Health - redesign of urgent care: evaluation - main report
The Redesign of Urgent Care pathway aims to improve patients’ access to urgent care. The evaluation captured patient and staff experiences of the pathway and analysed key urgent care delivery metrics, enhancing our understanding of what is working well and areas for improvement.
2. Background and purpose
2.1 Implementation of the Redesign of Urgent Care programme
For a number of years, NHS Scotland has been under pressure to manage increased system-wide demands for urgent/unscheduled care. Between 2016 and 2019 the total number of annual attendances at A&E Services (including Emergency Departments (ED) and Minor Injury Units (MIU)) increased by approximately 6%, including an increase of over 7% in ED attendances. A significant fall in attendances was observed during the COVID-19 pandemic. However, during 2022 and 2023 ED attendances have returned to near 2016 levels.
| Year | Total attendances (ED and MIU)[2] | % of 2016 | ED Attendances | % of 2016 | MIU/Other attendances | % of 2016 |
|---|---|---|---|---|---|---|
| 2016 | 1,638,170 | 1,340,700 | 297,470 | |||
| 2017 | 1,643,466 | 100.3% | 1,351,856 | 100.8% | 291,610 | 98.0% |
| 2018 | 1,668,799 | 101.9% | 1,371,466 | 102.3% | 297,333 | 100.0% |
| 2019 | 1,740,759 | 106.3% | 1,440,285 | 107.4% | 300,474 | 101.0% |
| 2020 | 1,275,088 | 77.8% | 1,088,651 | 81.2% | 186,437 | 62.7% |
| 2021 | 1,408,117 | 86.0% | 1,224,030 | 91.3% | 184,087 | 61.9% |
| 2022 | 1,531,638 | 93.5% | 1,321,594 | 98.6% | 210,044 | 70.6% |
| 2023 | 1,528,734 | 93.3% | 1,313,263 | 98.0% | 215,471 | 72.4% |
This increase in demand with recognised longer waiting times in EDs, led Scottish Government officials to explore alternative models of care drawing on national (UK) and international models. This included experience from recent models of urgent care developed in Denmark, where most urgent care activity is managed through local hubs, with early access to a senior decision maker and arranged scheduled care, where required. The introduction of ‘Urgent Care Resource Hubs’ was also recommended as part of a National Review of Primary Care Out of Hours Services report from 2015[3]. The purpose being to develop a model for NHS Scotland that aims to schedule urgent care where appropriate, to support care nearer to home and ensure the right care is provided at the right place and right time. The focus patient population for the RUC programme is a sub-group of patients who historically self-presented to A&E services who may be safely managed through patient pathways with alternative entry and exit points to health and care services.
In the midst of the COVID-19 pandemic the RUC programme was created at pace to provide a safer patient experience and an alternative urgent care (RUC) pathway for the cohort of people who would otherwise have directly self-presented to A&E services. This recognised that many patients directly attending A&E services could be more safely and appropriately cared for in their home and community settings, rather than within an acute hospital environment. The redesigned RUC pathway aimed to provide urgent care as near to home as possible by expanding and promoting NHS 24 (call 111), as the preferred initial contact for patients and carers who had an urgent care need. Local Board Flow Navigation Centres (FNCs), with rapid access to a senior decision maker to promote alternative, optimal pathways of urgent care were also established.
As necessary, patients would receive scheduled urgent care to the most appropriate place at the right time, with the aim of improving care experience by reducing unnecessary crowding in A&E services and mitigating ‘surge’ presentations. A Strategic Advisory Group chaired by Calum Campbell, Chief Executive, NHS Lothian and Angiolina Foster, Chief Executive, NHS 24 was established to lead development of the redesign (RUC) programme. A conceptual Framework was developed, supported by all NHS Board Chief Executives with agreed principles for Phase 1[4].
To support this service transformation NHS Ayrshire & Arran agreed to be the first pathfinder site to test the conceptual model and the transferability of the model to a national roll out to all territorial Boards. A Rapid External Review of the NHS Ayrshire and Arran (NHS A&A) Urgent Care Programme Pathfinder site, was published on 30 November 2020[5]. This report considered the impact on the wider system and recommendation to proceed with a national roll-out.
RUC launched nationally on 1 December 2020, on a minimum specification – with a readiness assessment to ensure agreed compliance by all NHS Boards (which all Board Chief Executives signed off). This was described as an incremental or ‘soft launch and relied only on local media messaging to publicise the new urgent care referral pathways, rather than a high-profile nationwide media campaign.
Independent of the RUC Programme, a number of challenges existed within the unscheduled care pathway in relation to workforce, system integration and data quality and availability. The COVID-19 pandemic combined with the RUC Programme have highlighted these areas including staffing pressures within GP OOH services and NHS 24 111.
The RUC pathway aims:
- To increase care nearer to home for patients and carers
- To convert some unscheduled care activity to planned care activity
- To reduce patients who self-present to A&E services
- To reduce overcrowding in A&E services
The RUC pathway includes 3 main Interventions:
- Public messaging to encourage patients and carers to use NHS 24 111 more frequently including routine working hours
- Increase capacity in NHS 24 111 service to:
- manage increased demand and
- create appropriate options and pathways for patients including to Flow Navigation Centres.
- Establish new local Flow Navigation Centres to:
- help navigate patients to most appropriate local services and provide rapid access to a Senior Clinical Decision Maker by phone or digitally to provide self-care advice or as necessary onward referral.
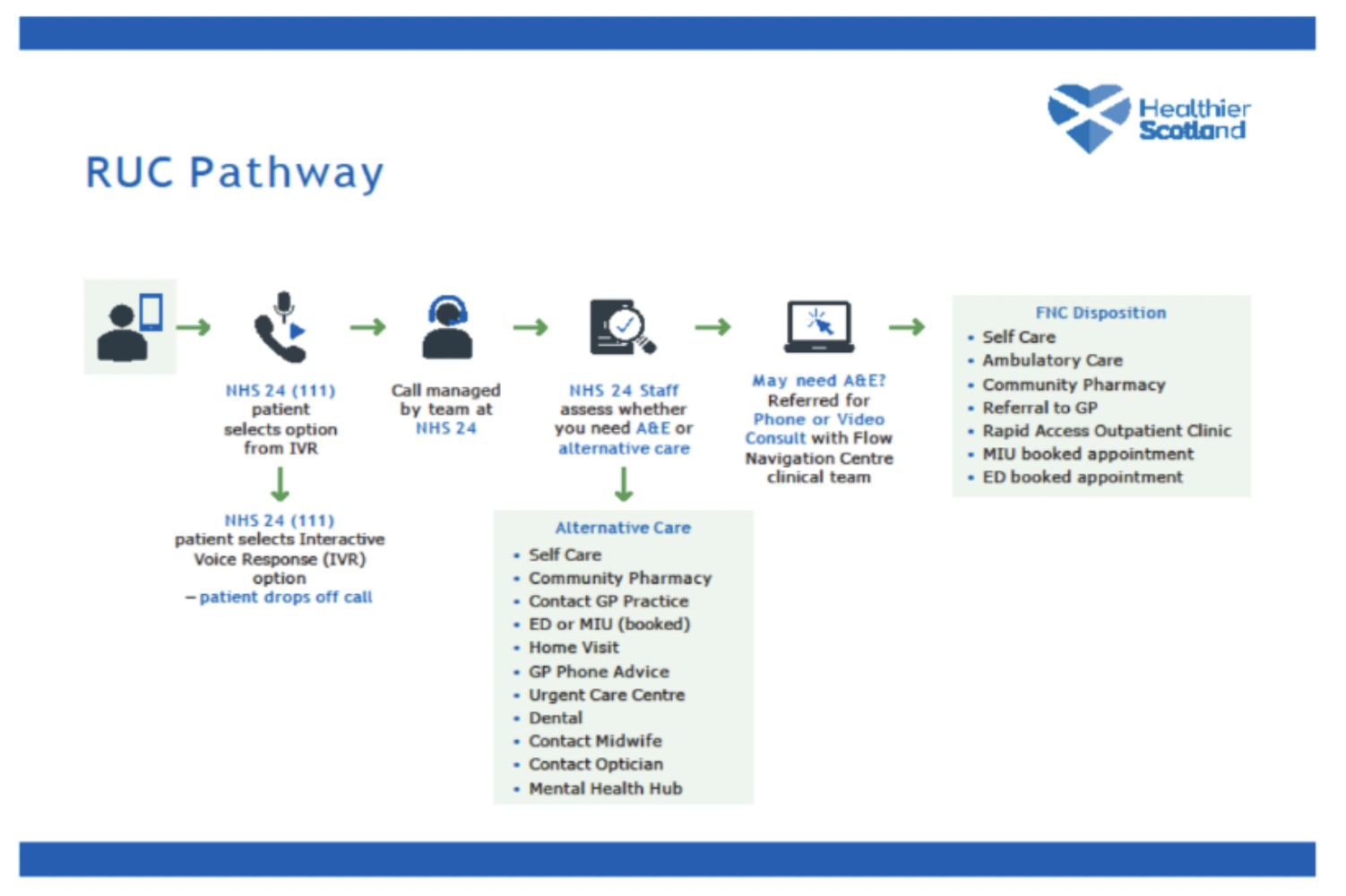
As outlined in Figure 2.1 below, callers to NHS 24 111 (with 111 being a single national number available 24/7) first hear an automated Interactive Voice Response (IVR) message with options to help direct them to the right support. There is an option callers can select if they think they need care for a health concern that is not life-threatening. This option constitutes the RUC pathway.
The NHS 24 111 call handler will assess the patient need with support from a clinical supervisor. The outcomes of the call will depend on the need of the patient and can include self-care advice or advice to attend a General Practice or community service. Some callers will be advised by the NHS 24 111 call handler that they will get a callback from their local Flow Navigation Centre.
Flow Navigation Centres offer clinical triage and virtual assessments with early access to a senior clinical decision maker. The main functions are to maintain care closer to home by providing clinical advice including self-care and for those who require additional services to plan that efficiently. Following the video or telephone consultation from the Flow Navigation Centre, the caller may receive self-care advice, have a booked appointment at A&E services, be advised to attend A&E services or be referred to another service.
The total number of calls to NHS 24 111 increased between 2018 (1,530,135) and 2023 (1,723,884), although the number of calls in 2023 was lower than in 2022 when 1,960,085 calls were offered (see Technical Report, Section 4, Table 1). The proportion of all 111 calls that were to the RUC pathway was 27% (n=525,062) in 2022 and 26% (n=452,343) in 2023. Since this evaluation was commissioned, NHS 24 introduced a virtual queue service at scale in December 2023. This was introduced at the busier times for the service to provide callers with an option for their call to be placed in a ‘virtual queue’.
Two staging reviews were previously completed to evaluate the progress of the RUC pathway[6],[7]. These reviews used activity data to investigate how different pathways of care were being utilised, providing valuable insights in the use of the different services alongside the RUC pathway. Whilst development of the RUC involved stakeholder (including patient) engagement, the staging reviews have included limited evidence from the perspectives of patients. This type of feedback is essential for building a full picture of service quality: most definitions of care quality include patient experience as a component, and insight from patients and staff corroborates the acceptability, sustainability, and person centredness of new interventions.
2.1 Research aims
The aims of this evaluation are to provide an improved understanding of the following:
- Experience of callers to NHS 24 111 who discontinued their call [8]
- Experience of patients who had contact with NHS 24 111 (i.e. gone through the RUC pathway)8
- Experience of staff involved in the delivery of urgent and unscheduled care
- Changes to key Urgent Care delivery metrics, by comparing performance pre and post implementation of the RUC pathway
Contact
Email: dlhscbwsiawsiaa@gov.scot
There is a problem
Thanks for your feedback