Neonatal intensive care unit services - demand and capacity modelling: final report
This report outlines this modelling approach, inputs, and interpretation of the outputs to support the future of neonatal intensive care unit (NICU) services.
2. Methodology
2.1 Overarching approach
The scope of this work focuses on understanding the demand and physical capacity needs of the future model of neonatal care in Scotland. The approach to this work contains two main strands: modelling and engagement. Figure 1 below provides an illustrative overview of each stage, alongside the key modelling and engagement activities.

2.2 Approach to modelling
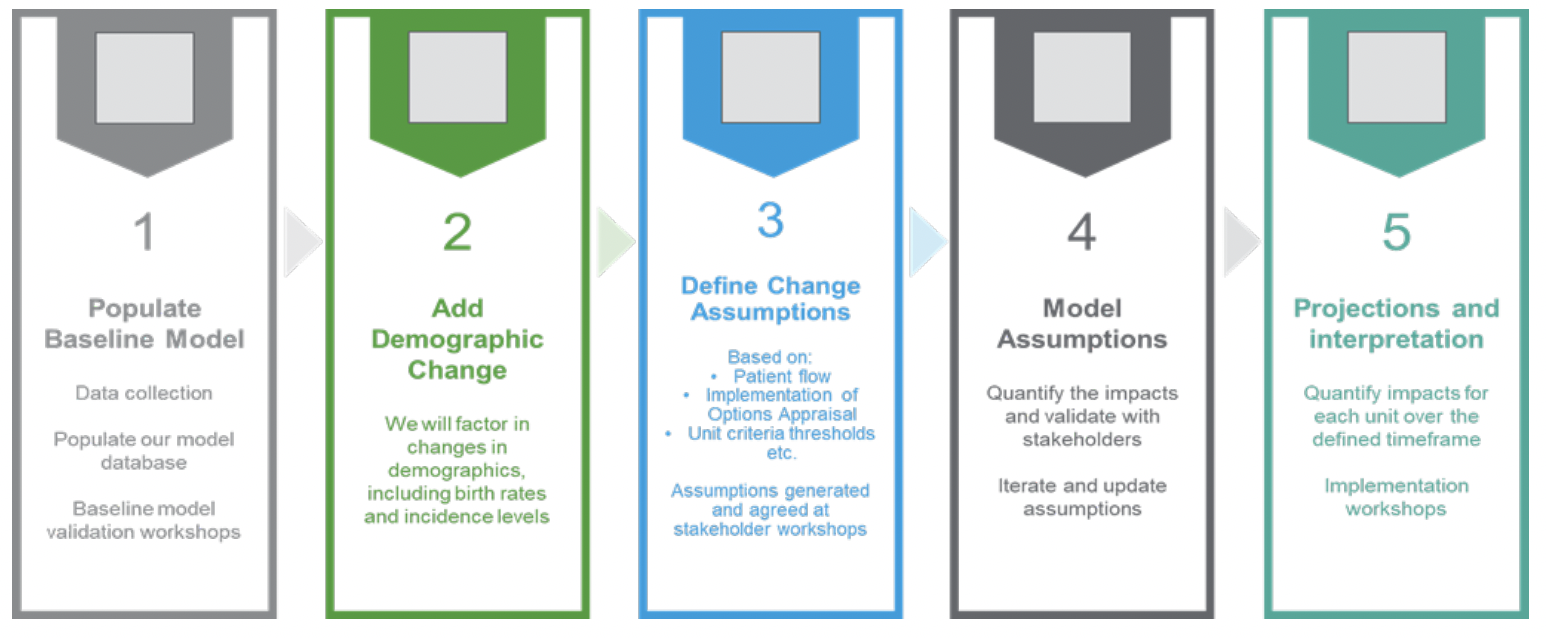
The modelling approach has encompassed five stages, as summarised in Figure 2.
2.2.1 Populate Baseline Model
Data was collected from a range of sources (see Section 2.4 for more information) to develop the baseline analysis. Longitudinal analysis was conducted to determine whether there was any seasonality or time series trends in the data and to establish a baseline for the model. This baseline analysis was validated through a series of operational and strategic stakeholder workshops (see Section 2.5 for further information on engagement). Following the validation stage, the baseline data was used to develop the demand and capacity model.
2.2.2 Add Demographic Change
The first stage of the modelling was to apply demographic change to the model. This was applied using the Scottish sub-national 2018-based population projections (Source: ONS / National Records of Scotland) for each local authority area (applied to the place of residence to each mother in the baseline). Demographic change was modelled over the planning horizon (projected to 2026/27). Incidence rates for babies requiring NICU care was also applied, in line with feedback from stakeholders on the increased propensity to treat smaller and sicker babies over time.
2.2.3 Define Change Assumptions
Throughout the modelling and engagement with stakeholders, a series of change assumptions have been identified for inclusion in the model. These include:
- The process for identifying the smallest and sickest babies who will move in the future model of care;
- The principles for the flow of babies between neonatal units;
- The suggested occupancy rates across neonatal units and levels of care;
- The length of stay assumptions associated with the repatriation of babies to the future LNUs;
- The frequency of in-utero transfers, in relation to total activity; and
- Assumptions to help estimate the additional impact on maternity and transport services.
Sensitivity analysis (through alternative scenarios) has been undertaken to test for the impact of changing assumptions. The primary model assumptions for which alternative scenarios have been tested include:
- Changes in the proportions of sickest babies who would move in the future model; and
- The flow of babies between neonatal units.
2.2.4 Model Assumptions
The baseline data and assumptions have been used to model the following outputs:
- The future number of cots required at each of the in-scope units;
- The additional maternity capacity (in terms of maternity beds) required as a result of additional in-utero transfers; and
- The potential number of additional ex-utero transfers which will be required to support the future model of care.
The outputs of this modelling have been shared and validated with stakeholders through a range of operational and strategic stakeholder workshops. The interpretation of the modelled impacts has been included throughout Section 5 of this report.
2.3 Model scope
Table 1 provides a summary of the model scope[2], which was refined throughout initial engagement with Scottish Government, regional planners, and clinicians.
| Identified NICU sites |
|
|---|---|
| Current NICU sites |
|
| Early implementer NICU sites |
|
| Partner organisations |
|
| In scope (for identified and previous NICU sites) |
|
| Out of scope* |
|
2.4 Summary of the evidence
In order to establish a baseline and evidence-based
2.4.1 Documentation reviewed
This modelling utilises and builds on a body of work that has going before it, not least ‘The Best Start: A Five-Year Forward Plan for Maternity and Neonatal Care in Scotland’ (January 2017). This outlined the new model of neonatal service provision and changes that would need to occur to make this happen. In addition to this, the following key documentation was reviewed both for context and to support planning assumptions for the model:
- Neonatal Intensive Care Options Appraisal Report – A Five-Year Forward Plan for Maternity and Neonatal Services (July 2023)
- A Framework for Practice – Criteria to Define Levels of Neonatal Care including Repatriation within NHS Scotland (July 2023)
- Principles of Discharge Planning and Neonatal Follow Up, A Framework (November 2019)
- NHS Lothian Early Implementers Evaluation Report (November 2022)
- NHS Ayrshire and Arran Early Implementers Evaluation Report – (November 2022)
- Optimal Arrangements for Neonatal Intensive Care Units in the UK – A BAPM Framework for Practice (2021)
There was a range of publicly available supporting data that was used in the modelling approach, including population projections and geographical reference data.
2.4.2 Data requested
In order to have sufficient unit and geographical granularity within the baseline analysis and modelling, data was collected from PHS, ScotSTAR / Scottish Ambulance Service, plus each of the eight units that have been included within the model scope. The data collected was grouped into four thematic areas: activity, capacity, workforce, and patient cohort. Table 2 provides a summary of the data collected from each of these organisations.
| Data requested | |
|---|---|
| Activity | Data was requested from units covering all neonatal activity for the previous three years. Information included within this dataset included:
|
| Capacity | Data was requested from units covering to identity trends in their capacity by neonatal level of care (IC, HD, SC) and for in-utero transfers. The following data was collected on a monthly basis:.
|
| Workforce | Staffing data by professional role and grade (where relevant), including:
|
| Patient cohort | The number of babies born by the resident local authority and hospital location of birth, birthweight, and gestation. This dataset contained five years of data (April 2018 – November 2023) |
2.5 Engagement
The overarching approach that has been undertaken has included engagement with both operational and strategic stakeholders at each stage of the modelling work. A summary of the stakeholders who have been engaged and the types of engagement undertaken has been included below:
| Stakeholder groups | Engagement |
|---|---|
| Regional Chief Executives | Initial meeting with each of the three regional chief executives to discuss our approach to modelling and timelines |
| Strategic stakeholders (Perinatal sub-group) | Strategic stakeholders were invited to three sets of workshops:
|
| Clinical representatives | This was a one-off session to discuss the definition of sickest babies |
| Operational stakeholders (North and East Scotland Health Boards)[3] | Operational stakeholders were invited to three sets of workshops:
|
| Operational stakeholders (West Scotland Health Boards)2 | Operational stakeholders were invited to three sets of workshops:
|
| Regional planners | An introductory meeting was undertaken with the regional planners during project inception. Regional planners were also included in the baseline validation, early impacts, and early implementation workshops with strategic stakeholders. |
The Perinatal Subgroup formed the strategic stakeholders for engagement purposes. Operational stakeholders from each of the in-scope Health Boards were invited to take part in engagement workshops. Each region was asked to nominate operational representatives from a range of professions (including neonatologists, neonatal nurses, AHPs etc.) to attend these workshops.
2.6 Implementation considerations
Throughout the baseline analysis and engagement with stakeholders, feedback was received that related to the implementation of the new model of care. This has been collated and synthesised and as such, implementation considerations have been included within this report. These can be reviewed by Scottish Government, regional planners, and individual units to inform implementation plans on the future model of care.
2.7 Limitations
Due to the compressed timeframes available for data collection, individual sites had limited time to extract and validate the neonatal data. In many cases this also required a degree of manual collation and calculation to complete datasets, which are also reliant on accurate recording of information on local systems.
There have been some differences in extraction approaches across units and variability in the quality and coverage of data received. We have commented on individual baseline outputs where we believe this to have caused a material difference to result and validated this through the modelling stages via stakeholder workshops. Examples include one site not being able to provide granular data on neonatal interventions and another only being able to provide data pertaining to the sickest and/or smallest babies (rather than all neonatal admissions) in the time frame available. A full list of data limitations can be found in Annex A.
Other limitations relate to the scope of the analysis. Existing LNUs and SCUs in Scotland fell outside the scope of this report. The modelling includes an assumption that activity in these units will not change under the new model. A full analysis of maternity capacity was also not included within the remit of this commission, but the additional demand on the three future NICU sites has been estimated, recognising that neonatal units very much rely on capacity for maternity admissions.
Workforce requirements have also been excluded from this demand and capacity modelling exercise. This will form part of the regional implementation plans beyond the commission of this modelling.
Contact
Email: thebeststart@gov.scot
There is a problem
Thanks for your feedback