Draft: Birthplace Decisions, Information for pregnant women and partners on planning where to give birth
This is a draft document, which we are currently seeking your views on.
What does the evidence show about births in different settings?
You may wish to discuss what the evidence shows us about the risks and benefits of births in different settings with your midwife when discussing your birth choices.
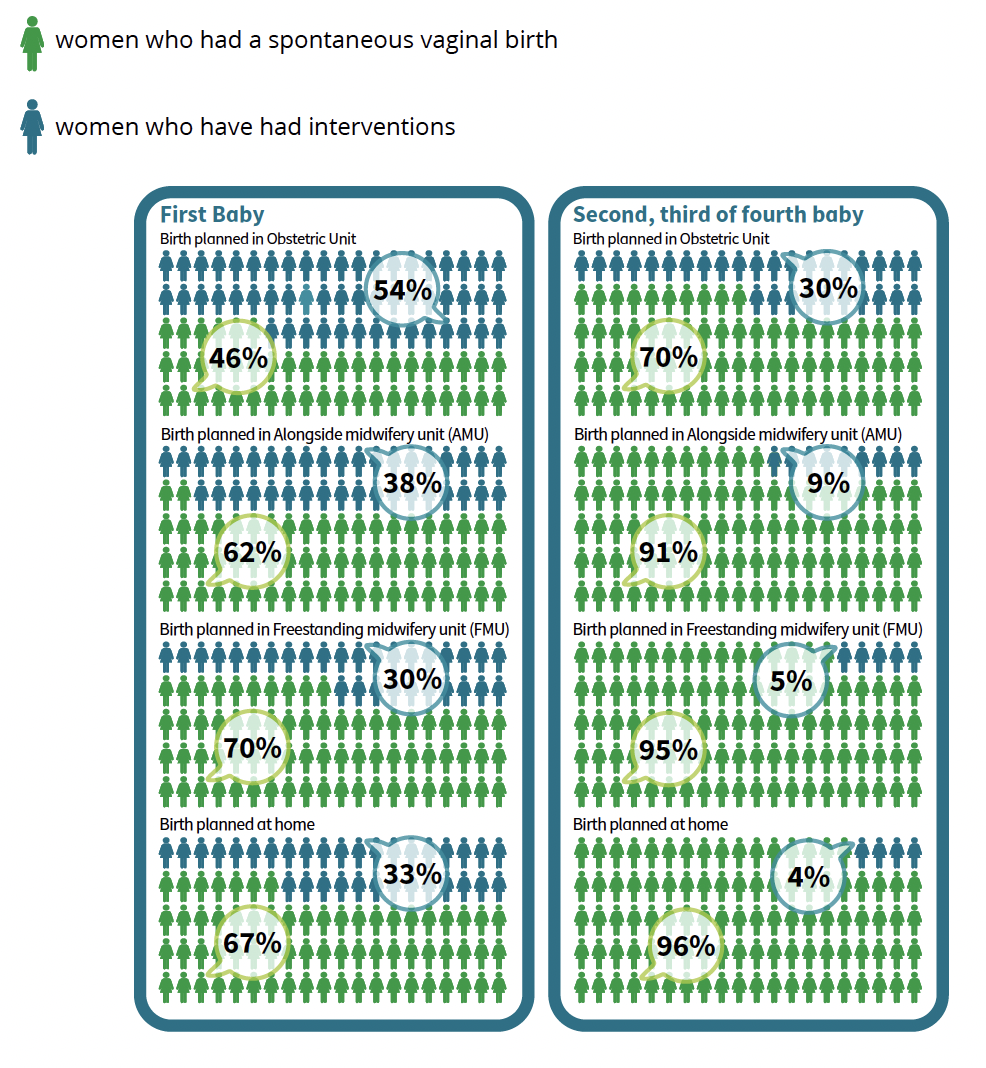
Birth is generally very safe for women at low risk of complications and their babies. The diagrams below show outcomes for women and their babies when birth is planned in different settings. The diagrams refer to healthy women at low risk of complications.
Spontaneous Vaginal Birth
Spontaneous vaginal birth means that you go into labour by yourself (labour is ‘spontaneous’), and give birth without assistance from instruments (ventouse or ‘vacuum’ birth, or forceps), without Caesarean and without general, spinal or epidural anaesthetic before or after birth.
What are the chances I will have a spontaneous vaginal birth in each birth setting?
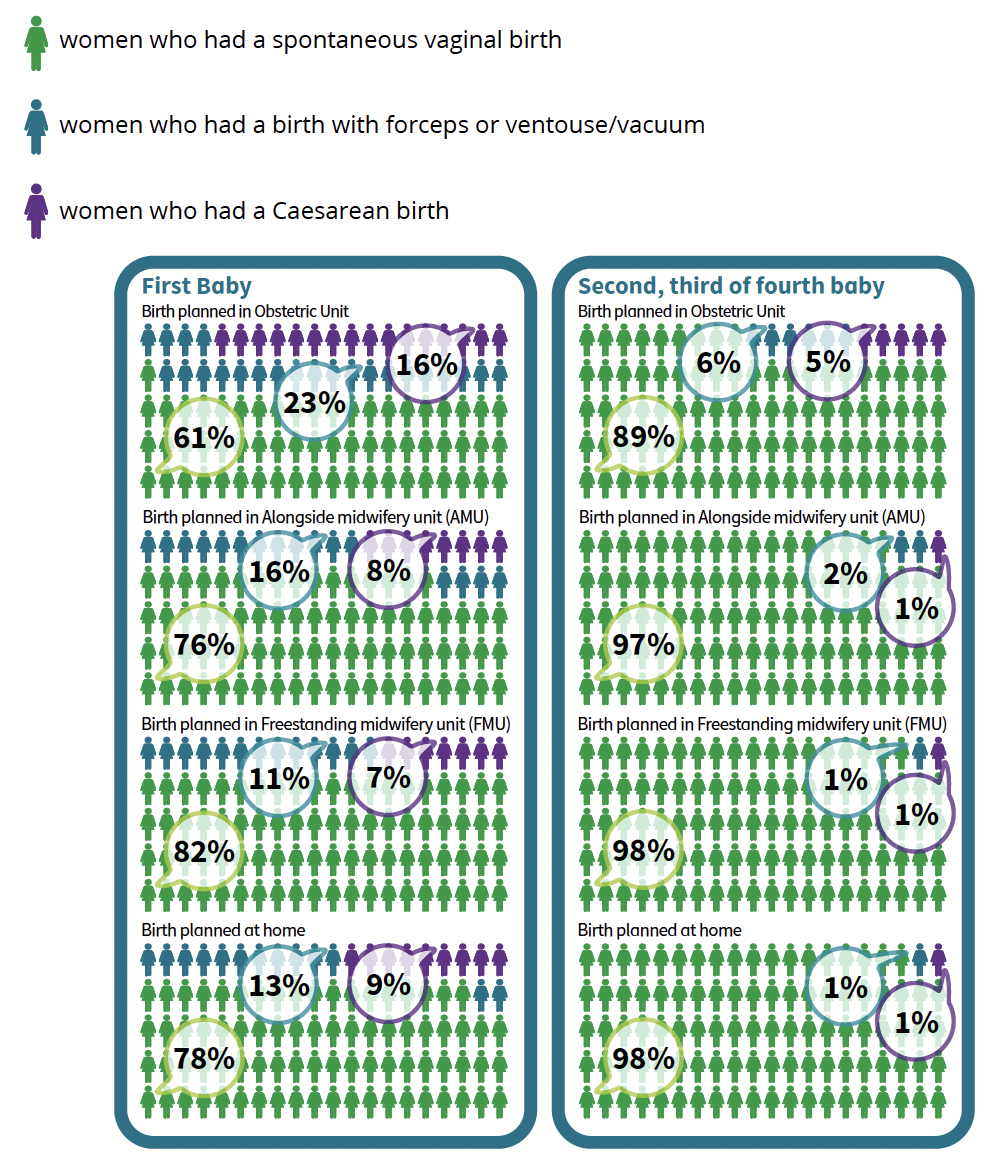
Birth with Forceps
Birth with forceps and emergency Caesarean birth, ventouse or ‘vacuum’, and forceps, are sometimes needed to help deliver the baby.
Like Caesarean births, births with forceps are more common amongst women having their first baby, compared to women having their second or subsequent baby. In some cases, the use of instruments is not successful, and then a Caesarean birth is performed.
What kind of birth can I expect to have?
Birth is generally very safe for women at low risk of complications and their babies. These diagrams show outcomes for babies when birth is planned in different settings.
Poor outcomes are rare, but can happen in any setting.
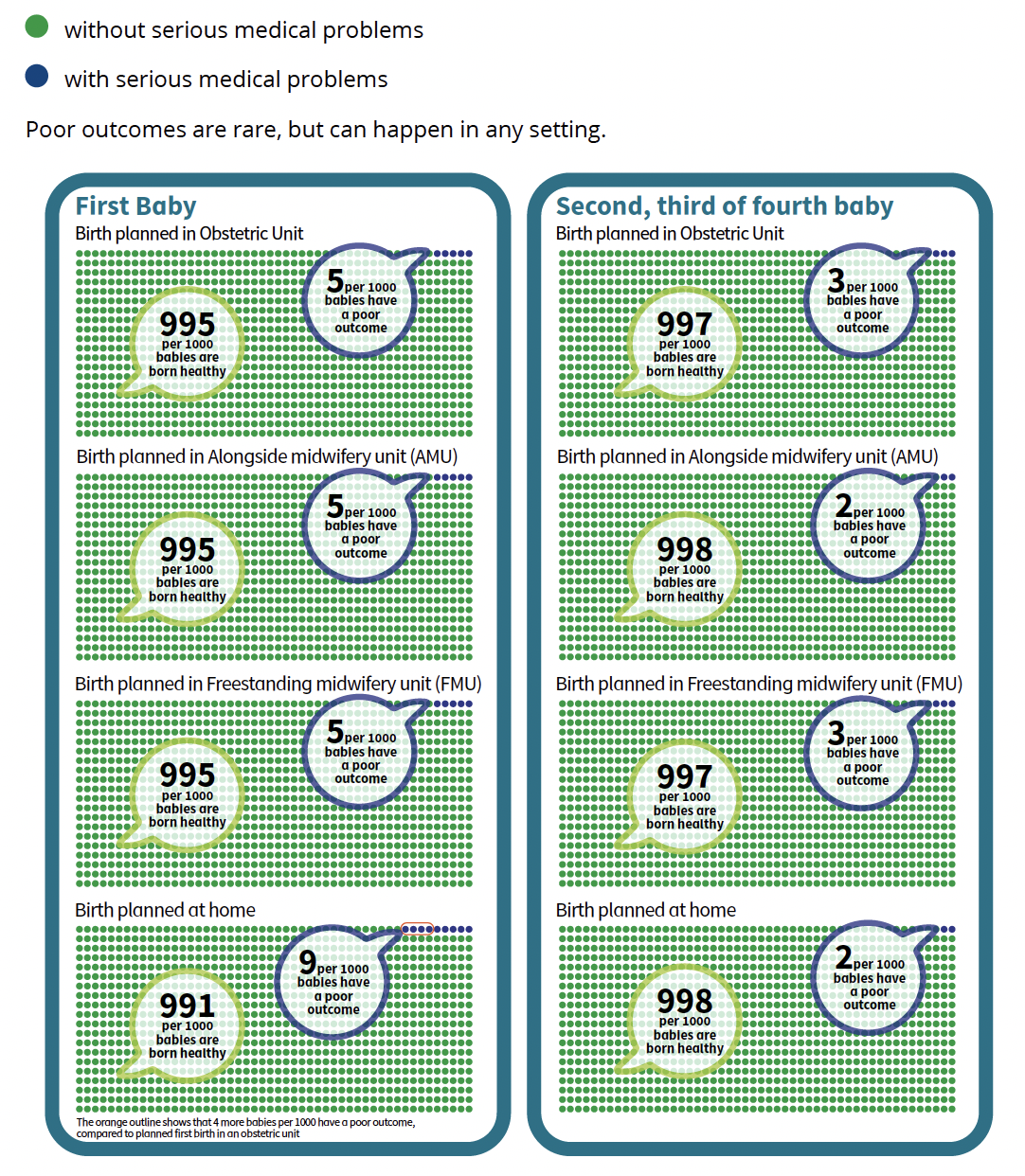
These tables are taken from the King’s College “Birth Place Decisions” leaflet, with data from the Birthplace in England Research Programme
Contact
Email: thebeststart@gov.scot
There is a problem
Thanks for your feedback