Cancer strategy 2023 to 2033
This Cancer strategy for Scotland sets out our vision for the next ten years to improve cancer survival and provide excellent, equitably accessible care. It was developed in collaboration with people with lived experience and our wider partners.
3. Strategy Ambitions
3.1 Our Strategic Priorities
Our strategy will strengthen core elements of the cancer pathway while focussing on cross-cutting issues that will enable success. It will reflect value-based and Realistic Medicine, putting the person affected by cancer at the heart of our approach.
We aim to reduce inequalities across all our ambitions, strive for consistency through a Once for Scotland approach where appropriate, and ensure services are sustainable (in programmes, environmentally, and in resourcing).
The strategy aims to anticipate and reflect the changes over the next 10 years expected in cancer incidence, most common types, treatment options including more precision medicine (where treatment reflects people’s genes), and how our health systems diagnose and treat cancer.
We will focus on cancer types that are the largest burden and have worse outcomes. These include lung and other less-survivable cancers (brain, liver, oesophagus, pancreas, stomach) that have seen very little progress in the last five decades. Lung cancer remains Scotland’s single biggest cause of cancer mortality and continued focus and action to address this are paramount.
A focus on lung cancer
Lung cancer is the single biggest cause of cancer mortality in Scotland and will require the focus applied to it in the National Cancer Plan 2020 to continue with vigour in the long term. Improved survival will require leadership, prioritisation, resourcing and strong action. The required actions will be set out in each action plan accompanying this strategy and include preventative measures such as smoking cessation services and robust tobacco control; earlier and faster diagnosis, including targeted screening and delivering Scotland’s optimal diagnostic pathway; access to specialist treatment; and ongoing research, investment in innovation and further data and intelligence gathering.
3.2 Our Strategic Aims
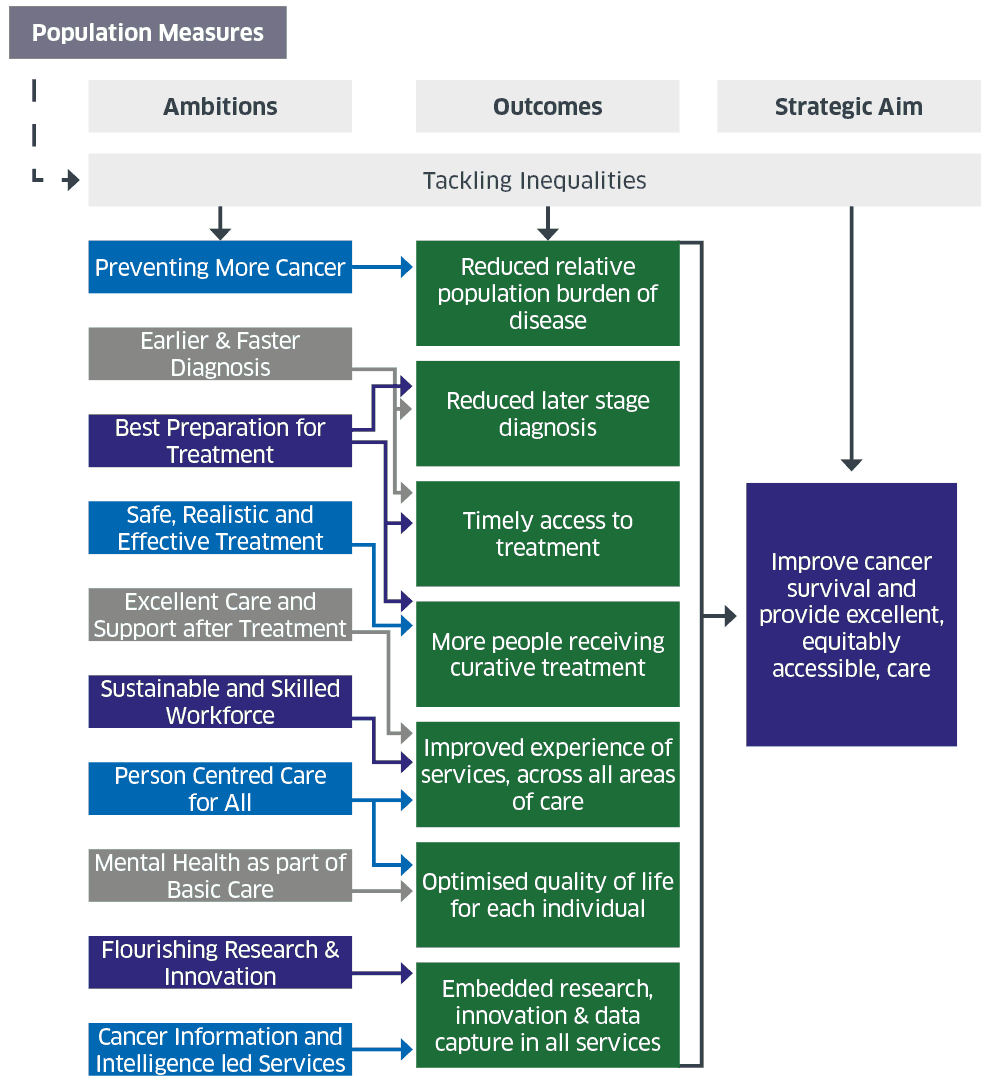
To meet our strategic aim of improved cancer survival and providing excellent, equitably accessible care, we have set out eleven ambitions addressing both cross-cutting and cancer pathway priorities, describing our 10-year vision for each. Our eleven priority ambitions are presented without hierarchy:
Pathway
1. Preventing More Cancers
2. Earlier and Faster Diagnosis
3. Best Preparation for Treatment
4. Safe, Realistic and Effective
5. Excellent Care and Support after Treatment
cross-cutting
6. Sustainable and Skilled Workforce
7. Person-Centred Care for All
8. Tackling Inequalities
9. Mental Health as part of Basic Care
10. Flourishing Research and Innovation
11. Cancer Information and Intelligence-led Services
These ambitions relate to our vision and intended outcomes as follows (recognising that the relationship amongst the elements is far more complex than can be displayed in a diagram and that a number of elements are interconnected):
In addition to an ambition on Cancer Information and Intelligence-led Services, under every other ambition we have included a box on ‘Data for Success’. These are not intended to be comprehensive but to highlight the
importance of data in determining priorities and in monitoring the implementation and outcomes of our ambitions and actions, including where we would like to do more such as addressing inequalities.
3.3 Our Strategic Ambitions
Ambition 1: Preventing More Cancers
Our 10-year vision
Scotland is a place where the new generation of young people do not want to smoke. It is a place where everyone eats well and has a healthy weight, underpinned by a population that is more physically active. Alcohol is no longer a major cause of cancer. The incidence of preventable cancers, such as cervical cancer, is reduced.
This means that:
- We live in a Tobacco-Free Scotland, reducing smoking rates to below 5% by 2034
- We live in a Scotland where more people are more active more often, in line with our Active Scotland Outcomes Framework
- Diet-related health inequalities are significantly reduced, supported by the actions in our 2018 Diet and Healthy Weight Delivery Plan, including legislation to restrict promotions of less healthy food and drink at the point of sale
- People have better informed health-seeking behaviour (know how, when and where to seek help)
- High HPV vaccination coverage is maintained for girls and boys.
Successful implementation of evidence-based prevention strategies targeted at harmful health behaviours could prevent approximately 40% of cancers. Based on these estimates, around 13,000 Scotland cancer cases could be prevented each year.[13]
- Smoking is the most significant cause of preventable cancer in Scotland (18%).[14]
- Obesity is linked to around 2,200 cases of cancer a year in Scotland. Maintaining a healthy weight reduces the risk of 13 types of cancer, including breast, bowel and liver.[15]
- Physical activity is beneficial for the prevention of some cancers including breast, colon, endometrial, kidney, bladder, oesophageal, and stomach. Decreasing time spent sedentary may also lower the risk of endometrial, colon, and lung cancers. Physical activity before and after a diagnosis of breast, colorectal and prostate cancer is beneficial for survival outcomes.[16]
- There is a clear relationship between alcohol consumption and increased risk of developing certain cancers: in 2015, approximately 6.5% of deaths were attributable to alcohol consumption: 28% of these were from cancer.[17]
- There is strong evidence that physical activity before, during and after cancer treatment can reduce anxiety, depressive symptoms and fatigue, and improve health-related quality of life and physical function.
Reducing these risks, and their contribution to inequalities in cancer incidence, is being addressed through strategies and plans such as the Tobacco Control Action Plan (2018), (with a new one due to be published in 2023), the Diet and Healthy Weight Delivery Plan (2018) including support for families to make healthier choices; the Active Scotland Delivery Plan that supports work to reduce the risk of cancer and contributes to prehabilitation and rehabilitation; and the Alcohol Framework 2018 that guides actions to reduce alcohol consumption, including increasing awareness of the link between alcohol and cancer.
Skin cancer is one of the most common cancers in the world. Excluding non-melanoma skin cancers (which are more common), malignant melanoma is the 5th most common cancer in Scotland with increasing rates, particularly in males.[18] Exposure to ultraviolet light from the sun is thought to cause most melanomas and non-melanoma skin cancer.[19] Prevention is through reducing exposure to ultraviolet light from the sun, artificial tanning sunbeds and sunlamps.
Primary cancer-specific prevention strategies include human papilloma virus (HPV) vaccination. HPV vaccination policy is based on recommendations from the Joint Committee on Vaccination and Immunisation (JCVI) and is being offered in Scotland to all girls and boys in the first year of secondary school. Evidence from England is that the vaccine reduces cervical cancer incidence by almost 90% in those who were vaccinated aged 12 to 13.[20] In Scotland, this equates to the prevention of around 450 cervical cancers and around 17,200 cases of precancerous conditions over an 11-year period.[21]
Secondary prevention of cancer means the early detection and treatment of disease before signs and symptoms are apparent – see also ‘Optimise Screening’ under Earlier and Faster Diagnosis Ambition.
Data for success
We will interpret health behaviour surveys and use data to better understand public health interventions that are likely to reduce cancer risks.
Ambition 2: Earlier And Faster Diagnosis
Our 10-year vision
Later stage disease (stages III and IV) has reduced by 18 percentage points. A focus will remain on reducing the health inequality gap, particularly those from areas of deprivation.
Beyond preventing cancers, earlier and faster diagnosis plays the most fundamental role in cancer control. It is vital to further improve cancer survival rates in Scotland which, despite progress in the last 10 years, continue to lag behind international counterparts. This is particularly important for less survivable cancers. Those from areas of deprivation are often more likely to be diagnosed with cancer, particularly at a later stage, and are less likely to take part in screening when invited.
Currently around 42% of cancers are diagnosed at stage III and IV in Scotland, with variation amongst cancer types and socioeconomic groups.[22] Realising our vision would mean that 24% of cancers were diagnosed at stage III and IV in year 10. Based on the latest data available at the time of publication, this would mean around 5000 fewer people in Scotland diagnosed with later stage disease in year 10.
It is recognised that not all cancers can be conventionally staged so additional measurements, such as emergency presentations, will be required to track progress and improvements in other cancer types, including blood and neurological cancers.
There are challenges in meeting the two current cancer waiting times (CWT) standards in NHS Scotland. Latest published data (Q4 2022) show that 72% of people with cancer received first treatment within 62 days of an urgent suspicion of cancer (USC) referral, and 94% received first treatment within 31 days of a decision to treat being made.
We are now treating 36% more patients on the 62-day pathway than 10 years ago (4262 in Q4 2022 compared to 3144 in Q4 2012), and 18% more on the 31-day pathway (6757 in Q4 2022 compared to 5711 in Q4 2012). Embedding all eight key principles of the Effective Cancer Management: Framework (2021) will remain a priority for health boards’ cancer management teams to diagnose cancer earlier and faster – improving waiting times performance, experience and outcomes for people with cancer.
Our response to the challenge of diagnosing cancer earlier and faster will require action in a range of areas through our national whole systems Detect Cancer Earlier (DCE) Programme, including:
Improve Public Education and Empowerment: Raise awareness of possible signs, symptoms and risk factors of cancer – tumour site and non-specific – to empower people to seek help in a timely manner. Break down engrained behaviours and attitudes including fear of cancer that can often act as a barrier to earlier diagnosis, with a focus on reducing the health inequality gap.
Support Primary Care: Primary care plays a pivotal role in the diagnosis of cancer. The vast majority of people with cancer will develop symptoms prior to diagnosis so it is imperative to continue to support primary care clinicians in identifying and appropriately referring those with a suspicion of cancer. That support must highlight the role of socio-economic and health inequalities in cancer and the implications of unmet need in relation to earlier diagnosis. Primary care has unique capacity to deliver prevention and early intervention. For example, many recommendations in the primary care Health Inequalities Short-Life Working Group: report (2022) should contribute to earlier and faster diagnosis for those at greatest need, especially by addressing unmet need and earlier, increased engagement with primary care by individuals who otherwise might not seek care and support.
Optimise Screening: Screening will continue to keep up with technological innovation and emerging clinical evidence to ensure the people of Scotland have access to the most effective screening tools possible, including taking forward recommendations from the UK National Screening Committee on targeted lung screening and exploring the use of self-sampling for cervical screening. It will be a responsive, person-centred system that facilitates equality of access and encourages uptake in all groups. To direct and support this work the first Equity in Screening Strategy has been produced by National Screening Oversight in collaboration with NHS and Third Sector partners and sets out a vision to achieve equity for all those eligible for screening. A whole system approach will be taken to ensure that reducing inequalities is recognised by all as a priority. Outcomes will include increased awareness and understanding of screening programmes, with targeted information for under-served groups. Health professionals across the screening programme will have a greater understanding of the reasons for inequalities in the system and effective ways to address them. A strategic approach will be taken to identify, address, and remove barriers to participants across the entire screening pathway. Data collection and presentation around inequalities will be improved, for example through the development of a Screening Intelligence Platform, to help target evidence-based interventions. Robust evaluation of actions will be undertaken to facilitate scaling up of effective interventions.
Enhance Diagnostics: The early diagnosis or exclusion of cancer is essential to reduce anxiety for people with cancer and their families as well as to guide clinical care. This requires timely access to the most appropriate and effective diagnostic tests, both in primary and secondary care. Further innovation and redesign of diagnostic services including diagnostic imaging, endoscopy, PET-CT and pathology will be required to facilitate timely access to tests as well as introducing new, effective diagnostic tests as they emerge. Oversight and governance are undergoing redesign with the planned launch of a Diagnostic Strategic Network, which will provide the strategic direction to ensure diagnostic services are equipped to support the recovery efforts and person-centred, sustainable and innovative future delivery. Ongoing delivery of the Endoscopy and Urology Diagnostic Recovery and Renewal Plan (2022) remains a priority.
Harness Data: Continuous improvement in the provision of timely, high-quality, transparent, and integrated data will enable an improved understanding of barriers to earlier diagnosis and variation (geographical, socio-economic, ethnicity and other equalities data). This includes having more timely staging data available for all stageable cancer types.
Invest in Innovation: Research and innovation have a key role to play in improving earlier diagnosis rates, such as biomarkers (including volatiles), artificial intelligence and multi-cancer early detection tests (MCEDs). Identifying promising research and developing a pipeline that enables innovations to be brought into NHS Scotland, to help diagnose cancer earlier and faster, will ensure improvements can be rolled out and embedded at pace. This will be supported by Chief Scientist Office and the SHIP, including the Cancer Innovation Consortium and the ANIA Pathway, and will require coordination across multiple partners, including industry and academia.
Data for success
We will measure progress through a number of sources, ensuring the inequality gap is narrowed throughout, including:
- Number of cancers diagnosed through unwarranted emergency presentations
- Cancer waiting times publications
- Independent qualitative data and insight to monitor public understanding of possible signs and symptoms of cancer
- Breakdown by Scottish Index of Multiple Derivation (SIMD) where possible
The importance of a rapid diagnosis
An interim evaluation of the Rapid Diagnostic Services carried out by the University of Strathclyde found that the one-to-one contact with dedicated healthcare staff and the timeliness of cancer or non-cancer diagnosis are particularly valued. In consequence, overall patient satisfaction with the new service is high. Patient safety and clinical effectiveness (not least in terms of cancers detected) appears to be good.
A user said:
“It was like a whirlwind, not of destruction/confusion, but reassurance and comfort. Everything happened quickly, in a very organised way, giving me confidence that the people who would be caring for me knew what they were doing and would be there for me.”
Ambition 3: Best Preparation For Treatment (“Pre-Treatment”)
Our 10-year vision
Every person diagnosed with cancer in Scotland is provided with timely, effective and individualised care to best prepare them for treatment. This begins with prehabilitation and holistic needs assessment, and continues throughout the individual’s pathway of care, including appropriate follow up. A comprehensive range of cancer genomic tests is available to all those who could benefit.
Pre-treatment encompasses the stage between the point of diagnosis and the initiation of treatment. Additional information and support from the point of suspicion of cancer can improve overall experience, reduce anxiety and, in some instances, positively impact overall outcomes. Shared decision making, holistic needs assessments, information provision and signposting should be considered from the earliest point.
Collaborative working across health, care and third sectors enables early identification and access to the care and support that suits an individual’s needs at the time that is right for them. Our partnership with Macmillan, and “Improving the Cancer Journey” will continue over the next 10 years to achieve future sustainability within the Health and Social Care Partnerships and Local Authorities. This programme alongside other initiatives like the Single Point of Contact optimise collaborative working. We will work with the Scottish Cancer Coalition and other relevant partners to ensure an accessible directory of support services is available for everyone affected by cancer in Scotland.
Prehabilitation prepares people for cancer treatment and includes exercise, nutrition, psychological support, and assistance with alcohol and tobacco reduction/avoidance. It aims to improve quality of life, maximise treatment rates and minimise side effects of treatment. It should be delivered as outlined in the Key Principles – Prehabilitation for Scotland. Holistic needs assessments should be used to identify the concerns that a person with cancer has and to understand their needs. This should inform the development of a personalised care and support plan, that addresses current needs and is anticipatory for the future. That will ensure the right information is shared at the right time, and that people with cancer are signposted to relevant services.
Advances in genomic medicine should also be used to help clinicians deliver precision medicine and ensure that people with cancer receive the most appropriate treatment and avoid unnecessary side-effects. The Scottish Genomic Test Directories already include a range of genetic tests for cancer treatments, with further development of these directories anticipated in the coming years.
Data for success
We will use qualitative and quantitative data to measure experiential, clinical and system-level outcomes.
We will map prehabilitation programmes and develop a minimum dataset.
We will monitor the uptake of the Improving the Cancer Journey initiative and the number of holistic needs assessments conducted.
The Value of Prehabilitation (Prehab)
Having never been to Maggie’s before, Ian was referred by his oncologist before starting his treatment for oesophageal cancer. At that time, he felt a bit anxious and in limbo with regards to treatment, as surgery depended on chemotherapy working well. However, he was glad to receive reliable information about his role in recovery and improving treatment outcomes. As a result, Ian felt more confident managing his physical health, emotional wellbeing, and diet and nutrition. He also found it comforting to hear about another person’s experience – including the ups and downs – of treatment for oesophageal cancer.
Since the prehab workshop, Ian has been back to Maggie’s on multiple occasions, as have several family members who wanted to provide support to Ian and access support...
... for themselves. As Ian is now approaching his surgery, he revisits the information and techniques he’s learned.
“You think, you know, I’m going for an operation here, what do I need to look at specifically for my operation? I need to keep my fitness up. I need my mindset right.”
Of Prehab at Maggie’s, he says: “… It’s quite strange how well Prehab fits with Maggie’s… if you look at the main aspects that come out of the Prehab course in particular, every single one of your learning outcomes is something that’s taught, or supported, or part of the main Maggie’s ethos, in a way. It’s in your curriculum. It’s naturally there.”
Ambition 4: Safe, Realistic And Effective Treatment
Our 10-year vision
All people with cancer have equitable access to treatments, with minimal variation in care. Where someone’s cancer can potentially be cured, they have access to the best available treatment to achieve this. Pathways benefit from new technologies and tests allowing earlier treatment and leading to better outcomes. The Scottish Cancer Network is at the centre of this work, developing national clinical management pathways for all people with cancer.
Safe and effective treatments are critical to improving outcomes for each person with cancer and improving overall quality of life. Cancer care encompasses various treatment methods, broadly surgery, radiotherapy and systemic anti-cancer treatment (SACT) – dependent on an individual’s precise diagnosis. The management of an individual’s cancer may not involve any of these treatments, where that has been decided between the individual and their clinical team.
Surgery remains the single most effective treatment for solid tumour cancers. People requiring cancer surgery are increasingly benefiting from treatment in specialist centres, by teams who frequently perform a particularly complex operation and gain experience and expertise in doing so. We require service providers to collaborate and integrate regionally and nationally to ensure we maximise the potential for the most skilled and knowledgeable surgeons. Evidence shows this approach leads to better clinical outcomes for people with cancer, as well as fewer complications and less time in hospital. People with cancer requiring complex operations are usually very receptive to being treated by highly specialist teams, even where it involves increased travel, but it is crucial that they are appropriately supported in doing so (practically, financially and emotionally as required). Robotic assisted surgery makes significantly smaller incisions than required for traditional surgery, reducing the risk of complications, shortening recovery times and allowing hospitals to treat more patients. This will become routinely available for a wider range of operations throughout Scotland, facilitated by greater integration of services and regional working.
Radiotherapy is received by 40% of all people with cancer who are cured.[23] The National Radiotherapy Plan (2022) outlines 13 key actions to ensure that Scotland continues to have a world-class radiotherapy service. We will continue to roll out advanced treatment, including Stereotactic Ablative Radiotherapy (SABR) to those who would benefit, maximise the potential of Artificial Intelligence (AI) to support treatment planning, and agree national protocols and approaches to hypofractionation. We will continue to assess current evidence on the use of photons and proton beams and develop a long-term view of patient access to proton therapy.
SACT encompasses the treatment of cancer with chemotherapy and immunotherapy drugs. Both have the potential to cure some cancers (and can be used in combination with surgery and radiotherapy to improve outcomes) as well as providing disease and symptom control and extension of survival. Cancer medicines account for the highest proportion of new medicines introduced within NHS Scotland each year, with a fast rate of growth in their availability, a high risk of side effects and associated high costs. The pressure on SACT services to deliver these new medicines continues to increase. The number of patients receiving SACT has seen a steady increase over the last few years. In comparison, the increase in patient appointments has seen an even sharper increase over the same time period.[24]
The Scottish Medicines Consortium (SMC) is the national source of advice on the clinical and cost-effectiveness of all newly licensed medicines for NHS Scotland. The National Cancer Medicines Advisory Group (NCMAG) was established to improve equity of access to safe and effective off-label and off-patent uses of cancer medicines (i.e. used outwith their licence) through provision of national advice for cancer medicines not covered by the remit of the SMC. The work of NCMAG will continue, alongside the SMC, to improve medicines access. Alongside this there will be a renewed focus on SACT services to support sustainable delivery with appropriately increased resource. Allied to SACT delivery, and in order to maximise the opportunities of precision medicine, we aim to offer comprehensive genomic tests to appropriate people with cancer at an earlier stage in their clinical pathway.
The Cancer Medicines Outcome Programme (CMOP) helps assess the ongoing safety, effectiveness and value of cancer medicines (including off-label) in Scotland. Alignment of CMOP with the Scottish Medicines Consortium, National Cancer Medicines Advisory Group and the Scottish Cancer Network will ensure national cancer medicines intelligence informs clinical practice and enhances person-centred care.
There will be an ongoing need for services for people with cancer who develop an acute cancer-related illness presenting in an emergency setting or acute complications from ongoing treatments. The Acute Oncology Service (AOS) in NHS Scotland: Principles (2022) document will guide the development of new models to provide people with cancer requiring emergency care a direct route to cancer services.
Underpinning all cancer treatment is patient safety. All services in the NHS will be delivered in ways that take into account the Scottish Patient Safety Programme and meet the obligations set out under legislation, such as the Patient Rights (Scotland) Act 2011 (legislation.gov.uk) organisational duty of candour.
Data for success
We will continue to measure the number of patients receiving SACT and radiotherapy to monitor workloads, demands and requirements.
We will better measure cancer surgery workload.
We will measure outcomes through patient experience and outcome surveys as well as through the CMOP.
We will better monitor the introduction of new cancer medicines and their impact on the health service to help guide the introduction of new medicines.
We will disaggregate data as much as possible by ethnicity and equality characteristics.
Ambition 5: Excellent Care And Support After Treatment
Our 10-year vision
Personalised support and care post-treatment are core considerations in cancer management pathways: this includes rehabilitation, early detection of recurrence, and supportive and palliative care. People affected by cancer are informed and supported to adequately manage side effects of treatment with the appropriate tools, including an electronic treatment summary.
All individuals requiring rehabilitation have access to meaningful, person-centred rehabilitation that will support
them to live well and support a good quality of life, regardless of their stage on the cancer pathway. Follow-up is standardised in the SCN’s clinical management pathways, is evidence-based for each cancer type and individual (including secondary cancers) and covers patient-initiated requests for review. Every person with cancer in Scotland requiring palliative care receives well-coordinated, timely and high-quality care, including care around death. Bereavement support is provided for families and carers based on their needs and preferences.
Treatment, even with curative intent, is not always the end of care. Some people may need continued support by the NHS and others, including the third sector, to maximise their quality of life. More people are living with cancer, and treatment can cause anticipated side effects and complications that have a significant impact. Supported self-management, rehabilitation, palliative and supportive care are therefore essential, along with consistent approaches to follow up, in line with individuals’ clinical needs.
Good rehabilitation is part of the whole cancer pathway to support individuals to recover or adjust so that they achieve their full potential to live well with cancer. The Once for Scotland Rehabilitation Approach (2022) provides a framework for good rehabilitation that puts the individual at the centre and builds on the concept of Realistic Medicine to provide a personalised approach that is outcomes-focused and supported by a shared decision making process. Rehabilitation includes activities, interventions and information resources that support self-management and facilitate access to services that address growing or complex needs, from as early as possible through to after treatment. Rehabilitation has the potential to maximise quality and quantity of life whilst reducing disease burden.
Palliative care, care around death, bereavement care, and support for carers are integral parts of the cancer journey experienced by people and their families. Palliative care includes anticipatory care planning, early supportive and palliative care in parallel with cancer treatment, symptom management, and specialist palliative care. Palliative care is integrated across health boards, Health and Social Care Partnerships and the third sector, involving primary care, hospitals, hospice care, social care and family support. Our vision for palliative care will be reflected in a new Palliative and End of Life Care Strategy.
The importance of spiritual care and the role of spirituality for health and wellbeing is becoming better understood. Spiritual wellbeing enhances and integrates all other dimensions of health, including physical, mental, emotional and social.
A Cancer Treatment Summary is a document produced by secondary cancer care professionals in collaboration with a person with cancer, for them and their GP practice. It provides information including possible treatment toxicities, side effects and consequences of treatment, signs and symptoms of a recurrence, and any actions for primary care. By co-producing and keeping a copy, the summary is also designed to support patient self-management, guide decision making, improve a sense of control, and reduce anxiety that can be particularly associated with end of treatment.
Collaborative working across health, care and the third sector can enable early identification and access to the care and support that suits an individual’s needs at the time that is right for them. Cancer Patient Experience Surveys (CPES) carried out
in Scotland indicate that this process is not universally experienced, and many feel inadequately supported following treatment. We will optimise collaborative working, meet holistic needs and improve quality of life by embedding rehabilitation and treatment summaries in cancer pathways, regularly re-assessing needs and sharing proactive care planning.
Data for success
We will measure accessibility to a broad range of tailored rehabilitation services that are outcomes-focused and centre on the individual.
We will explore how best to measure quality of palliative care in cancer using validated outcome measures for service providers, patients and carers such as the Resolve toolkit, and the Carer Support Needs Assessment Tool Intervention.
Steven’s* Story about Palliative Care
“Marie* had the back pain for months until she fell and ended up in hospital. That’s when they found out it was breast cancer and it had gone to her bones and her liver too. Marie was 42 and Tom* just 10. But the tests were done fast, and we got an urgent appointment with the cancer specialist. The ward staff tried hard to control the pain but Marie got worse and confused too. They sent for the palliative care team which scared us, but the doctor explained that they work with other teams to help people like us and they did. New pain killers and letting us talk – about the medicines, the cancer, and everything else.
For two years, Marie did well with the different cancer treatments, got back to work and was her usual self. Then the cancer took off again. First in the lungs and then her brain. The cancer doctors did all they could. It was our district nurse who talked about hoping for the best but thinking about what would matter if Marie got worse. So hard for us to tell Tom, but his head teacher helped. The palliative care nurses worked with our GP to get on top of the breathlessness and headaches. Marie enjoyed the day hospice, and it gave me a break. We did struggle with making plans when we didn’t know exactly what would happen or when, but it was worth it.
We had to go to the hospital once when Marie had a bad chest infection, and she got better. The palliative care team visited, and everyone worked hard to get us home. Marie’s sister came, friends helped, and we had the nurses, home carers, and the GP too. It wasn’t easy but we managed, and it was the right place for us. Tom is doing ok. I have friends I can talk to, and my boss has been great.”
*not their real names
Ambition 6: Sustainable And Skilled Workforce
Our 10-year vision
A sustainable, skilled workforce with attractive career choices and fair work, where all are respected, supported and valued, whether they work wholly or partly in cancer services.
Our Workforce
- Is inclusive and diverse, reflective of the communities that it cares for and supports
- Has a working enironment that provides strong leadership, promotes wellbeing and supports people to grow and develop their capabilities
- Is an example of Fair Work
- Is skilled and trained - embracing new and emerging technologies, responding flexibly to patients’ expectations of the right care in the right place and the right time.
- Is enabled and equipped to support the delivery of projected growth in demand for health and social care services
- Is heard and at the heart of transforming Health and Social Care Services
- Across health and Social Care is recognised to be independent
Our strategy aligns with the Health and Social Care: National Workforce Strategy (2022). Our workforce is central to implementing our vision and delivering a whole system approach to improving health and wellbeing outcomes. At every stage of the journey to improve cancer survival, we need appropriately skilled and supported health and social care staff.
Strengthening our workforce means addressing the workforce journey through five pillars: plan, attract, employ, train and nurture.
The cancer workforce comprises a wide range of healthcare professionals, some of whom are cancer specialists and some for whom cancer is a component of their job. The NHS workforce has faced significant pressures and sustained actions are required – from planning for and attracting into the workforce, through to support and development of staff, including their mental health and wellbeing. We will model cancer workforce requirements taking account of where and how people with cancer most often use services, including primary care, and how these change as service delivery evolves. We will continue to grow the number of training places to expand the workforce we need for our strategic ambitions. Trainee places will be located in line with greatest need and to ensure that career opportunities within Scotland are offered to those qualifying here.
Alongside this growth, it will be vital to make fundamental changes to how our workforce is best deployed, ensuring that all professionals are doing the work they are best placed to do while recognising some tasks may be undertaken more appropriately by others. Technological advances and digital solutions will change how our workforce operates and how people with cancer access services, for example, increased use of telemedicine (clinical care provided remotely).
It will be crucial to maximise the retention of our workforce, providing support for mental health and wellbeing, providing flexibility in roles as individuals approach retirement, and increasingly collaborating and integrating roles across departmental or Board boundaries. Job plans require capacity within them for continual professional development, research (where relevant), and governance.
Data for success
We will need granular cancer workforce data to be able to complete a workforce review in oncology. We also need an understanding of where people with cancer meet the health system and how this may evolve in order to develop workforce requirements.
We will model training and staffing requirements and measure retention and retirement data.
Ambition 7: Person-Centred Care For All
Our 10-year vision
People with cancer are at the heart of all decisions and actions involving them. They are given the opportunity to co-design their own care plan, and information including a treatment summary is readily available. A single point of contact (SPOC) is at the centre of this. Where possible, diagnostic tests and treatment are situated close to home and travel to specialist care is fully supported, making use of the continued advancement in new technologies.
Value-based health care and Realistic Medicine mean outcomes are delivered through shared decision making and discussion about the potential benefits and harms of different treatment options, including the option to do nothing. This approach allows people to make an informed choice, as well as reducing waste and potential harm. Shared decision making and informed consent are fundamental to good practice: involving people in decisions about their care strengthens their ability to self-manage. In addition, evidence shows that they value their care more and experience less regret.
People with cancer have a potentially life-changing diagnosis and immediately become ‘patients’ that are served by a health system. The system and its staff need to treat and care for the individual person rather than the ‘patient’ or ‘tumour’, recognising each one’s preferences and needs. There are four principles underpinning person-centred care that should be central to all cancer services:
Person is treated with... dignity, compassion, respect
Care is... personalised
Care is... coordinated
Care is... enabling
- Dignity, compassion and respect ensuring all interactions are founded on kindness and our shared humanity.
- Personalised
- carefully listening to the things that matter most to people
- setting personal goals about treatment, care and daily life
- identifying personalised action or activities to help achieve personal goals.
- Enabling
- providing information in a way that is meaningful and easy to understand
- supporting people to make the right decisions based on the things that matter most to them
- supporting people to undertake activities and actions to help them achieve their goals helping people to live well on their own terms.
- Coordinated
- supports people to get support and treatment in a timely manner
- enables collaboration between services and professionals
- creates opportunities to combine interactions, for example through co-location.
A single point of contact (SPOC) has the potential to improve access to care and timely reporting of results; ease navigation through care pathways; improve communication and experience, shared decision making and patient-reported outcomes; and positively impact our workforce by releasing capacity to provide more proactive and expert care.
Getting It Right for Everyone (GIRFE) reflects similar values, providing a more personalised way to access help and support with a joined-up, coherent and consistent multi-agency approach. This will be a practice model across acute, community and social services going forward.
Data for success
We will need to develop a concise framework that outlines the key structures and processes that support a person-centred approach. We will develop metrics that measure processes such as shared decision making, and whether a ‘good’ personal outcome was achieved throughout the cancer journey, including supportive and palliative care.
We will continue to use PROMs and will also use the person-centred measurement framework using quantitative and qualitative data to better understand quality of care from the perspective of the person with cancer and their family.
We will monitor the availability of a single point of contact and measure the optimal model of delivery to inform future practice.
The Importance of a Single Point of Contact
A person affected by cancer shared their experience anonymously via Care Opinion. They highlighted the need for a single point of contact and the impact it could have:
“I was expecting to receive an appointment for a routine CT scan, before my next oncology appointment. Waiting for appointments to come through the post is on my mind for weeks around the appointment time, as I never quite know when to expect the letter or when the appointment will be. Knowing that a scan is imminent also brings to mind the what if questions, such as what if something shows up this time and the cancer is active again? So it's an anxious time…
… I had to make 5 calls to ‘strangers’ to finally understand why I didn’t have an appointment for my CT scan. I had to be on the ball and assertive. That’s a big ask for many patients who may be too ill, or lack confidence to ask for what they need. It took 2 weeks to get a resolution. That’s two weeks of worry and frustration for me, and 5 calls the NHS had to manage.
We need the Single Point of Contact to be rolled out to all cancer patients. How much nicer it would be to call one person, who might even be friendly and helpful, and be able to trust that they will look into the matter and update me. What a relief!”
Ambition 8: Tackling Inequalities
Our 10-year vision
A reduction in inequality in cancer incidence, access to services, experience and outcomes.
‘Inequalities’ denotes differences between groups and ‘inequities’ denotes unjust differences between groups. Inequalities disadvantage people and limit their chance to live longer, healthier lives.[25] If services are not provided equitably (process) then inequalities will remain (outcome). Some inequalities in cancer are more associated with specific factors (such as poorer survival in the elderly compared to younger people with cancer) whereas others are more systemic. For example, there is approximately 20% poorer uptake of cancer screening in the most deprived areas compared to the least deprived; those living in the most deprived areas are three times more likely to develop lung cancer; cancer-related deaths are 74% higher in the most deprived population than the least deprived.[26]
Both specific and systemic aspects need to be addressed.
Additional factors such as sex, age and ethnicity can influence cancer risk, access to services and outcomes, and the relationship amongst them is complex. Reducing inequalities means applying a broad, societal approach as well as targeting specific actions to disadvantaged groups along the cancer pathway. Best Start, Bright Futures (2022) aims to reduce health inequalities in the long-term by reducing child poverty now.
Scotland’s geography means there are particular challenges in providing equity of access to some rural and island communities. Improving the accessibility of services through the location of services and use of digital technology, providing transport, maintaining support structures, ensuring affordability and increased focus on cultural competence of services are all measures likely to reduce inequalities. Speciality outreach services can improve access and self-reported health.[27]
We will reduce inequities in access, experience and outcomes for individuals and groups experiencing socio-economic inequalities, racism and discrimination. We will do so by improving the way we collect and use data and evidence to monitor equity of access, experience and outcomes for marginalised and minoritised groups, and targeting action where it is needed most. In line with our commitments under the Race Equality Framework and Action Plan (2016-2030), the Expert Reference Group on Covid-19 and Ethnicity, and the Women’s Health Plan, we will have a specific, early focus on improving outcomes for minority ethnic groups, women and people living in the most deprived areas of Scotland.
We will promote healthy living by reducing alcohol, tobacco and drug use while encouraging active and healthy living, which will reduce the risk of developing cancer and enhance treatment outcomes and survival, in those at highest risk (see Preventing More Cancers).
We will improve inclusive communication and outreach to people who may not access screening although they wish to. Targeted screening (for example, for lung cancer as recommended by the National Screening Committee in September 2022) and new methodologies (such as cervical smear self-sampling) will be explored, to help reduce the screening inequalities gap (see Earlier and Faster Diagnosis). Inequalities funding has been used to develop an intelligence platform bringing together data from each screening programme to help identify common trends and identify inequality. This work will be continued to help develop processes to reach people currently excluded, by identifying and removing barriers.
Disparities in access to diagnostic and treatment services will be improved using new technology that facilitates alternative siting of services and remote consultations (see Flourishing Research and Innovation). We will make sure that efforts to add more digital elements into the health system are proportionate to ensure that nobody is left behind, while meeting the expectations of those who want to interact in this way. People with cancer will not be disadvantaged by the cost of travel or loss of paid working days.
Primary care, and especially general practice, has unique capacity and coverage in our communities to address entrenched health inequalities, and we aim to maximise its potential. Good quality prevention and early intervention in primary care are key to reducing preventable ill health, including cancer.
There will be more equal access to anticipatory care planning, palliative care, care around death and bereavement support. We will improve access to research and clinical trials for minority ethnic people and those that are currently underrepresented in clinical trials.
By practising Realistic Medicine, NHS Scotland can ensure we deliver the right care in the right place, reduce waste and harm, and redirect resources to where they will add the most benefit. We will promote equity of access to care and utilise a whole system approach that puts people’s needs at its heart. This is a vital step in reducing health inequalities.
Data for success
We will strengthen our ability to more closely monitor and to take action to address inequalities along the full cancer pathway.
We will better identify, monitor and address the healthcare needs, experiences, access and outcomes for marginalised and minority groups.
Ambition 9: Mental Health As Part Of Basic Care
Our 10-year vision
Dependent on need, proactive and comprehensive psychological and mental health interventions and support are available and accessible, from those trained at informed to specialist practice types, to all people affected by cancer and their families.
People recently diagnosed with cancer, those receiving treatment, those who have completed treatment, those receiving palliative care and those who are caring for people with cancer all report that the emotional aspects of cancer can be some of the most challenging. The post-treatment phase can be a particularly volatile time for mental wellbeing, and in almost half of all cancer cases, emotional effects are cited as more difficult to cope with than physical and practical effects.[28]
People affected by cancer can be better equipped emotionally and psychologically to face the challenges that lie ahead with the right psychological and spiritual support in the right place, by the right person, at the right time. The psychological and spiritual needs of the individual vary by personal circumstances and characteristics as well as cancer type and how they present. Access should be equitable regardless of geographical or socio-economic factors, ethnicity, gender, disability or other equality characteristic. By delivering person-centred care and psychologically focused care, we can empower people with cancer and potentially reduce the sense of loss of control that is commonly associated with cancer and its treatment.
The Psychological Therapies and Support Framework for People affected by Cancer provides service providers across Scotland with guidance to enable equitable and efficient access to psychological support, and a mechanism to monitor success and challenges at local, regional and national levels. A new Mental Health and Wellbeing Strategy for Scotland and a new National Specification for Psychological Therapies and Interventions will be published in 2023, which will recognise the mental health impacts on people of all ages affected by long term conditions including cancer. These tools should be embedded in all cancer care.
Data for success
We will measure and monitor mental health in established cancer care pathways.
We will measure mental health through qualitative experiential data.
We will identify waiting times for psychological care through the psychological therapies national waiting times standard and use indicators from the new National Specification for Psychological Therapies and Interventions once published.
Ambition 10: Flourishing Research And Innovation
Our 10-year vision
Equitable access to clinical trials has become integral to the management of treatment options. Where relevant, health professionals have allocated research time, adequate laboratory support, and are working in partnership across academia, industry and the third sector. Qualitative and non-RCT research are providing relevant, quality evidence to inform best care. Routine cancer data are available to support this.
More complex molecular tests ensure people with cancer have access to a portfolio of precision oncology and clinical research. Laboratories have capacity to support research, including clinical trials.
New technologies are being used to strengthen the full cancer patient pathway, with alternative methods for consultations and information-sharing leading to greater choice and convenience for people with cancer. The application of artificial intelligence (AI) has grown. Multidisciplinary networks are making the best use of scientific and clinical expertise to translate innovation into clinical practice. Health boards make robust, evidence-based decisions based on Scottish Health Technologies Group (SHTG) advice, leading to improved outcomes and more efficient use of resources.
Research and innovation are a core part of the NHS. They play a key role in improving earlier diagnosis rates (see Earlier and Faster Diagnosis), enabling people with cancer to access new treatments at an earlier stage and influencing health planning and policy. Public Health Scotland (PHS) facilitates research studies through centres and the electronic Data Research and Innovation Service (eDRIS). Strong links between research in cancer and related fields such as primary care, mental health and palliative care are important, including qualitative and non-RCT research.
We live in a time of extraordinary innovation in technology that provides opportunities to diagnose and treat people with cancer. These range from the genomics revolution in diagnostics and treatment, to advances in the use of AI, 5G, Internet of Things in healthcare through to the apps, tools and products that we now use in our everyday lives. Recent health service examples include the use of video appointments such as Near Me and the use of drones in supply chains.[29] In March 2022, we reached 1.5 million Near Me appointments across Scotland, saving an estimated 49 million travel miles for patient, families and staff.
Our approach to digital health will be guided by the Digital Healthcare Strategy (2021). The Digital Front Door work will be a key development for people interacting with health and social care services in Scotland.
The SHIP aims to strengthen Scotland’s innovation activities in health and social care with a focus on early-stage innovation. The CfSD’s ANIA Pathway aims to fast-track proven innovations into the healthcare frontline on a Once for Scotland basis, with an early focus on innovations for delivery of care in cancer. The SHTG in Healthcare Improvement Scotland provides evidence-informed advice on the use of health technologies. It works, as others, in partnership with NHS Local Board and Regional Test Bed infrastructure to ensure that products, services and processes developed are relevant and effective for NHS Scotland.
Data for success
We will need a standardised suite of performance measures for the clinical research community and simple key performance indicators for health boards.
Service data and patient outcome data is needed to monitor new technologies.
Ambition 11: Cancer Information And Intelligence Led Services
Our 10-year vision
There is a more integrated cancer intelligence platform along the full cancer pathway. This creates a responsive system that efficiently supports data collection, retrieval and use for clinical management, surveillance, evidence generation and policy development, which is aligned to the move towards a single electronic health record. Quality Performance Indicators will be a key driver of an overall cancer services improvement agenda, aligning with optimal pathways and national clinical management pathways. Data collection and analysis of measures including PROMs (patient-reported outcome measures) and PREMs (patient-reported experience measures) are integrated into service provision to facilitate person-centred care and shared decision making. This means:
- Improved completeness, quality, timeliness and use of data (diagnostic, clinical, inequalities and experience) along the patient pathway.
- Data definitions are consistent across Scotland, the UK and beyond.
- The Cancer Medicines Outcome Programme (CMOP) is a national, world-leading cancer intelligence asset capable of recording and analysing real-world medicines use, and disease-specific outcomes data at patient and population levels.
- Data interpretation and utilisation skills are core for the cancer workforce. The workforce is prepared and delivering services with the most appropriate and advanced technologies (including virtual and asynchronous appointments).
- Systems used to support the delivery of cancer services continue to have information governance assurance, and cyber and data security at their core. By working with regulators and applying agreed standards, improved data infrastructure allows greater efficiency of clinical practice and knowledge flow, and data utilisation.
Cancer data capture and use should be seamless across all health and social care settings, make best use of technology, and provide timely intelligence to those who need it, along the full cancer pathway. Data are fundamental to understanding the whole system of cancer control and care. They support service delivery and redesign including person-centred decision making, and policy and planning. They are required for audit, quality improvement, research and primary prevention. PHS operates the Scottish Cancer Registry and Intelligence Service, collects Quality Performance Indictor Data as well as reporting on a range of audits and cancer services (see Appendix 2).
The Innovative Healthcare Delivery Programme (IHDP), in collaboration with PHS and NSS, has worked over the past seven years to transform access to cancer data in Scotland, with the aim of harnessing NHS Scotland’s rich data assets to improve cancer patient outcomes. IHDP is now an integral part of PHS. New data sources have been added to the Scottish Cancer Registry as well as the creation of wrap-around intelligence services. The SCRIS project has catalysed many developments in the processing and supply of national cancer data, such as the national publication of SACT utilisation data during the pandemic to allow monitoring of recovery. SCRIS provides a secure, single point of entry to an increasing number of ‘joined up’ national cancer datasets and broad range cancer-related information. The datasets cover 17 cancer indicators, with work ongoing to obtain further ones such as lifestyle risk factors and selective primary care data; workforce planning; diagnostics and laboratory data; multidisciplinary team (MDT) data; rehabilitation data; patient-reported outcome measures (PROMs); and data relating to recurrence and secondary cancers. The new Cancer Intelligence Platform being developed by PHS and NSS will allow all these evolving data to be hosted and accessible in the years to come. Better co-ordination and joining up of the cancer data science community, including in analytical work, will ensure the most efficient use of resources across cancer services, supported by PHS.
The CMOP provides an opportunity for NHS Scotland to gather cancer medicines intelligence where there is uncertainty, about ‘real world’ outcomes (as opposed to those reported in clinical trials). This is done for both new and established medicines, from supporting the early health technology assessment phase of new medicines, through to the ongoing monitoring of medicines in routine use.
Quality Performance Indicators will be a key driver of an overall cancer services improvement agenda, aligning with optimal pathways and national clinical management pathways.
Contact
Email: cancerpolicyteam@gov.scot
There is a problem
Thanks for your feedback