My Health, My Care, My Home - healthcare framework for adults living in care homes: annual progress report September 2023
This is the first annual progress report for My Health, My Care, My Home. It looks back on the past year, highlighting some initiatives that have aided the delivery of the Healthcare Framework’s recommendations. It also references others that started prior to June 2022 that have since progressed.
The Multi-Disciplinary Team (MDT)
The benefits of a multi-disciplinary approach to care are clear. Having an effective, proactive MDT in place is the catalyst to providing better outcomes for people living in care homes and is the foundation of implementing the overall vision of the framework.
The framework has a strong focus on MDT working, which places the individual at the centre of the MDT, and we are delighted that there are many examples of this happening across the country, some of which are highlighted below.
In February 2022, NHS Lanarkshire began a Care Home MDT pilot. Initially staff working in the care homes and GP practices identified patients new to living in the care home who were deteriorating or had complex needs. The care home liaison nurse and pharmacist reviewed the patient in collaboration with care home staff, completing a comprehensive assessment, accessing GP records and clinical portal with support as required from a Care of the Elderly Consultant. They also reviewed the individual’s assessments and care plans to produce a summary for the MDT to consider.
As of March 2023, this has resulted in 40% of residents reviewed having one or more medications that are linked to increased falls risk stopped. In June 2023 the pilot began to roll out to all new residents admitted to care homes in three localities. The MDT has continued to work collaboratively with the care home staff, assisting with care planning and introducing ReSPECT (Recommended Summary Plan for Emergency Care and Treatment). The team have now joined up with Social Work to attend the residents’ 4-6 week review in the care home.
Over the past year a care home in Perth and Kinross have been holding fortnightly virtual MDT meetings. These meetings involve the care home manager, the care home support workers, the GP, a specialist neurology nurse and, when required, a psychiatrist and social worker. Feedback from those involved has been very positive:
“The benefit of these meetings is that we can meet to discuss the residents, any concerns, and ideas for improvement of care. As the meetings are pre-arranged we are all able to attend and give the meeting our full attention. It gives an opportunity to speak to other professionals, to get their input, ideas and support to best help the resident in the care home. These MDT meetings help ensure we are providing a high quality of care and offering a person-centred approach so that residents can maintain a good quality of life.”
Senior Home Manager, Balhousie Rumbling Bridge
“As the MDT's are regular it’s easier to plan and discuss any non-urgent issues. This makes the best use of time and cuts down on contacts for the care home between the HD Specialists and the GP. The MDTs ensure I am up to date on where the patient is at in terms of their care, current medications, health issues and so I am then able to plan my support around this.”
Specialist Nurse, NHS Tayside
“By sharing our knowledge of the patients and their medical conditions, we are able to plan care more effectively. We can then agree who would be the best person to take forward any actions, referrals or discussions with the patients and/or their families. Due to the MDT it is easier to have regular ACP discussions. This ensures the patient’s wishes are respected and the ACP is agreed and shared across all relevant systems.”
Huntington’s Disease Specialist, NHS Tayside
Stirling and Clackmannanshire HSCP have developed a team of care home liaison nurses who work across all the care homes and GP practices within the area, assessing residents and providing advice and support for both the care home team and the GP practices.
Other areas of Scotland have recruited Advanced Nurse Practitioners (ANPs) to provide direct support to care homes. One example of this is Fife HSCP, who now have ANPs in each of their seven local clusters that work alongside the GP practice and the care home and are able to respond quickly to the urgent healthcare needs of people living there. This provision of proactive urgent care can reduce the number of GP visits required to care homes. Their data shows that there were 47% less Emergency Department unplanned attendances from care homes between October 2022 compared to October 2021, and 54% less inpatient admissions over the same period.
Dundee HSCP has introduced an Urgent Home Visiting Team that has direct contact with GP practices and will conduct all urgent care visits to care homes as well as being able to prescribe ‘just in case’ medication. The team supports care home staff to identify people approaching end of life and works closely with multi-disciplinary colleagues to support residents, their relatives, and care staff to prepare for and deal effectively with supporting symptom management and end of life care. To provide continuity, they also plan routine visits to follow up on some actions. Between March and April 2023, the team made 931 visits to care home residents. From September 2023 this model will cover all GP practices in Dundee.
General Practitioners are an important part of the MDT, and the framework highlighted the benefits of close relationships between individual GP practices and care homes. The framework highlighted that care home staff can encounter difficulties when working with several different GP practices, as they each have different ways for requesting advice, visits, and prescriptions.
We attended the Scottish Primary Care Leads group in May 2023 and were able to hear about other work that is taking place in this area. We discussed ‘local enhanced services’ (LES) in relation to care homes, which provide additional funding to supplement services already offered within the core GP contract. There is a desire in some areas to review their LES that relate to care homes in line with the aspirations of the 2018 GP contract and the ambitions of this framework.
Data on alignment between care homes and named GP practices
Public Health Scotland data shows that, as of 1 April 2023, there were 905 GP practices in Scotland, and the Care Inspectorate Datastore indicates that, as at 31 March 2023, there were 1037 adult care homes registered in Scotland.
While the data shows 905 GP practices, not all of these will have patients registered that are living in care homes. Similarly, some of the 1,037 care homes will provide respite or step-down facilities, so patients only stay temporarily and then return to their usual home address and GP practice.
To gain an insight into the number of care homes currently aligned to named GP practices, we obtained data from National Services Scotland (NSS). This data identified that, as of March 2023, 64% of care homes in Scotland are aligned to either 1 or 2 GP practices. Annex D provides a breakdown of this data by Health Board. Moving forward we will continue to receive quarterly data from NSS relating to the number of GP practices that are linked to each care home.
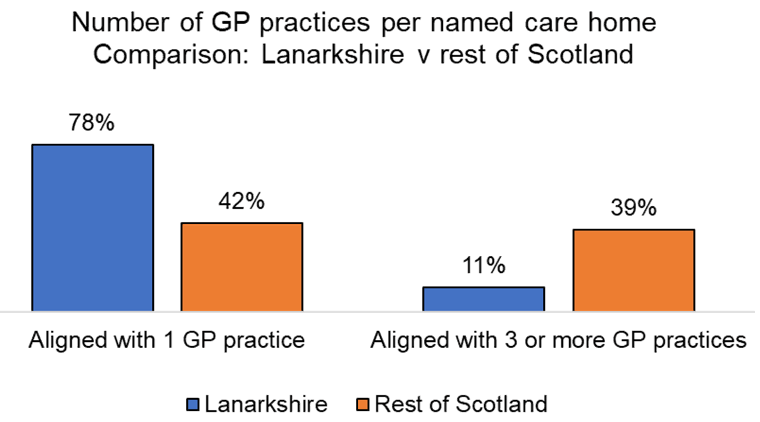
Many HSCPs have reported success from aligning care homes with individual GP practices. This is true in Lanarkshire where a LES has helped to align most care homes with a specific GP practice. 78% of care homes in Lanarkshire are currently linked with a single GP practice, providing care for all the people living in the care home; and only 11% of Lanarkshire care homes are required to engage with 3 or more different GP practices. This compares with the national figures of 45% and 36% respectively. They report subsequent benefits in working relationships and improved outcomes for people living in care homes with a reduction in unnecessary admissions to hospital.
We recognise that it will not be possible, practical, or desirable to align every care home in Scotland with an individual GP practice, but we do see it as essential that close working relationships are developed between every care home and the GP practice(s) covering them.
Contact
There is a problem
Thanks for your feedback