Flu and COVID-19 vaccination programme 2023-2024: equality impact assessment
Findings from an equality impact assessment of the 2023-to 2024 Flu and COVID-19 Vaccination Programme (FVCV).
Impact Assessment for winter 2023-24
Age
34. The FVCV vaccination programme approach is guided by JCVI advice on prevention of severe illness and mortality and the functioning of health and social care systems. This prioritises people primarily due to their age and other clinical risk factors.
35. Data analysis continues to show that COVID-19 disproportionately affects those in older age groups. Older people undergo hospital admissions with COVID-19 at a higher rate than younger people. As of 31 March 2023, people aged 75-84 were admitted to hospital with COVID-19 at a rate of 1,299 per 100,000 population, and for those aged 85 and over, the rate was 2,471 admissions per 100,000 population. This compared to a rate of 208 admissions per 100,000 population for people aged 45-64[2].
36. Those most at risk as a result of their age have been prioritised by the JCVI and offered vaccination early throughout the various phases of the programme.
37. Evidence shows that younger people with no underlying health conditions are less at risk from severe illness, hospitalisation and death from COVID-19. Those under the age of 50, with no underlying health conditions, are not being offered a COVID-19 booster vaccination this winter.
| Cohort | Flu% uptake | COVID % uptake |
|---|---|---|
| Aged 65+ | 85.5% | 90.6% |
| Older Care Home Residents | 89.4% | 90.5% |
| Aged 50 to 64 | 55.4% | 66.0% |
| Clinically at risk (Flu: 18 to 64 year olds at higher risk of flu / COVID-19: 5 to 64 year olds) | 56.9% | 63.8% |
| All health care workers | 55.7% | 57.7% |
| All health and social care workers | 46.9% | 47.9% |
| All social care workers | 36.4% | 40.5% |
38. What is encouraging is that through the course of the pandemic uptake in the highest age groups has repeatedly been the highest.
39. Lower vaccine uptake in younger age groups may be driven by their perceived lower risk from COVID-19 and flu, with a considerable clinical focus on those in older age groups or those with underlying health conditions. Communications and marketing materials continue to highlight the benefits of vaccination across all age groups, such that individuals can make an informed choice on vaccination when it is offered to them, especially those with particular clinical risk conditions that place them at greater risk.
40. We have continued to use analysis and feedback from previous parts of the programme to inform and improve how we appoint people. Digital preference and literacy tends to decrease with age, so we have appointed all those aged 75 and over and sent them this appointment via letter. There has been a greater push to encourage more individuals to update their contact preferences during 2023-24 to indicate whether they wish to receive a letter, email or text communications rather than the traditional paper letter invitation for vaccination. This has been promoted at every opportunity. We have retained the National Vaccination Helpline for those who are more comfortable talking to someone, rather than rescheduling online. We have also attempted, where possible, to offer a range of appointment venues and types to cater for older individuals such as housebound vaccinations and local venues, including community pharmacies.
41. Some planned FVCV evaluation activities in 2023-24 include:
- Analysis of booking methods (e.g. prompts vs scheduled appointments; digital comms v letters; reminders) and delivery of models to support maximal and equitable uptake
- Evaluation of who engages in outreach settings, including Scottish Ambulance Service mobile units
- Did Not Attend (DNA) survey in partnership with National Contact Centre; and
- National survey of Health and Social Care Worker attitudes and experiences of the winter programme (Jan/Feb 2024)
42. Primary schools in Scotland have successfully supported the flu immunisation programme since 2014. Flu can be serious and life-threatening, even for healthy children. The aim is to reduce the risk of children and young people spreading flu to friends and family and to help prevent the flu virus adding additional strain on our NHS services through the winter. To support this aim, the flu eligible groups were expanded in 2021 and remain in place for the winter 2023-24 programme.
Disability
43. In 2021, almost half (47%) of the adult population reported living with a long-term health condition. Women were more likely than men to report having such a condition (52%, compared with 43%). This proportion increased with age for both men and women. Just over a quarter (26%) of all adults aged 16-24 reported living with a long-term condition, rising to almost three-quarters (74%) of those aged 75+. In 2021, a third (34%) of adults reported living with a limiting long-term condition, more than two-thirds of those with any long-term condition. The proportion of adults living with a limiting long-term condition increased with age. Less than one-in-five (18%) of those aged 16-24 reported living with a limiting long-term condition compared with three-in-five (60%) of those aged 75 and above. Again, women were more likely than men to report having a limiting condition (39% compared with 30%). 1 in 5 Scots identify as disabled and more than a quarter of working age people report having an impairment[3].
44. Given the considerable proportion of the Scottish population that lives with disability and the significant impact of the COVID-19 pandemic, access to the individual and public health benefits of vaccination are important. People who are clinically extremely vulnerable or have particular health conditions are eligible for a flu and COVID-19 vaccine as part of winter 2023-24. This does not, however, include all people with disabilities and not everyone with pre-existing medical conditions is disabled.
45. The JCVI advice and Green Book definition of those with a learning disability was widened in August 2022 to include all those on the learning disability register[4] and this has remained in place for 2023-24. Scotland does not specifically operate a learning disability register and the reference mainly relates to the register in England. In England, anyone with a learning disability can request that their GP add them to the list, regardless of severity. In identifying those who are eligible in Scotland, we have applied the same criteria to our own data.
46. Programme delivery continues to seek to address specific issues that are more likely to affect disabled people, for example:
- accessible vaccination venues, e.g. for people who use wheelchairs or have sight loss;
- availability of transport assistance;
- availability of information in accessible formats and languages including British Sign Language (BSL);
- elimination of other communication barriers;
- the provision of quieter spaces, allowing more time for appointments, smaller clinics and appropriately trained staff to support the needs of people with Learning Disabilities, Autism Spectrum Disorder (ASD), Sensory Impairments and mental health conditions;
- consideration of the needs of people with mobility impairments or mental health conditions who may be unable to leave their home to attend an appointment;
- provision for the needs of people who may require to attend the vaccination appointment with support (paid/unpaid carer, family member, friend, interpreter, guide support etc.);
- access to digital and non-digital information and services; and
- consideration of the needs of those who may be experiencing anxiety or needle phobia at their appointment.
47. Learning and engagement with stakeholders throughout the programme has led to a commitment of embedding more of the above measures and making translation and transport information easy to access. The collection of disability data to support the design and monitoring of Scotland’s public health approach to immunisation is also being considered.
Sex / Gender
48. Data analysis continues to show that COVID-19 disproportionately affects men in terms of hospital admissions. As at 31 March 2023, men were admitted to hospital with COVID-19 at a rate of 345 admissions per 100,000 population, and for women the rate was 330 per 100,000.
49. Consideration has been given through the programme to the location, appointment timings and travel to vaccination clinics to ensure people with different working and caring responsibilities are not excluded. Information materials make it clear that individuals can bring their children or people they care for to their appointment.
50. Vaccination uptake data has continued to be monitored. Data suggests that uptake of the COVID-19 vaccine does not vary greatly by sex, with both female and males showing 75-80% uptake. As we descend in age groups, uptake among men is lower than women between the ages of 16 and 39 for doses one, two and three (data correct as per Public Health Scotland (PHS) Dashboard[5], as of 31 July 2023).
Pregnancy and Maternity
51. In December 2021, following the recognition of pregnancy as a risk factor for severe COVID-19 infection and poor pregnancy outcomes during the Delta wave, pregnancy was added to the clinical risk groups. Pregnant women in their 1st, 2nd or 3rd trimester remain eligible for both vaccines this winter.
52. Uptake within the pregnant women group remains challenging and lower than expected.
53. In order to maximise uptake and protection for pregnant women as part of the Winter 2023 programme, the preferred approach to the vaccination is for co-administration of both flu and COVID-19 vaccines by midwifery teams at existing appointments. The Chief Midwife of Scotland continues to endorse this approach and where possible Health Boards are asked to offer co-administration with seasonal flu within their local arrangements, where practicable. In areas where this is not possible, midwives are given training and are expected to encourage pregnant women to access vaccination via community clinics.
54. The data on COVID-19 vaccinations given to pregnant women that was last published on 28 September 2022 (providing data for up to the end of July 2022) came from the COVID-19 in Pregnancy in Scotland (COPS) study. COPS was a time-limited study set up to conduct surveillance and research on COVID-19 infection and vaccination in pregnancy during the pandemic. The study closed at the end of September 2022.
55. To support ongoing monitoring of vaccination in pregnancy, since the COPS study ended PHS has been working to establish the Scottish Linked Pregnancy and Baby Dataset (SLiPBD). SLiPBD will provide regularly updated information on all recognised pregnancies in Scotland, which can then be used to identify vaccinations given in pregnancy. We expect SLiPBD to be able to publish this data next year.
56. Specific pregnancy leaflets have been updated for winter 2023-24 and provided to maternity settings. There is also an updated pregnancy resource on NHS Inform: Pregnancy and the coronavirus vaccines | NHS inform
Sexual Orientation and Trans Gender
57. No differential impacts have been identified.
Race and Ethnicity
58. The PHS Health Inequalities Impact Assessment (HIIA) and PHS FVCV programme evaluation report 2022 identified a number of potential issues affecting access to vaccination and uptake relating to race and ethnicity. This included lack of trust in organisations promoting the vaccine; lack of available information which is culturally and linguistically appropriate; lack of flexibility in vaccine appointments and perceived harms from vaccine promoted via social media (especially in the Polish community).
59. The programme approach has been to consider these issues and to constantly adapt to intelligence and data regarding uptake in consultation with third sector and community groups. Initial activity included:
- Informed consent materials are available in 25 different languages on NHS Inform and in accessible formats such as Easy Read, BSL and audio
- QR codes on all vaccination appointment letters which direct individuals to this information so they are fully informed ahead of their vaccine.
60. The PHS and FVCV report recommended that Scottish Government, Public Health Scotland, and local Health Boards should continue to work in partnership with trusted voices and stakeholders representing minority ethnic communities to better understand the distinct 21 needs of different groups, reduce practical barriers, and inform service improvements.
61. For winter 2023-24, PHS will continue to provide a breakdown of vaccination uptake data by ethnicity and deprivation. Boards will be able to see this updated data weekly, with the data being publicly available from the middle of the programme. This in-depth analysis will assist Scottish Government and Health Boards in monitoring the impact of Boards inclusivity plans and how they can more effectively target resources to reduce health inequalities amongst particular groups and geographical areas.
62. Work was carried out by Dr Josephine Adekola of Glasgow University in 2022 which looked at the African, Caribbean and Black communities’ experiences during the COVID pandemic and their attitudes towards COVID-19 vaccines also involved several Health Boards this year when the film of the research was shown in their areas and facilitated Q&A sessions with health board staff and community members. All boards involved have reported that they had made stronger connections with the community as a result of this work.
63. Data reveals that from the beginning of the programme, uptake among African, Black, Caribbean, Polish and Gypsy/traveller communities has been significantly lower than the general population, with individuals from these communities almost a third less likely to take up the offer of vaccination.
Religion or Belief
64. From the programme outset, SG and PHS have engaged with faith leaders and representatives asking for support to promote the vaccination programme within communities as well as seek their advice on any adaptations to delivery that should be made to enable people to receive and take up their offer of vaccination. A number of faith leaders have publicly endorsed the vaccination programme.
65. The PHS HIIA identified vaccine ingredient information and the potential to hold vaccination clinics in places of worship as two important aspects of confidence of the programme among particular religious groups. PHS has also produced information on vaccine ingredients.
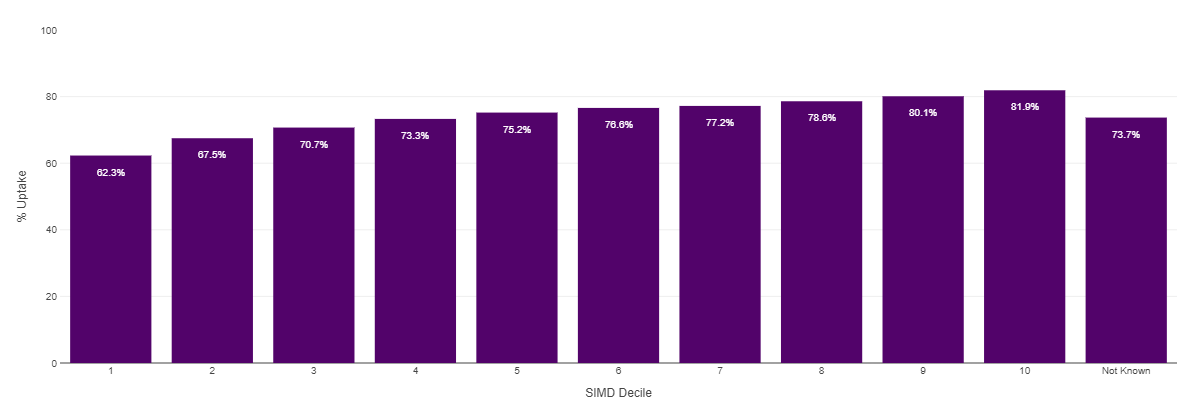
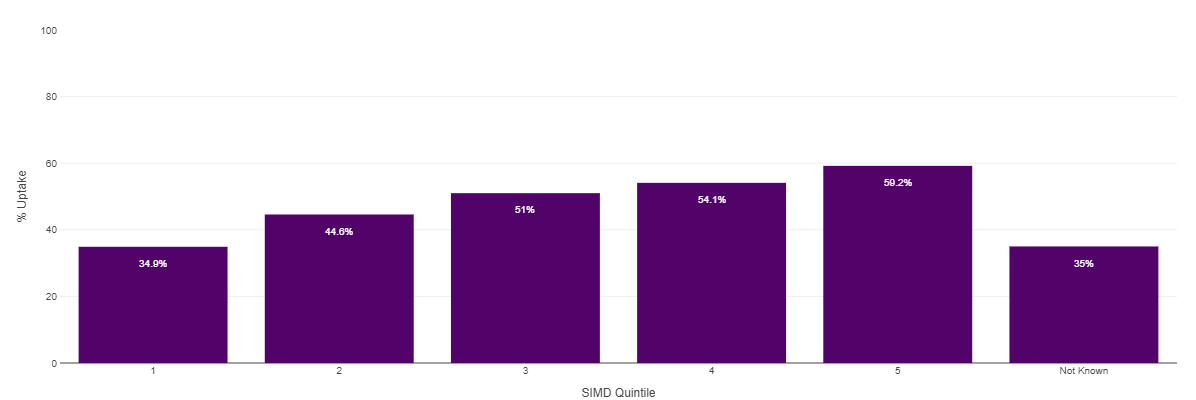
Deprivation
66. Figures across the pandemic continue to show that uptake decreases as we move down the Scottish Index of Scottish Multiple Deprivation (SIMD) categories (10 being the most affluent areas and 1 being those areas with the highest levels of deprivation). Health Boards continue to try and reduce this inequality through a range of measures including locating clinics in areas of highest deprivation, for ease of access, working with Deep End GP practices to encourage uptake within their catchment areas and by operating pop up and mobile clinics within particular communities.
67. Some of the measures that were available at the height of the pandemic, such as financial support for transport to clinics, or free taxi services are now no longer available. Boards do offer some support for individuals, as they do for other health interventions, but these are determined at a local level.
Substance Misuse & Homelessness
68. This year Boards have continued to work with a range of third sector partners for example, Local Authority Resettlement Teams, Addictions Teams, and Homeless Teams, including charities, foodbanks and organisations that are familiar to those living in the most deprived areas with a lower vaccination uptake, to encourage those who are identified as immunosuppressed and eligible to come forward for vaccination and direct them to their nearest vaccination drop in clinic.
69. Some Boards are working locally with homeless nurses to offer vaccinations in homeless hostels. The nurses have agreed to discuss vaccinations ahead of the vaccinations teams visiting and are getting support from the local vaccination team, to access resources.
70. All Health Boards are offering drop in clinics during winter 2023-24 to encourage people to come forward for vaccination at a time that suits them. It is hoped this will also encourage groups such as those experiencing homelessness and substance users to come forward.
71. Some Boards have continued proactive calling of people who are eligible and have not yet been vaccinated and have continued the use of the vaccination bus to target areas of low uptake targeting areas of deprivation and those who lead more transient lifestyles so that they can easily access vaccination should they wish to do so.
Other Factors Impacting on Equality
72. Progress on the COVID-19 vaccination programme has been unprecedented and every opportunity has been made to take a national collective approach and improve the offer to the public, for example, the introduction of digital systems in addition to letters and phone line. In addition to the above impact assessments, specific approaches have been taken to ensure that the following eligible groups are not excluded from the programme as a consequence of their particular circumstances.
Prisoners
73. For winter 2023-24 all prisoners who fall into any of the eligible groups will be offered COVID-19 vaccination. All Scottish prisoners are eligible for the flu vaccine. Different Boards have different arrangements in place with individual prisons. Some are delivering the vaccination programme through outreach teams that visit the prison, whereas others are being delivered in-house by prison healthcare teams. PHS continues to produce updated tailored leaflets to support informed consent and provide information on what to expect after your vaccination for the prison population for the 2023 programme.
74. Prisoner uptake data is in progress of being collected and PHS teams are working with Scottish Prison Service to receive and collate this data which will be released in 2024.
Refugees and asylum seekers
75. A number of people from Afghanistan have arrived in Scotland under the Afghan Relocation and Assistance Policy (ARAP) scheme. This was an emergency response to the situation in Afghanistan, whereby people who worked for British institutions, particularly the military, were offered relocation to the UK because of the risks they faced as a result of their service to the UK. Although many of the people coming to the UK speak good English, this is not universal, particularly among family members. COVID-19 vaccine information is available on NHS Inform in the two main languages used in Afghanistan, Dari and Pashto. Various Health Boards have established links with colleagues in primary care, local authorities and HSCPs to support development of pathways for eligible members of Afghan resettled families.
76. Scotland is a super sponsor for those fleeing the conflict in Ukraine. PHS have developed assets and materials in Ukrainian that have been distributed to resettlement teams. They have also been distributed to the two cruise ships docked in Edinburgh that are housing some of those displaced by the war in Ukraine up until summer 2023. NHS Lothian is working with the refugee and resettlement teams to facilitate vaccination for this community.
Contact
Email: ImmunisationPolicy@gov.scot
There is a problem
Thanks for your feedback