Care Home Data Review - Full Report
The Care Home Data Review (CHDR) is a collaboration between Scottish Government, Public Health Scotland and Care Inspectorate, with the aim of improving the care home data landscape. This report details the feedback to the review and presents recommendations for data improvements.
Data Systems & Standardisation
The Data Strategy for Health and Social Care and Digital Strategy Delivery Plan set out the vision, aims and actions being taken forward across the whole of health and social care to both improve digital systems and increase interoperability through the adoption and use of common standards.
When looking at data systems and standardisation, it is recognised that there are potential risks in focusing solely on care home data in isolation. As a result, many of the potential solutions to issues raised within the Care Home Data Review will need to be taken forwards as part of wider programmes of work, with the recommendations concentrating mainly on how to ensure alignment between the Care Home Data Review and the aims and deliverables of the Data Strategy for Health and Social Care and Digital Strategy for Health and Social Care.
Data systems/processes
The Data Strategy for Health and Social Care notes that information systems across health and social care do not currently make it easy to access and share data across organisations within the sector. The strategy notes that increasing our understanding of the existing data available and improving our technologies for storing and accessing data, will make it easier for both professionals and individuals to access the right data at the right time.
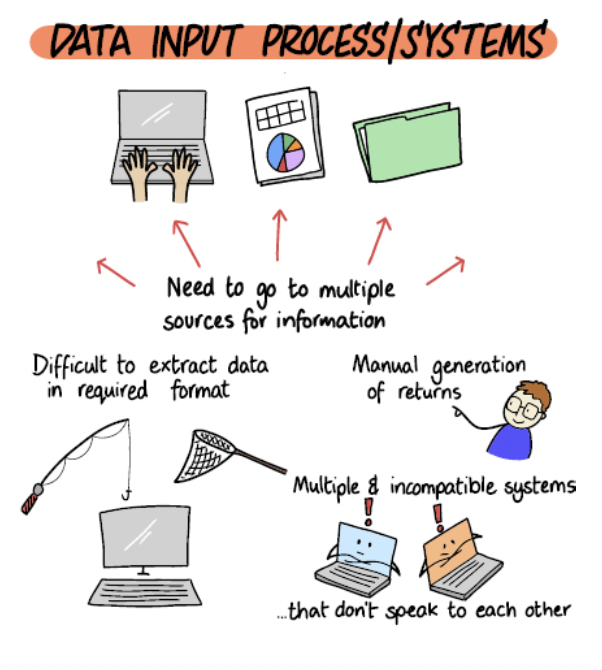
Due to the mixed nature of care home provision, with public, private and voluntary / not for profit providers, there are a wide range of systems and processes used to generate, capture and record data. These range from paper based records to a variety of different electronic Management Information Systems (MIS), with differing systems maturity. Feedback from the review suggested that, in many cases, the information requested for local and national purposes is difficult to extract and provide in the required format. This is exacerbated by multiple requests asking for similar, but subtlety different, information.
The current systems for data provision often require providers going to multiple sources and using multiple systems to provide data. Providers also commented on the current requirement to use a number of different websites/tools to input data for each data collections. In many cases, data is required to be manually input rather than extracted from the existing systems and this is time consuming and increases the chance of errors. The lack of consistent data requests means that data providers have to provide multiple datasets to different groups, through different systems. This increases workload and frustration.
Differences in systems / system maturity
There are large variations in the systems and system maturity used for data management across the care home sector, at both individual care home and local data provider level.
The Landscape Assessment of Data and Digital Readiness of Scottish Care Homes (LADDeR) study attempted to map the current data and digital readiness in care homes, the systems used to collect and store data, and how this information is shared with other care partners. The study covered the south-east of Scotland and found that the majority of cares home still use paper based management systems.
Furthermore, despite being out of scope of this review, it is recognised that there are issues around digital connectivity within some care homes which will impact on data processes. In the LADDeR study[52], 43 care homes answered questions on digital connectivity. All had wireless internet connection capabilities, however, “most care homes have less than optimal internet connection. Poor connectivity and regular service interruptions are experienced by 18%, and a further 40% report service is interrupted at times and long loading times.”
Changes at Local Government level
The local government data platform will fundamentally change the reporting landscape, by introducing a local government owned data broker between local authorities and data producers / requesters. The platform will manage and orchestrate the collection of data, collating returns from individual authorities into a single dataset, and will drive improvements in data quality, timeliness and standardisation. The platform will be designed to integrate with the existing and the future wider data ecosystem, by using secure and efficient methods to transfer and give access to data.
Management Information Systems
Although decisions around resourcing Management Information Systems are decided locally and are out of scope of this review, there are some actions which can help data providers when they are procuring or modifying their Management Information System. For example, the mandating of data standards would enable systems suppliers to understand the minimum data requirements and formats expected by the local and national data collecting organisations. A potential option for implementing data standards could be through procurements contracts. Standardisation is covered further below.
Case study: Care Homes Assessment Tool
Data collection and usage can be enabled by digital technologies. DHI (Digital Health & Care Innovation Centre) and Scottish Care collaborated with a range of partners on the live testing of an innovative Care Home Assessment Tool (CHAT) in Lanarkshire and Glasgow which spanned 3 waves of the Covid-19 pandemic (Aug 20 – June 22). CHAT aimed to aid communications between care homes and GP practices to support local operational decision-making and enable rapid access to external clinical support for deteriorating resident situations. The project highlighted some of the issues with the current digital landscape.
The CHAT application itself was considered very simple and easy to use by care home staff, but a more sophisticated approach would be required to match individual resident need to the most appropriate external service out with the specific challenges of the pandemic. There is significant variation in care home service models across Scotland, with complex relationships in place with a wide range of health and support service providers but where data sharing could provide significant resident, staff, and organisational benefits.
CHAT identified the importance of establishing an overarching national Product Owner and the need to integrate digital solutions within a wider ICT system architecture if they are to be adopted at scale and support the efficient transfer and storage of data.
The interim use of secure email was used in CHAT as a rapid communication channel between care homes and GP practices, but this did not automatically transfer data into the GP Docman system, creating risk and inefficient pathways. Data quality and lack of interoperability between legacy systems are systemic problems which will require national level decisions and investment.
Digital applications should also provide multi-directional data flow between the care home, GP practices/Out of Hours Services and expand the resident data to include non-infection related conditions.
There are also significant challenges in navigating and aligning information governance and compliance processes and documentation across different providers and sectors. These need to be clear, streamlined and be accompanied by readily available professional IG support if they are not to be seen as barriers to innovation.
The requirement for a consistent national approach to support Care Homes staff training and digital upskilling was also a key finding.
Ongoing work - systems
As noted above, the systems issues raised in the Care Home Data Review are only one part of much wider considerations relating to improvements in technology and infrastructure across the whole of health and social care.
The Data Strategy for Health and Social Care – 2024 update outlines the improvements already made to digital infrastructure and the tools available to improve the way that we collect, store and analyse data. The document also sets out the priority areas 2024-25. Two key developments for improving access to data for both the public and professionals are the development of the National Digital Platform (NDP) infrastructure and the Integrated Social Care and Health Record.
The Technical Design Authority was established in February 2024 to provide assurance on the development of the blueprint for Scotland’s digital and data systems. The blueprint will reduce the variety of architecture in use and bring consistency to improve and align data infrastructure across health and social care. In addition, it will provide IT suppliers with clarity and understanding of the system and help better manage contracts.
Case study: Expanding the use of CHI (Community Health Index) in social work and social care
COSLA and COSLA’s Digital Office have been exploring the benefits and risk of using CHI in Local Government to support more effective data matching and data sharing. Engagement took place from January to June 2024 with a wide range of stakeholders including Local Government professional groups, NHS colleagues, Third and Independent sectors and people with lived experience to inform their thinking and ensure alignment with broader Local Government and national work. The engagement has enabled groups to provide feedback and insights into existing programmes of work where the use of CHI could potentially bring added value and support the proof of concept.
There are many potential benefits to adopting CHI in Local Government such as:
- supporting data linkage and improve data quality
- act as a verification tool for accessing the Digital Front Door and the Integrated Social Care and Health Record
- support sustainable person-centred public services and reduce inequalities within Scotland’s current fiscal challenges, ageing demography and recruitment and retention challenges
- support integrated health and social care and delivery of better outcomes to people accessing services
- reduce duplication in the system
- reduce the need for people to repeat information multiple times
- increase capacity in an already stretched system
Standardisation
As noted previously, the care home data landscape is complicated by having a large number of different organisations involved in the provision of care, using different systems and standards and with differences in data maturity across local areas. The lack of standardisation and harmonisation can lead to inconsistent data to inform decisions, reduce comparability and interoperability, increase the data collection burden, and make it difficult to reuse data. It was noted in the review that data standardisation, and sharing, are critical to rationalising the current data landscape.

As with the development of system solutions, the work to establish common data standards for care home data will be only one part of much wider work ongoing to develop standards across the whole of health and social care.
The Data Strategy for Health and Social Care commits to setting out the preferred data standards for use across the sector to drive up common approaches to the way in which data is captured, to facilitate interoperability and make it easier to reuse and link data. The Digital Strategy Delivery Plan similarly notes the planned programme of work “to set out our approach to the introduction of legally mandated standards for the safe and effective sharing of information across health and social care, under the powers proposed by the National Care Service (Scotland) Bill”.
The Data Standards Sub Board has been established to allow COSLA and the Scottish Government to lead work to set out the preferred standards for use across the health and social care sector, to oversee and take forward a common approach to the way in which data is captured. Data definitions and standards that should be applied to and across data collections fall within the scope of the Sub Board. It is important that any consideration by the Care Home Data Working Group of data standards and definitions for use across care home data collections is linked into the work of the Data Standards Sub Board. Members from the Care Home Data Review Working Group will sit on the Data Standards Sub Board to ensure alignment and will be able to contribute directly to this area of work. For example, a key aspect of this work will be the mapping of existing data standards and data collections. The data mapping work carried out as part of the review, and associated metadata, will help to provide the relevant information for care home data.
In addition to linking into the longer term wider programme of work on data standardisation, the Care Home Data Working Group will look to consider potential quick wins for aligning definitions and standards across care home data collection. For example, there is currently a discrepancy between locations categorised as care homes on the PHS locations list, also used by NRS for care home deaths data, and those legally permitted to operate as a care home as set out on the Care Inspectorate register of services. Work is being taken forward across SG, PHS, CI and NRS to look to align the definition of a care home used in our statistics. This will allow a more consistent picture of care home information across organisations.
Similarly, several of the national data collections ask for information about residents’ client group (for example, Dementia, Learning Disability). However, during the mapping of the data landscape, it was evident that there is a lack of standardisation across the data collections thus increasing burden and also introducing greater complexity in working with, and in understanding analysis about care home residents due to the inconsistencies. Where differences in definitions are identified across collections, the Care Home Data Working Group will work with the organisations responsible for these collections, along with providers and users, to investigate the potential for aligning definitions.
As well as specific work to consider standardisation, some of the other recommendations from the review should also help with ensuring a more standardised approach to data collection. For example, the setting up of data networks and a process for establishing new data collections to help ensure that data asks are consistently understood and aligned.
Data Systems & standardisation: Aims and recommendations
Aims: Improve data systems and interoperability
Recommendations: Link in with the wider work on improving data infrastructure and interoperability as part of the Digital Health and Care Strategy.
Work with local government partners to explore alignment of work on care home data to the Local Government Data Platform project.
Continue to explore existing systems and real-life care home data capture in order to better understand and inform required improvements.
Aims: Agree consistent standards and definitions for use across care home data collections.
Recommendations: Link in with the work of the Data Standards Sub-board for health and social care.
Investigate the potential for national data collections to align with appropriate standards set by work being led by Scottish Government and COSLA, working with relevant stakeholders.
Scope out the work required and the potential for data producers to ensure national care home data collections, and national datasets which have a care home flag / code, use the Care Inspectorate care home definition and unique identifiers to ensure consistency, and enable data linkage, across datasets.
Contact
Email: SWStat@gov.scot
There is a problem
Thanks for your feedback