the largest single source of direct climate change emissions for NHS Scotland. The NHS uses electricity to power its buildings, equipment and (increasingly) its vehicles. It also needs to heat and cool its buildings. Greenhouse gases are emitted through the burning of fossil fuels for heat at NHS sites and also in the generation of electricity supplied through the national grid.
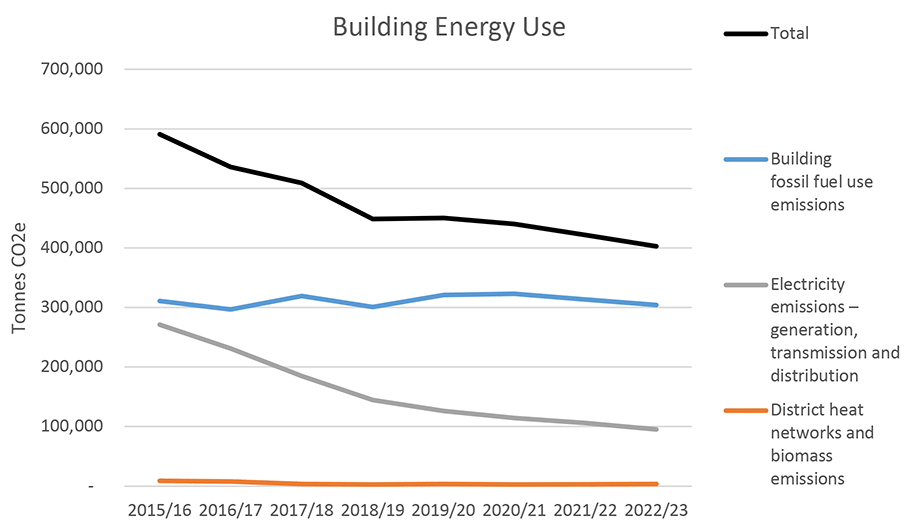
NHS Scotland’s total heat and power emissions have reduced by 31% between 2015-16 and 2022-23. Emissions have fallen much more quickly than energy use. This is largely due to the decarbonisation of the grid, for example, using gas instead of coal for electricity generation, and improvements to energy efficiency.
The NHS Scotland Energy Transition Board (the ETB) has been set up to:
- Coordinate national support, including funding, to Health Boards for building energy decarbonisation; and
- Coordinate and oversee, at a strategic level, a programme of major energy decarbonisation projects for the NHS.
The 20 NHS sites with the largest climate change emissions made up over 60% of total NHS building emissions in 2022/23. These sites are being treated as strategic priorities as they are critical to decarbonising the NHS.
Some of these sites present early opportunities for moving to renewable heating systems because they are modern, energy efficient buildings and there are promising potential renewable heat sources on site or nearby. Other sites will require long-term investment to modernise them before they move to renewable heating systems.
| Health Board | Site | Emissions, tCO2e |
|---|---|---|
| NHS Grampian | Foresterhill Health Campus, includes Royal Cornhill Hospital | 35,600 |
| NHS Greater Glasgow & Clyde | Queen Elizabeth University Hospital Campus | 28,700 |
| NHS Tayside | Ninewells Hospital | 24,300 |
| NHS Greater Glasgow & Clyde | Glasgow Royal Infirmary | 18,000 |
| NHS Lothian | Royal Infirmary of Edinburgh | 14,600 |
| NHS Lothian | Western General Hospital | 13,600 |
| NHS Highland | Raigmore Hospital | 15,500 |
| NHS Lothian | St Johns Hospital & Howden Health Centre | 11,900 |
| NHS Greater Glasgow and Clyde | Gartnavel Health Campus | 11,000 |
| NHS Fife | Victoria Hospital | 10,200 |
| NHS Forth Valley | Forth Valley Royal Hospital | 8,800 |
| National Waiting Times Centre | Golden Jubilee National Hospital | 8,100 |
| NHS Dumfries & Galloway | Dumfries & Galloway Royal Infirmary | 7,100 |
| NHS Greater Glasgow & Clyde | Royal Alexandra Hospital | 7,000 |
| NHS Lanarkshire | Wishaw District General Hospital | 6,500 |
| NHS Lothian | Royal Hospital For Children & Young People, Edinburgh | 5,700 |
| NHS Ayrshire & Arran | Crosshouse Hospital Campus including Ayrshire Maternity | 6,100 |
| NHS Borders | Borders General Hospital | 5,300 |
| NHS Greater Glasgow and Clyde | Monklands District General Hospital | 5,100 |
| NHS Tayside | Perth Royal Infirmary | 4,900 |
Sustainable Transport
Transport is a significant contributor to emissions in Scotland, making up over 25% of total emissions. The table below shows that reported greenhouse gas emissions from combined NHS fleet and business travel have increased from 32,648 tCO2e in 2019/20 to 42,450 tCO2e in 2022/23, a 30% increase. Reporting of fleet and business travel emissions has improved since 2019/20 and the higher figures do not necessarily mean an increase in actual emissions.
Table 3: NHS Scotland Reported Fleet and Business Travel emissions 2019/20, 2021/22, 2022/23 (Source – Health Board Annual Climate Emergency and Sustainability Reports 2022/23)
Where not all Health Boards have reported, the number of Health Boards reporting is given in brackets after the emissions figure.
| Source of emissions | 2019/20 (tCO2e) | 2021/22 (tCO2e) | 2022/23 (tCO2e) | % Change since 2019/20 |
|---|---|---|---|---|
| Fleet | 26,507 | 29,737 | 30,547 | +15% |
| Business travel | 6,142 (9) | 9,821 (12) | 11,904 (16) | +94% |
| Total | 32,650 | 39,558* | 42,451 | +30%** |
* This differs from the figure for 2021/22 given in the 2023 report due to further data gathered since then.
**The increase in emissions is partly due to more Boards reporting and improved reporting.
Decarbonising the Fleet
In line with the NHS Scotland Climate Emergency and Sustainability Strategy, NHS Boards are working to decarbonise their fleets, focussing first on cars and light commercial vehicles (up to 3.5 tonnes). The table below shows the composition of the fleet for the whole of Scotland as of 23 May 2024. All 18 Health Boards which have a fleet have submitted a return.
| Total Number of All Types of Vehicle | Zero Tailpipe Emissions (i.e. full EVs, no hybrid) | % EVs April 2024 | |
|---|---|---|---|
| Cars | 2228 | 1009 | 45% |
| LCV* | 1933 | 414 | 22% |
| HVs** | 649 | 8 | 1% |
* Light Commercial Vehicles
**Heavy Vehicles
Recent figures show significant progress can be made in a relatively short period of time. Since 2019, NHSScotland has received upwards of £16 million of funding from Transport Scotland by way of the Switched on Fleets programme, allowing Health Boards across Scotland to invest and grow a supporting network of EV chargers and vehicles. There are now over 900 charging points across the NHS Scotland estate, a marked increase from April 2022, when the number of charge points was 538. Initiatives like solar charging and battery storage are planned to help support our energy transition work.
At the time of writing, over a third of the 3000+ NHS Scotland fleet, excluding Scottish Ambulance Service, has transitioned to electric vehicles. Several Boards have fleets where the majority of vehicles are now electric:
- NHS Forth Valley
- NHS Lanarkshire
- NHS Lothian
- NHS Shetland
- NHS Tayside
- NHS Orkney
Whilst it remains to be seen what the dominant technology will be for decarbonising heavy commercial vehicles in a healthcare setting, trials of 16-tonne fully electric vehicles are currently underway within NHS Greater Glasgow & Clyde to test the suitability of a fully electric solution. We also continue to investigate the opportunities for “stepping-stone” technologies such as hydrotreated vegetable oil (HVO) and alternative technologies such as hydrogen fuel cells.
Realistic Medicine and Effective Prescribing
Realistic Medicine
Health and care systems across the world are thinking about how they can deliver Value-Based Health and Care (VBH&C), which focusses on achieving the best value clinical outcomes from the patient’s perspective. By reducing waste and switching to more effective medication programmes, VBH&C can also help tackle the global environmental crisis.
Realistic Medicine is a practice that can improve the resilience of our health and care system by reducing waste and potential harm. It also redirects resource that is currently wasted to higher value and more sustainable care. The Chief Medical Officer published his annual report Realistic Medicine in June 2023. This series of reports sets the strategic direction for the practice of Realistic Medicine. The latest report sets out the climate emergency’s impact on the NHS, and how a value-based healthcare approach can help to mitigate the worst effects.
Effective Prescribing
Effective prescribing can reduce medicine waste and achieve better outcomes for patients. NHS England estimates that the production of medicines and chemicals used by the NHS are responsible for 20% of total NHS emissions.
The Scottish Government and NHS Scotland has published updated Scottish Quality Prescribing Guides covering Respiratory, Polypharmacy, Diabetes, Antidepressants, Benzodiazepines & z drugs[3].
Improved outcomes for patients can be achieved through a person-centred medication review, which can help optimise disease control. A recent EU-funded cross border project, led by the Scottish Government, evaluated the multidisciplinary collaborative approach to deliver pharmacist-led, person-centred medicines reviews, using the 7-steps methodology. 6,481 patients engaged in reviews in primary care, secondary care, outpatient clinics and care homes.
This demonstrated various positive impacts to patient outcomes, care and safety and benefits to the wider healthcare system. An average of 11 interventions were made per patient, with 82% classified as clinically significant and 4% potentially preventing major organ failure or similar. 94% of interventions made were accepted, with the average number of medications reduced from 12 to 11 and 92% of reviews resulted in more appropriate medication use. See: iSIMPATHY summary and evaluation report
An example of where better prescribing can significantly reduce greenhouse gas emissions is in respiratory care. Pressurised Metered Dose Inhalers (pMDIs) contributed around 84,000 tCO2e of emissions in 2022/23, largely driven by the use of short-acting reliever inhalers. Person centred reviews and better prescribing focussing on prevention can help prevent over-use of inhalers. Clinicians can help reduce the environmental impact of inhalers (and improve asthma management) by helping patients to optimise inhaler technique, ensuring adherence with preventer medicines, and reducing reliance on short acting beta agonists.
Unfortunately, as shown in the Part 2 Table 3, emissions from propellant inhalers increased by 3,266 tCO2e between 2021-22 and 2022-23, an annual increase of 4%. The Quality Prescribing Guide for Respiratory was published in April 2024 and can support more improvements to prescribing: Respiratory conditions - quality prescribing strategy: improvement guide 2024 to 2027 - gov.scot (www.gov.scot)
Some Facts about inhalers
- There were approximately 4.5 million pMDI inhalers prescribed in Scotland in 2020/2021.
- A 70% reduction could save 63,000 tCO2e emissions each year, approximately 15,750 trips around the world in a Ford Focus.
- Person centred prescribing has the potential to create significant cost savings, by helping the patient onto a more appropriate treatment regime that can save unnecessary use of medicines and avoid hospitalisations associated with the use of sub-optimal medications.
- UK has high proportion of pMDI use (70%) compared to Scandinavia (10-30%). If NHS Scotland prescribed the same proportion of DPIs as Sweden, 55,000 tCO2e would be saved annually.
Medical Gases
Medical gases are an essential part of any modern health service but some are significant greenhouse gases. The Scottish Government and NHS Scotland are working together to reduce their climate impact. In 2023, Green Anaesthesia Scotland won the inaugural European Sustainable Healthcare Project of the Year from Health Care Without Harm and the Sustainability Award at the Scottish Public Service Awards.
Volatile Anaesthetics
In 2017/18, volatile anaesthetic gases made up over 10,000 tCO2e of NHS Scotland’s annual emissions. By 2022/23, this had fallen to less than 1,400 tCO2e.
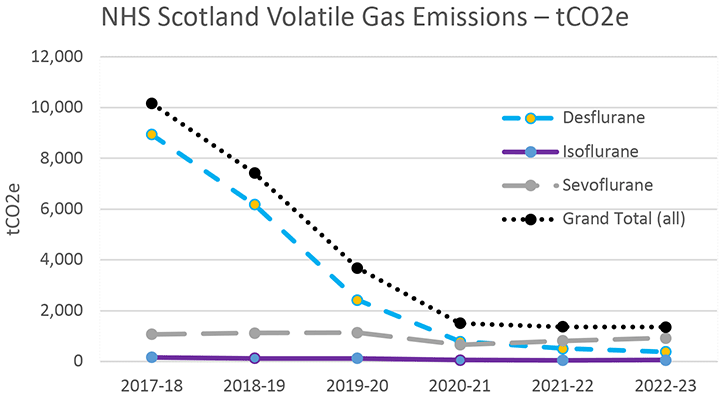
Data source: Hospital Medicines Utilisation Database (HMUD), Public Health Scotland (PHS)
Most of the decrease is due to the reduction in the use of desflurane, a greenhouse gas with a very high global warming potential. Desflurane is more expensive than the alternative volatiles with a lower global warming potential, and you need three times as much to achieve effective anaesthesia, so the switch has saved money for NHS Scotland. The adoption of low-flow anaesthetic techniques has also contributed to the decrease in emissions.
The use of desflurane is now so low that it is no longer be procured nationally by NHS National Services Scotland. Health Boards can still purchase desflurane directly themselves, where required.
Volatile Capture technology is presently being reviewed by the Scottish Health Technologies Group to understand the value it confers in light of now lower emissions of sevoflurane a climate pollutant with a short atmospheric life.
Nitrous Oxide and Entonox
Nitrous oxide is an ozone depleting substance and a potent greenhouse gas with a 100-year global warming potential of 298 times that of carbon dioxide. It is used in general anaesthesia and for pain relief (in combination with oxygen, under the brand name Entonox, commonly known as “gas and air”). It is an important source of pain relief, and particularly important for pain management in maternity services.
Nitrous oxide emissions are largely caused by leaks from piped medical gas systems. Its use as an anaesthetic agent is limited mostly to dentistry, obstetric emergencies, and paediatric gas inductions. Efforts to date focus on minimising system loss. Many piped supply systems have been found to be redundant and often a smaller portable supply will suffice.
Nitrous Oxide
Annual emissions for anaesthetic N2O have fallen by 3,884 tCO2e (37% over the past six years up to, and including, 2023/24). The table below sets out N2O emissions by Health Board for the baseline year (2018/19) against the last two years of available data with a percentage rating which takes account changes since the baseline. As can be seen there is significant variation in performance by Health Board, although for Scotland as a whole the trend in emissions is downward.
| Health Board | 2018-19 (Baseline) | 2022-23 | 2023-24 | Percentage change from baseline |
|---|---|---|---|---|
| National Waiting Times Centre | 190 | 60 | 52 | -73 |
| NHS Ayrshire & Arran | 544 | 284 | 335 | -38% |
| NHS Borders | 253 | 257 | 45 | -82% |
| NHS Dumfries & Galloway | 251 | 103 | 191 | -24% |
| NHS Fife | 315 | 326 | 433 | +37% |
| NHS Forth Valley | 285 | 502 | 51 | -82% |
| NHS Grampian | 1,682 | 1,399 | 981 | -42% |
| NHS Greater Glasgow & Clyde | 2,576 | 2,105 | 1820 | -29% |
| NHS Highland | 444 | 226 | 203 | -54% |
| NHS Lanarkshire | 807 | 345 | 395 | -51% |
| NHS Lothian | 1,959 | 771 | 713 | -64% |
| NHS Orkney | 34 | 15 | 15 | -56% |
| NHS Shetland | 33 | 83 | 11 | -67 |
| NHS Tayside | 940 | 884 | 1188 | +26% |
| NHS Western Isles | 63 | 114 | 59 | -6% |
| Grand Total | 10,375 | 7,474 | 6,491 | -37% |
To the best of the Scottish Government’s knowledge, by February 2024:
a) 35 N2O piped systems had been decommissioned or minimised;
b) 12 systems were scheduled for decommissioning;
c) 12 high emitting hospitals have not submitted N2O minimisation plans; and
d) 21 systems require investigation.
Three key concerns have been highlighted to clinical, pharmacy and facilities teams:
1. Cylinders should be used until depleted including manifold stocks;
2. Oversupply of this agent should be avoided; and
3. Excellent security and monitoring need to be in place as this is a recreational drug.
Entonox
Entonox accounted for 16,579 tCO2e in 2023/24 making it the largest source of medical gas emissions in NHS Scotland. Unlike N2O for general anaesthesia, Entonox continues to be commonly used for pain relief. NHS Scotland aims to ensure that Entonox is available for pain relief while also minimising the gas which escapes to the atmosphere.
Initial analysis at a hospital level shows wide variation in the Entonox emissions per maternity from 14,056 kgCO2e (an outlier) to 200 kgCO2e with a national average of 287 kg CO2e.
A promising start was made in 2023/24 to mitigating Entonox emissions. While it is still too soon to draw definite conclusions, we know that midwifery and facilities teams across Scotland are taking steps to reduce gas loss from delivery systems and that emissions were 7% lower in 2023/24 than the previous year.
A technical brief on Entonox mitigation has been issued by the Scottish Government and is available here: https://www.publications.scot.nhs.uk/publication/7937
The following table sets out changes in Entonox uses since the baseline year of 2018/19.
| Health Board | 2018-19 (Baseline) | 2022-23 | 2023-24 | Percentage change from baseline |
|---|---|---|---|---|
| National Waiting Times Centre | 2 | 45 | 81 | +3950% |
| NHS Ayrshire & Arran | 800 | 632 | 681 | -15% |
| NHS Borders | 379 | 292 | 186 | -51% |
| NHS Dumfries & Galloway | 471 | 384 | 310 | -34% |
| NHS Fife | 1,177 | 971 | 939 | -20% |
| NHS Forth Valley | 914 | 837 | 651 | -29% |
| NHS Grampian | 2,430 | 2,624 | 2,005 | -17% |
| NHS Greater Glasgow & Clyde | 3,872 | 3,605 | 3,694 | -5% |
| NHS Highland | 747 | 676 | 743 | 0% |
| NHS Lanarkshire | 1,602 | 1,462 | 1,465 | -9% |
| NHS Lothian | 2,649 | 3,316 | 2,809 | +6% |
| NHS Orkney | 57 | 71 | 77 | +35% |
| NHS Shetland | 81 | 72 | 41 | -49% |
| NHS Tayside | 1,318 | 1,535 | 1,555 | +18% |
| NHS Western Isles | 64 | 55 | 69 | +8% |
| Scottish Ambulance Service | 1,336 | 1,277 | 1,272 | -5% |
| Grand Total | 17,899 | 17,851 | 16,579 | -7% |
National Green Theatres Programme
The National Green Theatres Programme (NGTP) was formally launched in March 2023 and aims to reduce the carbon footprint of clinical theatres across NHS Scotland. The carbon saving actions from NGTP demonstrate that positive changes are achievable in terms of the products and items that are used. Key elements are:
- Working with clinicians, subject matter experts and professionals to develop realistic actions that reduce carbon emissions; and
- Supporting Health Boards to implement, measure and report on these improvements.
Informed by the learning from NHS Highland’s Green Theatre Project, NGTP aims to develop and spread actions that can reduce carbon emissions across a number of areas.
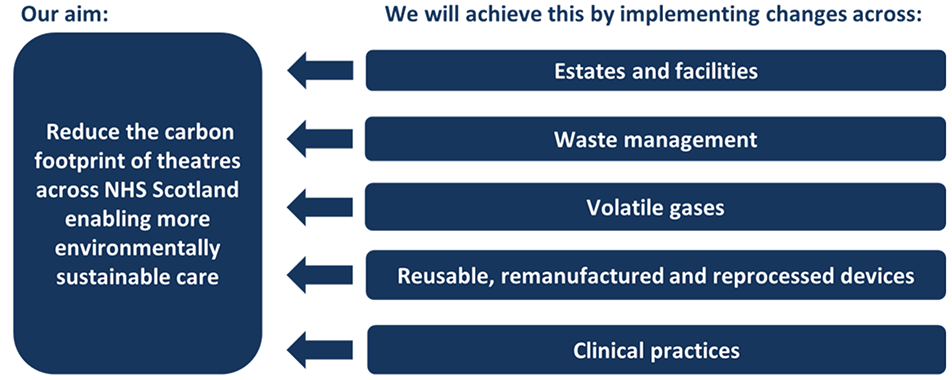
The programme is underpinned by a co-design approach, focussed on working with clinicians, subject matter experts and national partners to share learning and best practice and design solutions.
NGTP has developed two types of “Carbon Saving Actions” - “Actions for Implementation” and “Actions for Adoption”.
Actions for Implementation
Actions for implementation are carbon saving actions which Health Boards are being supported to implement with requirements to validate and report on improvements throughout the programme.
Potential opportunities per annum equate to annual savings of 20,422 tonnes of tCO2e and £5.8 million of cash[4]. The following table shows the main savings that could be achieved.
| Carbon Saving Actions | Carbon Saving Opportunity (tCO2e per annum) | Case Saving Opportunity (£ per annum) |
|---|---|---|
| Switch off out of hours Heating Ventilation Air Conditioning (HVAC | 6,692 | 3,932,500 |
| Decommissioning of Nitrous Oxide (N2O) manifolds | 6,486 | 0* |
| Removing Desflurane liquid | 6,421 | 834,249 |
| Embed waste segregation | 353 | 473,809 |
| Automated switch off out of hours of Anaesthetic Gases Scavenging Systems (AGSS) | 232 | 270,509 |
| Embed Rubbing not Scrubbing | 133 | 40,959 |
| Installation and implementation of alternative surgical fluid collection and disposal system | 75 | 0* |
| Change peri-operative paracetamol from intravenous to oral | 38 | 53,079 |
| Rationalising fluid giving sets and warming devices | 12 | 257,070 |
| Total | 20,442 | 5,862,175 |
*Cash saving have not been provided, these may be updated in the future subject to availability of information.
Actions for Adoption Actions for adoption are to raise awareness of other carbon saving actions that can contribute to reducing carbon emissions. These are actions that may be: progressed through other national work streams and, or may be difficult to measure. Health Boards are encouraged to consider how they are adopting these actions. They are as follows:
- Embed telephone and video clinics, reducing carbon footprint from staff travel, particularly in rural areas, where public transport options are limited;
- Enable active transport, which can improve mental and physical wellbeing for patients and staff as well lowering the carbon cost; and
- Introduce cold metal sticks to replace Ethyl Chloride spray to test for sensory function in regional anaesthesia.
Year Two
In its second year, the NGTP will continue to develop actions for implementation and actions for adoption whilst supporting Boards to make improvements relating to theatres. It will also look at how it can work more closely with circular economy principles, and opportunities for the introduction of reusable devices and textiles as well as the reprocessing and remanufacturing of items.
Waste, Procurement, and Circular Economy
Waste doesn’t just represent used products which need to be removed, but money left on the table and emissions left in the system. To manage waste effectively requires embracing the circular economy, changing processes, re-using where possible and recycling where that is not possible. It involves changing procurement processes to ensure sustainability and re-use, and ultimately, monetary value going back into the NHS. It is at the heart of all our investment decisions.
Waste
In 2023-2024, the focus has been on securing data on waste, undertaking a gap analysis and building sustainability requirements into waste management service contracts. A baseline review was undertaken by the Resource Management Association Scotland (RMAS) of Health Board waste management performance in relation to the 2025 waste targets originating from The Waste (Scotland) Regulations 2012. In summary, ahead of the 2025 target year.
- Six territorial Health Boards have achieved reductions in their general waste of 15%;
- 12 territorial Health Boards now send less than 5% of their general waste to landfill; and
- Six territorial Health Boards have reduced their food waste by 33%.
NHS Scotland has made strong progress on reducing food waste, with almost half of all boards meeting the 33% reduction in food waste target before the 2025 deadline. The management of food waste is a critical component of a health board’s net zero strategy and through the NHS Scotland Catering Services Expert Group, all boards are being supported to collect data and put in place regional and local food waste solutions.
Twelve Health Boards have met the 2025 target on diversion from landfill. The new national waste framework contract, (which came into effect 01 April 2024), should support further change but there remains real challenge in some rural and island Health Boards, where compliance may be limited by local waste management options.
Across Scotland, Health Boards have struggled to meet the 70% recycling target, with a huge range in performance reflecting the scale of challenges we face. Recycling performance in NHS Scotland ranges from 19% to 61%, with an average rate of 34%. NHS Assure, working with Health Boards, RMAS and Zero Waste Scotland have created Waste Route Maps for each geographic board to help with progress. As part of the Health Board Waste Management Route Maps, guidance was provided with respect to competency and staff numbers required to effectively manage waste on NHS sites.
| Reduce general waste by 15% by 2025 | No more than 5% of general waste to landfill by 2025 | Reduce food waste by 33% by 2025 | 2023 Recycling Rate | |
|---|---|---|---|---|
| NHS Ayrshire and Arran | Met | Met | Met | 26% |
| NHS Borders | Not met | Met | Insufficient data | 41% |
| NHS Dumfries and Galloway | Not met | Met | Not met | 36% |
| NHS Fife | Not met | Met | Not met | 40% |
| NHS Forth Valley | Met | Met | Insufficient data | 23% |
| NHS Grampian | Met | Met | Met | 44% |
| NHS Greater Glasgow and Clyde | Not met | Met | Met | 19% |
| NHS Highland | Met | Not met | Met | 37% |
| NHS Lanarkshire | Met | Met | Met | 61% |
| NHS Lothian | Not met | Met | Met | 23% |
| NHS Orkney | Insufficient data | Met | Insufficient data | Lacking data |
| NHS Shetland | Insufficient data | Met | Insufficient data | Lacking data |
| NHS Tayside | Not met | Met | Not met | 38% |
| NHS Western Isles | Met | Not met | Insufficient data | 22% |
Examples of Good Practice
In 2023-2024, as part of the NHS Scotland Circular Economy Programme, work was undertaken with a number of Health Boards to identify opportunities to increase both the quantity and quality of recycling.
NHS Tayside: Plastics Recycling
An 8-week trial was undertaken by NHS Tayside at Ninewells Hospital. This trial focused on the collection of high-quality plastic waste from four clinical areas. The plastic collected was non-infectious and was not contaminated. It was therefore suitable for recycling without any pre-treatment. NHS Tayside sought to identify the viability of source segregation of plastic in clinical areas and to gain an understanding of the value of the material collected. The trial focused on high quality products and packaging, those made from two types of high-grade plastics: HDPE (High-density polyethylene), PP (Polypropylene) and PET (Polyethylene terephthalate). These high-quality plastics are readily recyclable with high market demand and represent lost financial value in the economy.
The trial was successful. A significant volume of plastic was collected, and feedback from the clinical staff was positive, with the teams involved requesting to keep the plastic collection in place. In particular, the role of the Board’s Waste Management Officer was a crucial one. Providing clear instructions, supporting these with poster campaigns and colour coded bins was essential, making it as easy as possible for staff to recycle effectively. While the trial came at zero additional cost to the NHS, the data from the trial suggests that the quality of plastic is such that a rebate on collection will be likely for Health Boards.
The results of the trial demonstrated both the economic and environmental impact of high-quality plastic segregation. This trial fed into the development of the Waste Route Maps for each board and informed the new national waste framework contract (which went live from April 2024). Guidance is currently being produced by NHS Assure, to be implemented by boards, to ensure metrics and reporting will be in place to track financial and carbon savings.



NHS Highland: Paper Towels
Paper towels may not seem like a widespread commodity within hospitals, but they represent around 17% of waste sent to landfill in the NHS (by weight). This was identified as part of the work on Waste Route Maps. NHS Assure supported Portering Leads at NHS Highland to segregate paper towels and develop this as a separate waste stream. This was collected by a local contractor, Northern Recycling, and mixed with the collection of food waste on site, processed by Keenan Recycling. Contamination levels were found to be minimal, with the majority of segregated material suitable for composting.

Both projects have resulted in the national waste framework contract including these items to be collected separately.
Procurement
Medicines, medical equipment and other elements of NHS supply form around 62% of carbon emissions generated by the NHS per activity area. As part of our work to make the NHS net zero, it is vital that environmental sustainability forms a part of procurement considerations and that we work with suppliers to encourage them to develop more environmentally sustainable products and supply chains.
NHS National Procurement has been reviewing their suppliers’ Net Zero Plans to understand supply chain aspirations for net zero for their key healthcare products. They have focussed on suppliers with the highest annual spend and have identified 121 suppliers who have a Net Zero Plan in place. This covers £1.01bn and 77.5% of spend. Utilising input from NHS England’s Evergreen system and market investigation, net zero dates for these suppliers have been incorporated into an interactive dashboard where NHS procurement staff can view them.
National Procurement are collaborating with the other NHS and healthcare partners in England, Wales, and Northern Ireland to align practices and approaches to supplier engagement.
Sustainable Construction and Demolition
The overall impact of the Healthcare Built Environment on the net zero targets for NHS Scotland is significant and it is therefore critical that greenhouse gas emissions are reduced to as close to zero as possible within our estate. There is a challenge in realising that position whilst maintaining the myriad of competing requirements in such a complex built environment, and there is a lack of data to determine what that position looks like.
To help make improvements to future updates of the Sustainable Design and Construction Guide (SHTN 02-01), and provide more detailed guidance on how to achieve net zero in healthcare, NHS Scotland Assure have commissioned research to determine ‘What Good Looks Like’ with a specific focus on:
- reducing overall energy use demand within differing areas of construction;
- viable Zero Direct Emissions Heating solutions for the healthcare estate;
- limiting the amount of embodied carbon in healthcare construction; and
- increasing circularity in healthcare construction.
The research will be based on current best practice healthcare environments, and it is expected that outputs will help inform an update to the Sustainable Design and Construction Guide during 2024-2025.
Greenspace and Biodiversity
NHS Scotland is a custodian of significant areas of greenspace. Improving NHS Scotland greenspace is a low-cost way to develop healthy environments at the heart of communities, to help mitigate against predicted climate change effects such as summer heatwaves and increased rainfall in winter[5].
Grasslands Management
Since the 1950s, 97% of the UK wildflower meadows have been lost, which has had a detrimental effect on the variety of plants, mammals, invertebrates, and fungi that depend upon them. In February 2024, a report was published by NHS Scotland Assure to support Health Boards to improve the management of their grassland areas and create wildflower meadows. The approach set out in the report can have the following benefits:
- Supports the creation of diverse habitats.
- Supports pollinators such as bees.
- Reduces flood risk.
- Can result in cost savings.
The report is available here: Grassland Management Report, February 2024

Greenspace Project Funding
The Scottish Government provides an annual budget of £300K each year for NHS Scotland greenspace projects. The money has been used to support projects which directly or indirectly support biodiversity while also benefitting staff, patients, and local communities. For 2023-2024 money was allocated to support the following projects:
- Supporting use of, and access to, greenspace at Queen Margaret Hospital within NHS Fife, alongside a habitat survey and actions to improve biodiversity;
- At Stirling Health Care Village within Forth Valley, supporting biodiversity, improving access to greenspace, and improving the quality of the greenspace;
- Within NHS Highland, at Raigmore Hospital, design and planning to further support greenspace, biodiversity and connections to wider areas. This includes professional design input and a whole campus habitat survey; and
- At Ninewells Hospital within NHS Tayside, work to progress the design of a 24-hour accessible Neonatal courtyard garden for parents/staff.
Digital National Mapping of the NHS Estate
The NHS Scotland outdoor estate has been mapped using a tool developed by Public Health Scotland. This tool has different applications such as providing a visual map of flooding risk and opportunities for siting solar panels or wind turbines. Work is underway to fill in the digital map with the habitat types within the NHS estate. This is to help ensure that the best use can be made of the estate for reducing greenhouse gas emissions, making the NHS more resilient to adverse weather, improving biodiversity, enhancing the experience of the sites for staff, patients, visitors, and members of the local community.
Contact
Email: christopher.bierley@gov.scot
There is a problem
Thanks for your feedback