Care Home Data Review - Full Report
The Care Home Data Review (CHDR) is a collaboration between Scottish Government, Public Health Scotland and Care Inspectorate, with the aim of improving the care home data landscape. This report details the feedback to the review and presents recommendations for data improvements.
Data gaps
Current gaps in data
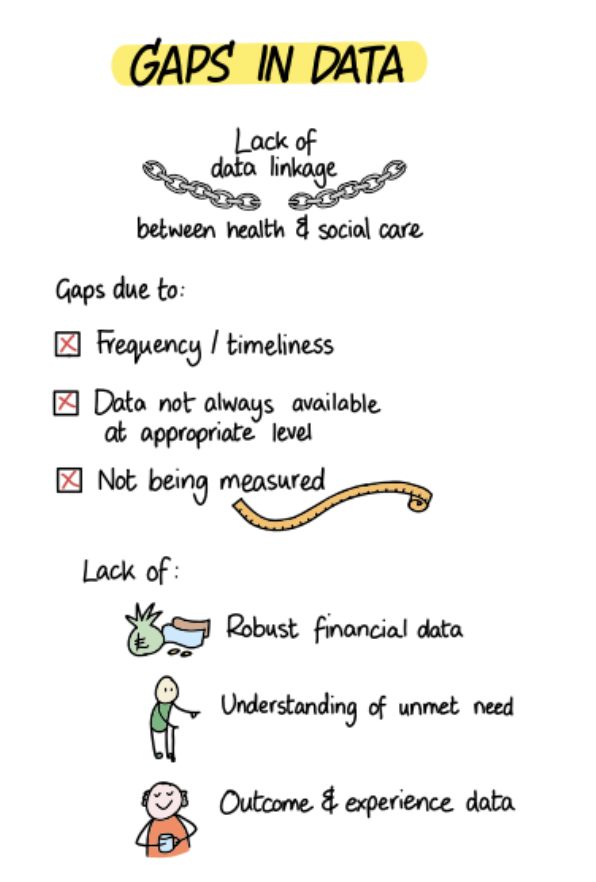
It is widely acknowledged that there are many gaps around care home data and evidence in Scotland, as well as issues around the timeliness of data. Gaps highlighted throughout the care home data review and within the research literature include: data on outcomes and wellbeing, care and support experiences, unmet need, the role of care homes for providing different types of care, and the complexity and dependency of care home residents. [7] ,[8] ,[9] ,[10] ,[11], [12]
The Covid-19 pandemic also highlighted fundamental gaps with our care home data, particularly around being able to identify the care home population[13],[14],[15],[16]. Our inability to answer key questions, such as who lives in a care home, during the pandemic “exposed data failings that have hindered service development and research for years.” [17]:
“Fundamental gaps, in terms of population and service demographics coupled with difficulties identifying the population in routine data are a significant limitation. These challenges are a key factor underpinning the failure to provide timely and responsive policy decisions to support care homes.”[18]
Further reports, such as Audit Scotland’s Social Care Briefing[19] and Office for Statistical Regulation’s report on Adult Social Care Statistics[20] discuss how improvements to social care data are essential for decision making and for implementing social care reform. The Audit Scotland report cites limitations across the social care sector around the lack of a social care record like an NHS record, and gaps in recording unmet need.
A common theme identified during the review was the need for better and more timely data about the needs of care home residents, to enable care home service planning as well as responsive policy nationally and locally, which should in turn inform better care. In addition, national and local organisations require data to enable benchmarking and allow monitoring and evaluation of outcomes, quality, improvement and safety. For example, data required to understand and monitor the improvements made under the Healthcare Framework for adults living in care homes.
In general, whilst it is recognised a large amount of data already exists, the areas highlighted for development fall under the following broad categories:
Care home residents – it is essential to understand who care home residents are, as well as the composition and needs of the resident population (age, frailty, health conditions, wellbeing). Ways for looking beyond the plain numbers to understanding the complexity of care.
Care home workforce – there is a need for more timely and accurate data on staff recruitment, turnover and retention, to determine safe staffing levels to meet the needs of residents.
Care home services – real time data on capacity (by bed type), occupancy rates, bed vacancies and discharges. Better data on outbreaks (covid, flu, norovirus etc) and visiting information.
Care home finance – need robust financial information relating to care homes, including types of funding, who is on contract rate and details for charges to self-funders.
More details of the data requirements highlighted in the review for each of the categories are available in the summary of workshop discussions. As part of the work to establish a more detailed understanding of data needs, the CHD Working Group will work to prioritise the data gaps identified in the review and document any additional requirements if required. This work will look to map the data needs across all stakeholders, identify and agree the key questions to be answered, at what level, and look to link these to existing sources and identify and assess the feasibility of new/revised data sources/collections/methods of estimation, where required. As has been mentioned, a key consideration when assessing data needs will be balancing the value of the information obtainable against the burden of data collection.
Equalities data
During the review, there have been a number of requests for improved quality, coverage and depth relating to equalities data. This requirement links into wider work being taken forward as part of Scottish Government’s Equality Data Improvement Programme (EDIP) which was launched in 2021. EDIP aims to put in place a stronger and more complete equality evidence base that will enable more inclusive policy making and support the collective effort across the public sector to fulfil the requirements of the Public Sector Equality Duty. The latest Equality Evidence Strategy, covering 2023-25, aims to improve the quality and comprehensiveness of equalities data and intersectionality.
A summary of equalities data available for social care in Scotland can be found in the Equality Evidence Finder[21]. Although data is available for some of the equality characteristics, there are known gaps (e.g. religion), emerging requirements (e.g. Augmentative and Alternative Communication) and inconsistent classifications are used across data collections (e.g. ethnicity). Understanding where there is a need for equalities data improvement will be considered by the CHD Working Group as part of its role in establishing wider data needs.
Data inclusivity
In October 2020, the UK’s National Statistician commissioned an Inclusive Data Taskforce “with the aim of making sure everyone is counted and nobody is forgotten in UK data and evidence.”[22] The Taskforce concluded that data about care home residents was a critical data gap[23].
An example of inclusivity in a Scottish care home data collection is the Scottish Care Home Census. “All sectors of care are invited to participate and are included, meaning private, not-for-profit and local authority care homes are included. This is in contrast to usual approaches which have been provider-led or only included those funded by their local authority. The Scottish Care Home Census also includes data on all adult care home services, without restrictions around age and service type. This is important as, although the majority of care home residents are older adults, younger age groups are a significant group, often with complex needs, who can otherwise be overlooked”[24]. Part of the responsibility of the CHD Working Group will be to identify data requirements, such as ensuring data inclusivity where appropriate, and work with data users to prioritise gaps.
Linking datasets
The research literature raises that the lack of common identifiers to link across some datasets within social care and across sectors hinders the insights we can obtain from current data collections[25],[26]. Data linkage provides opportunities for much richer social care and cross sector analysis[27]. Data linkage also provides opportunities for improving data quality and can also potentially help with identifying and addressing gaps. Currently there is some data linkage involving care home data routinely undertaken by PHS and some summarised information linked to health data is publicly available through the PHS insights into social care - care home dashboard. Some further management information is provided to health and social care partnerships.
Examples of the types of national data linkage projects which could be undertaken include:
- Evidencing the variation in health and social care pathways by HSCPs,
- Evidencing health and social care pathways for different cohorts for example, is there a difference in people’s care packages and health outcomes (e.g. A&E attendances, number of unplanned admissions) for people with unmet caring needs (as identified by HACE (Health & Care Experience Survey)) compared to those with care packages in place and who don’t identify as having unmet need.
- Using data linkage to improve the quality and completeness of data e.g. social care client group / characteristics information e.g. dementia, mental health, frailty.
- Using data linkage to identify data gaps for example, understanding which social care sub populations are excluded from HACE and are therefore missing from national social care experience data.
Some stakeholders noted the lack of linked health and social care data as a key omission – and noted the potential value added in understanding the holistic picture of care home residents and both their characteristics and potential pathways through the health and social care system.
Stakeholders identified the need for timely access to routinely linked health and social care datasets (including longitudinal data), in addition to timely access to ad hoc linkages[28] with the appropriate information governance in place. Some of the challenges associated with data linkage are discussed further in the chapter on Data Sharing.
Data quality and timeliness
The review also found that, in some cases, issues with the quality and/or timeliness of existing data can lead to either a reduction in its usefulness or it not being used at all – essentially creating a data gap.
For example, the time lag between the Source Social Care data return and its publication means it is suitable for some users but not for all.[29] To try and improve timescales the latest source social care data has been published in sections to try and make this available in a more timely manner. More timely data on staff recruitment, turnover and retention was also frequently cited during the stakeholder workshop[30].
“Data is often out of date by time of publication.”[31]
In terms of service planning, management systems such as Turas do not reflect the change in circumstances in care homes in real time, so the management data in Turas was out of date as soon as it was released. Health and Social Care Partnerships (HSCPs) commented that they had to phone care homes directly to get the latest vacancy information, thus increasing the burden both on them and on the care homes[32].
As noted in other sections of this report, the quality and timeliness of the data required will depend on the purpose for which it is required.
Data granularity
Another issue identified is the granularity of data[33]. Some data users are unable to access the data in the geography or unit they require. Also, ensuring that data collections and analysis consider all care home types and not just care homes for older people was an example provided by stakeholders. Depending on the data requirements, how the data is accessed and by whom, there may be Information Governance implications (see also Data Sharing chapter). The CHD Working Group will need to work with data users to understand data requirements and the Information Governance implications.
Aligning data requirements
Over recent years there has been a growing ask of care homes, HSCPs, local authorities and NHS Boards for more frequent and timely data (management information). This is in parallel to the routine data asks which are used for longer term planning, evaluation, policy development, Official Statistics reporting and research. There is a balance to be had with short turnaround data (management information) and the other data which may have a longer turnaround but is often more complete and of better quality. There are gaps and challenges to be addressed with all types of care home data, so close collaboration with the care home sector, care home analytical community and other data users will be required to achieve the aim of ensuring we have the right data at the right time, with the appropriate governance, to make informed decisions to benefit our care homes, residents and workforce (see also the Strategic Oversight And Co-ordination chapter).
As noted above, the Care Home Data Working Group will work with the data provider/user networks to further develop a shared understanding of the data needs of different users. A key aim of this work will be to understand and articulate what data is available, how it can be accessed, and by whom.
Case study: Identifying a care home population
The commonest route used to identify care home residents in routine data is using the CHI (Community Health Index) database (based on GP registration data), which includes the CHI Institution Flag. This coding is applied by Practitioner Services Division (PSD) and is based on GP registration / address information submitted to them by GP practices.
However, despite CHI providing a route to identify care home residents, there are currently a number of challenges when trying to use the CHI database for this purpose:
(i) The CHI Institution Flag data is incomplete – not all care homes are identified using these codes and it includes some addresses which are not care homes (e.g. sheltered housing complexes). PSD have not based coding on the Care Inspectorate list of registered services. Use of the CHI Institution Flag only allows you to analyse at a granular level (care home resident versus not), rather than at care home level.
(ii) Address data in the CHI database is extremely messy in terms of structure and format and this problem is exacerbated by the varied ways care home addresses can be presented (e.g. resident room number, house, building, care home name, company name, street name or combinations) and that GP data may not be updated if the care home changes name (e.g. ownership). Standard address lookups have not been used to enter these details at time of registration.
(iii) Care home residency is dynamic and temporary residence is common with use of care homes for respite care, intermediate care, step-up/step-down from hospital or for temporary placement awaiting care at home or definitive care home placement. Not all of these will trigger a change of registered GP address and so it is difficult to capture the care home population at any point in time. Important to note that not all care home services have residents registered in CHI – primarily those whose main business is in respite services – thus CHI will never provide a complete care home population alone.
To enable identification of households, PHS and the Improvement Service (IS) undertook a matching exercise using an algorithm developed by the IS which assigned a Unique Property Reference Number (UPRN) to the address information on the CHI database in 2020. There was ~90% match of UPRN to CHI[iv]. However, around 40% of care home addresses were in the 10% of addresses which could not be matched automatically. Manual work was undertaken to assign a UPRN to every active adult care home service in Scotland between February 2020 and November 2021, to enable analysis funded by SG and undertaken with PHS/University of Glasgow/University of Edinburgh which looked at COVID-19 in care homes. If care homes have a UPRN assigned, this allows for care home level analysis. This will require updating to ensure new/changed care home services can be included.
Data gaps: Aims and recommendations
Aim: Work with the care home sector and data users to prioritise and identify how best to address our data gaps.
Recommendation: Having identified data requirements and compared to the current data landscape, work with data users to prioritise gaps. A number of key areas were raised during the review, examples include "Workforce, recruitment, turnover & retention ", “Outcomes & Experience" and " Resident population & needs data".
Aim: Make better use of techniques and technology, such as data linkage, and collaborate to share data to address data gaps.
Recommendation: Explore and develop case studies on success of alternative methods for improving quality / addressing data gaps. For example, using Unique Property Reference Number (UPRN) data to improve data availability and reduce need for multiple collection.
Contact
Email: SWStat@gov.scot
There is a problem
Thanks for your feedback