Mental health and wellbeing strategy, delivery plan and workforce action plan: human rights impact assessment (HRIA)
Assessing the impact of the mental health and wellbeing strategy, delivery plan and workforce action plan on human rights in Scotland
Non-discrimination and equality
All forms of discrimination (such as age, gender, sexual orientation or ethnicity) in the realisation of rights must be prohibited, prevented and eliminated. It also requires the prioritisation of those in the most marginalised or vulnerable situations who face the biggest barriers to realising their rights.
Anyone who experiences mental ill health may be vulnerable and therefore fall under the umbrella of the strategy. However, there are certain groups that may be particularly vulnerable.
There are people whose illness is such that they require to be treated in hospital on a short or long term basis. Sometimes this cannot be done on a voluntary basis, and people can be subject to compulsory measures of care and treatment in hospital or in the community under mental health legislation. It is essential that these groups retain the same rights and entitlements as others and that appropriate safeguards exist to protect and uphold rights. Anyone carrying out functions under the Mental Health (Care and Treatment) (Scotland) Act 2003 must have regard to the over-arching principles of the Act which include taking into account the wishes and feelings of patients and carers, using options of least restriction and maximum benefit and that of reciprocity where society imposes an obligation on someone to comply with a programme of treatment of care, there should be the same obligation on health and social care authorities to provide safe and appropriate services, including ongoing care once the individual is no longer subject to compulsory measures.
Social and structural inequality in society means that those who face the most significant disadvantages in life also face the greatest risks to their mental health. This includes marginalised groups who experience discrimination, racism or exclusion (social, political, economic or environmental) solely based on age, race, sex, sexual orientation, disability or other characteristics protected by the Equality Act 2010. There are also other groups, such as veterans, refugees, children, young people, adults and families who are care experienced, people affected by substance use or those experiencing abuse or homelessness and those engaged in the justice system. People in prison often have a combination of mental and social care needs, arriving in prison disproportionately from the most deprived areas in Scotland, and with higher mental health needs relative to the non-prison population. Many people in these marginalised or hidden groups experience discrimination from parts of society, creating multiple discrimination and leading to significant marginalisation. This can be traumatic and cause long-term damage to their mental health and considerable adverse mental health impacts beyond those that the rest of the population face.
Poverty is the single biggest driver of poor mental health, and we know that people living in poverty carry a higher risk of suicide, as do those who are unemployed or socially isolated. Many people also face the additional barrier of digital exclusion, meaning it is harder to access advice, support and services.
In many cases, these same groups of people also often experience less access to effective and relevant support for their mental health. When they do get support, their experiences and outcomes can be poorer. These inequalities in mental healthcare can exacerbate mental health inequalities.
Disabled people are more likely to report lower mental wellbeing than those with no condition and are amongst those who need support and services to be accessible and inclusive in a range of formats, including non-digital. This includes people with learning disabilities, those with sensory loss and those with a long-term physical health condition. A large proportion of autistic people also experience mental ill health in their lifetime.
Women and girls are disproportionately impacted by poverty, which can lead to social isolation, anxiety, depression and stress. Greater caring responsibilities and the everyday threat of violence against women and girls can also adversely impact mental health. Childbirth is also associated with an increased risk of mental ill health in mothers.
Periods of transition often put extra stress on children and young people's pre-existing resilience and coping strategies. The late teenage years are a point when mental wellbeing can decline, particularly for young women, and can also be the point of onset of serious mental illness. Teenage years are also a stage in life where the increased use of online communities and social media can impact mental health, especially for young women. Experiences of bullying, harassment and abusive behaviour put young people at higher risk of poor mental health.
Scotland also has an ageing population. The proportion of 'older adults' (65 years old and over) in the population has increased from 16% in 2000 to 19% in 2020. This is expected to continue increasing over the next decade, putting more pressure on public services. Older adults, particularly those living in remote, rural and island areas, are more likely to experience loneliness and can also face barriers in accessing support and services, exacerbated by a lack of access to transport. Research from both NHS Grampian and Scotland's Rural College highlights the disproportionately higher rates of depression amongst agricultural communities, with suicide rates amongst farmers among the highest of any occupational group.
Experiencing minority stress, racism, discrimination and trauma has a significant negative impact on mental health and wellbeing and can disproportionately impact lesbian, gay, bisexual, transgender and intersex (LGBTI) people, minority ethnic groups, and disabled people. LGBTI and minority ethnic people also have reported that staff can lack cultural competency, sensitivity and understanding of their specific needs.
Evidence suggests that only around half of veterans experiencing mental health problems seek help. Stigma is one of the main reasons for this, and levels of help-seeking are particularly low in those with post-traumatic stress disorder. The specific needs of veterans must be taken into account when planning support and services.
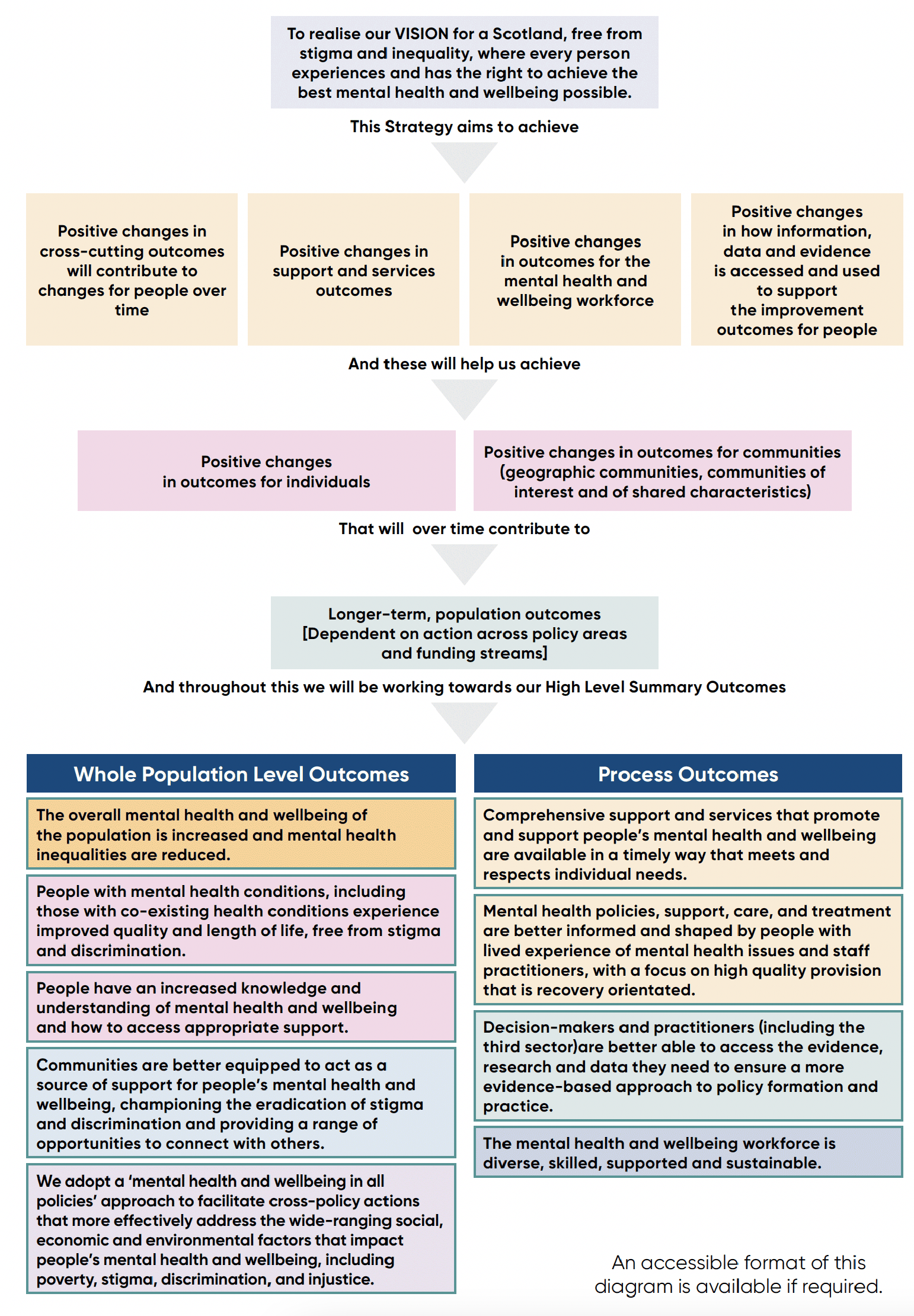
We want to be clear about what this Strategy is trying to achieve.
- Positive changes in cross-cutting outcomes will contribute to changes for people over time
- Positive changes in support and services outcomes
- Positive changes in outcomes for the mental health and wellbeing workforce
- Positive changes in how information, data and evidence is accessed and used to support the improvement outcomes for people
Specifically, the actions in the Delivery Plan and Workforce Action Plan will lead to that change happening in a sustainable way.
To do this, we have developed a set of outcomes. These are the differences or changes that we want to see as a result of this Strategy. The outcomes we aim for are the same for everyone, although the actions we need to take to get there will likely differ for different groups. We will use these outcomes to help monitor and evaluate progress as this Strategy is implemented.
The aim of the Strategy is to deliver positive outcomes for people. There are various actions which could be argued support the relevant rights and safeguards of human rights in the Delivery Plan and Workforce Action Plan.
- Promote positive mental health and wellbeing for the whole population, improving, understanding and tackling stigma and discrimination.
- Promote and Prevent mental health issues occurring or escalating and tackling underlying causes and inequalities wherever possible.
- Promote, Prevent and Provide mental health and wellbeing support and care, ensuring people and communities can access the right information, skills, support, services and opportunities in the right place, at the right time.
Through the actions laid out in the Delivery Plan for this Strategy, we will seek to:
- Tackle mental health stigma and discrimination where it exists and ensure people can talk about their mental health and wellbeing and access the person-centred support they require.
- Improve population mental health and wellbeing, building resilience and enabling people to access the right information and advice in the right place for them and in a range of formats.
- Increase mental health capacity within General Practice and primary care, universal services and community-based mental health supports. Promote the whole system, whole person approach by helping partners to work together and removing barriers faced by people from marginalised groups when accessing services.
- Expand and improve the support available to people in mental health distress and crisis and those who care for them through our national approach on Time, Space and Compassion.
- Work across Scottish and Local Government and with partners to develop a collective approach to understanding and shared responsibility for promoting good mental health and addressing the causes of mental health inequalities, supporting groups who are particularly at risk.
- Improve mental health and wellbeing support in a wide range of settings with reduced waiting times and improved outcomes for people accessing all services, including Child and Adolescent Mental Health Services (CAMHS) and psychological therapies.
- Ensure people receive the quality of care and treatment required for the time required, supporting care as close to home as possible and promoting independence and recovery.
- Continue to improve support for those in the forensic mental health system.
- Strengthen support and care pathways for people requiring neurodevelopmental support, working in partnership with health, social care, education, the third sector and other delivery partners. This will ensure those who need it receive the right care and support at the right time in a way that works for them.
- Reduce the risk of poor mental health and wellbeing in adult life by promoting the importance of good relationships and trauma-informed approaches from the earliest years of life, taking account where relevant adverse childhood experiences. We will ensure help is available early on when there is a risk of poor mental health and support the physical health and wellbeing of people with mental health conditions.
The Workforce Action Plan aligns with the five pillar approach from the wider National Workforce Strategy for Health and Social Care - Plan, Attract, Train, Employ, Nurture.
All of the actions in the Delivery Plan and Workforce Action Plan were developed in careful consultation with should ultimately help to promote and uphold human rights around mental health.
Contact
There is a problem
Thanks for your feedback