Health - redesign of urgent care: evaluation - main report
The Redesign of Urgent Care pathway aims to improve patients’ access to urgent care. The evaluation captured patient and staff experiences of the pathway and analysed key urgent care delivery metrics, enhancing our understanding of what is working well and areas for improvement.
4. Patient Experiences of discontinued calls to NHS 24 111
Background
A relatively high proportion of calls to NHS 24 111 are abandoned before they are answered, particularly during periods of high demand. Data from NHS 24 shows that between June 2023 and May 2024, 16% (n=71,985) of all calls to the RUC (A&E) pathway were discontinued[19]. Whilst many of these callers may call back, others will not, so it’s important to understand what actions people take when they end their call to NHS 24 111. However, it should be noted that this cohort of patients may differ in terms of their sociodemographic characteristics and/or health need to patients that decide to access urgent care services directly without contacting, or trying to contact, NHS 24 111 first.
About the survey[20]
This section outlines the findings from the Discontinued Caller survey, which captured the views and experiences of patients who discontinued a call to NHS 24 111. The aim of this survey was to understand the reasons why respondents decided to end their call to NHS 24 111 before speaking to someone and what action, if any, they took next. The intention was to provide insights into any differences in reported experiences by demographic subgroups but poor quality self-reported demographic data (i.e. where respondents answered the demographic questions about themselves rather than the person needing care) reduced the sample size which affected the ability to present reliable subgroup estimates.
At the end of the questionnaire, there was an open freetext question that asked respondents if there was anything else they wanted to share about their experiences of trying to access urgent care. Of the 387 respondents, 125 respondents (32%) provided a written comment at the end of the survey. Common issues reported related to long waiting times, access to urgent care and the pressure on the service, such as understaffing. Some of the written comments have been presented in verbatim alongside some of the quantitative findings. The comments selected were ones which typically represented other similar comments.
Notes for consideration when interpreting the findings
The length of time since the respondent ended their call could have been up to six months before they completed the survey. This sampling period was selected to ensure a sufficiently sized sample. However, there might have been an impact on recall ability and accuracy for those that had ended a call to NHS 24 111 some months beforehand, particularly for questions that required greater cognitive burden (such as recalling the length of time waited before discontinuing their call). However, ‘Don’t know/Can’t remember’ response options were included at many questions to mitigate the risk of inaccurate responses being provided. Please note in the charts, any response option/breakdown group marked with an asterisk indicates where suppression was required. Where the number of respondents is reported in a heading for a chart, please note this represents the total number of respondents who gave an answer to the question, which is inclusive of suppressed values. Likewise, some charts will not equate to 100% as suppressed responses have been omitted (e.g., Figure 4.8).
4.1 Reason for contacting NHS 24 111
Most respondents (85%, n=330) contacted NHS 24 111 first about their health concern rather than contacting another service, supporting the suggestion that there is a good level of awareness that NHS 24 111 is the entry point to access urgent care. A higher proportion of respondents contacted NHS 24 111 first if they called out-of-hours (89%, n=244), compared to those who had contacted NHS 24 111 in-hours (76%; n=73)[21], which is perhaps unsurprising given the fewer services available out of hours. For details, please see Technical Report, Section 6.1, Table 1.
The main reasons given by respondents for contacting NHS 24 111, rather than another urgent care service, were:
- NHS 24 111 being the most suitable service for their health concern (33%; n=109)
- Needing help out-of-hours (28%; n=93) and
- NHS 24 111 being the easiest service to access (21%; n=68).
For those that contacted another service before calling NHS 24 111, just over half (54%; n=31) had contacted a General Practice. The main reasons respondents subsequently contacted NHS 24 111 was because:
- the service had referred them to NHS 24 111 (33%; n=19),
- their condition had worsened (26%; n=15), or
- their General Practice is often too busy to get a same-day appointment (16%; n=9).
See Technical Report, Section 5, Table 9 for further details.
4.2 Self-reported time waited before discontinuing calls
Around one third of respondents to the survey (34%; n=133) told us that they discontinued their call to NHS 24 111 (made between September 2023 to February 2024) within 10 minutes (Figure 4.1). Approximately half of the respondents (45%; n = 173) reported that they waited 20 minutes or more before discontinuing their call with 105 of these respondents (27% of the sample) reporting they waited for more than 30 minutes before discontinuing their call.
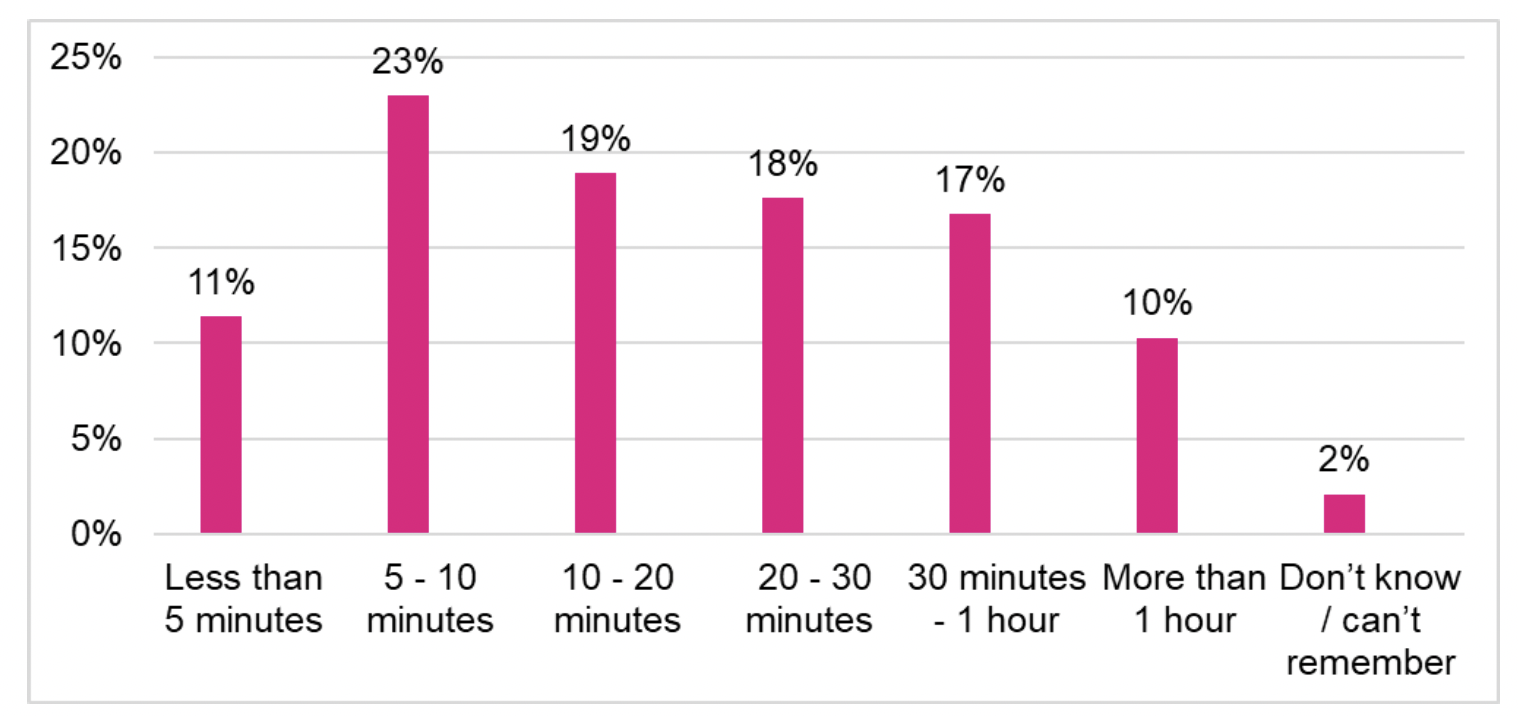
By way of context, NHS 24 111 data showed that between June 2023 and May 2024, the average (mean) time for calls to the RUC pathway to be discontinued was 7 minutes and 45 seconds (Technical Report, Section 4, Table 4). During this period a total of 71,985 calls to the NHS 24 RUC pathway were discontinued, of which just 2,080 (2.9%) did so after 30 mins or more. This reflects some disparity between the perception of survey respondents in relation to their wait time and NHS 24 recorded data which may be explained by numerous factors including (i) different sample groups over a different period of time (June 2023 to May 2024 for NHS 24 111 data compared to February 2024 to March 2024 for the survey) and/or (ii) recall accuracy for survey respondents. Nevertheless, the self-reported data is valuable for measuring people’s experiences and how they felt about the time waiting for their call to be answered, and this may be associated with their subsequent experiences of the care received. For example, as outlined in section 4.7, respondents who reported waiting longer before ending their call were less positive about their overall experience of contact with urgent care services.
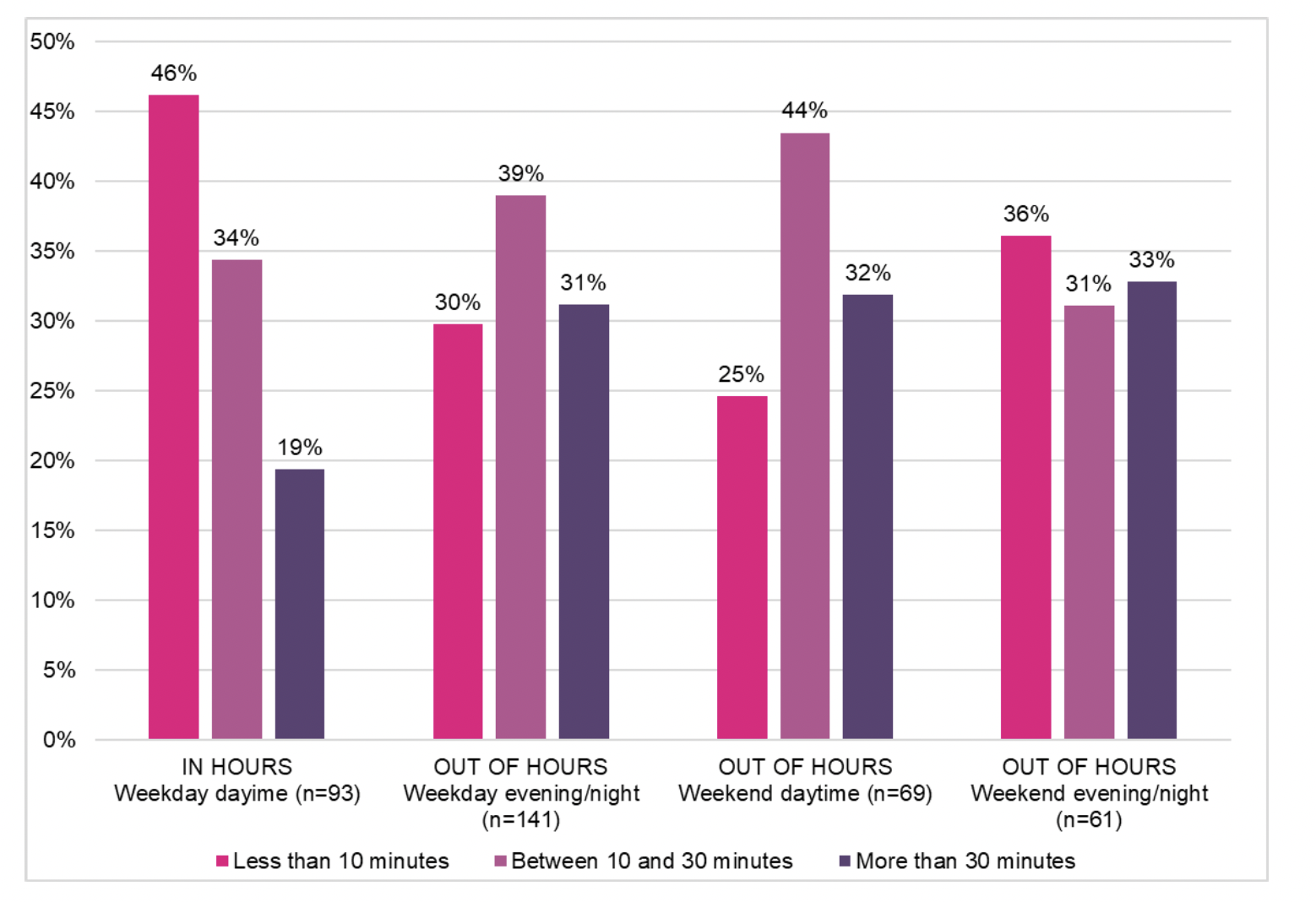
The proportion of respondents that reported waiting for more than 30 minutes before discontinuing their call was higher if they contacted NHS 24 111 out of hours (Figure 4.2). While 19% (n=18) reported a wait of more than 30 minutes before discontinuing their call if they contacted NHS 24 111 in hours (i.e. weekday daytime), this was the case for around one third of patients who contacted NHS 24 111 out of hours.
Of those respondents that provided a written comment at the end of the survey, over one third mentioned long waiting times, with most referring to the length of time for their NHS 24 111 call to be answered, although some mentioned a delay in getting a call back which would most likely refer to the call back from Flow Navigation Centres. Example verbatim written comments are shown in box 1. A few respondents wrote comments to explain that the reason they had ended their call was due to the waiting time for their call to be answered.
Box 1: Example respondent’s written comments on waiting times
“You are waiting for someone to answer you call for too long, sometimes the call cuts out. Other times you give up waiting and hang up.”
“Sometimes the wait is too long yet we are told to contact NHS 24 111 before attending any health service”
“It was disappointing and took a very long time and I didn’t get seen in the end.”
“Phones need answered quicker, if people are panicking then they will hang up.”
“I was told I would have to wait up to 45 mins for my call to be answered. My back was in complete spasm and I couldn’t move. This was the reason for my call as I thought I may have needed some muscle relaxers so I could release my back. So this is why I didn’t wait for my call to be answered.”
“The call times are long, and you then have to wait for someone to call back if you do get through. This is not always helpful if you are very unwell and trying to navigate phone calls. This is why I ended the call and partner took me to A&E.”
“I had to wait a long time before somebody answered so I ended the call to nhs 24 111 so I waited to speak to my doctor surgery the nxt day.”
“The call to 111 took too long to answer, in the meantime the health of my husband deteriorated so I had to call 999 for an ambulance. My experience of the ambulance emergency call was 9/10 of the call to 111 was rated at 1/10”
“I eventually got through, was told a doctor would call me back, this never happened. My mothers health worsened [so] called again, they said no ambulances were available. Had to call my sister to take my 86 year old mother with severe stomach pains to hospital.”
A significantly higher proportion of respondents discontinued their call within 10 minutes if they contacted NHS 24 111 in-hours when compared to those that called out-of-hours (see Technical Report, Section 6.1, Table 2 for full details). The finding that a caller waits for a longer length of time before discontinuing their call if contacting NHS 24 111 out-of-hours may reflect fewer alternative services available at this time.
4.3 Reasons for discontinuing the NHS 24 111 call
Understanding the reason why people end their NHS 24 111 call before speaking to someone at NHS 24 is important in understanding how unanswered call rates could be reduced. The majority of respondents decided to discontinue their NHS 24 111 call because it was taking too long for it to be answered (54%; n=209) and/or the recorded message advised them the call would not be answered quickly (23%; n=90) (Figure 4.3).
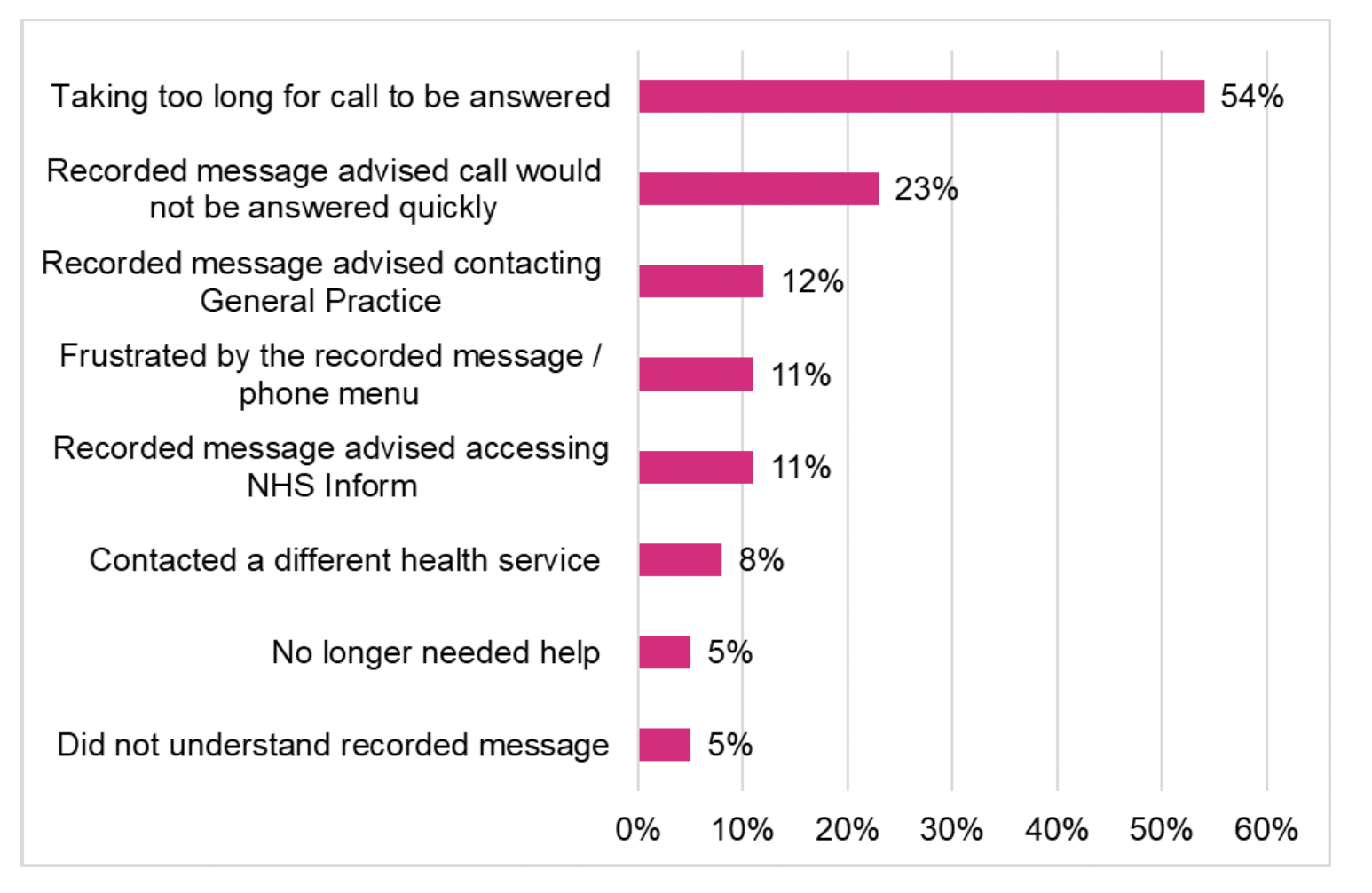
Regardless of the length of time waited, the most common reason given by respondents for ending the call was that it was taking too long for their call to be answered. Unsurprisingly, the proportion selecting this reason was significantly higher if they had waited for more than 30 minutes before discontinuing their call compared to those who waited for less time (See Technical Report, Section 6.2, Table 13).
4.4 Actions after discontinuing the NHS 24 111 call
The RUC pathway aims to lessen the demand for A&E services by reducing the volume of patients who self-present at A&E services. The survey showed 40% of respondents (n=155) reported accessing a secondary care endpoint[22] after discontinuing their call to NHS 24 111; 28% (n=107) attended an A&E or MIU. One in five respondents (20%; n=76) said they called NHS 24 111 again (see Figure 4.4 for full details).
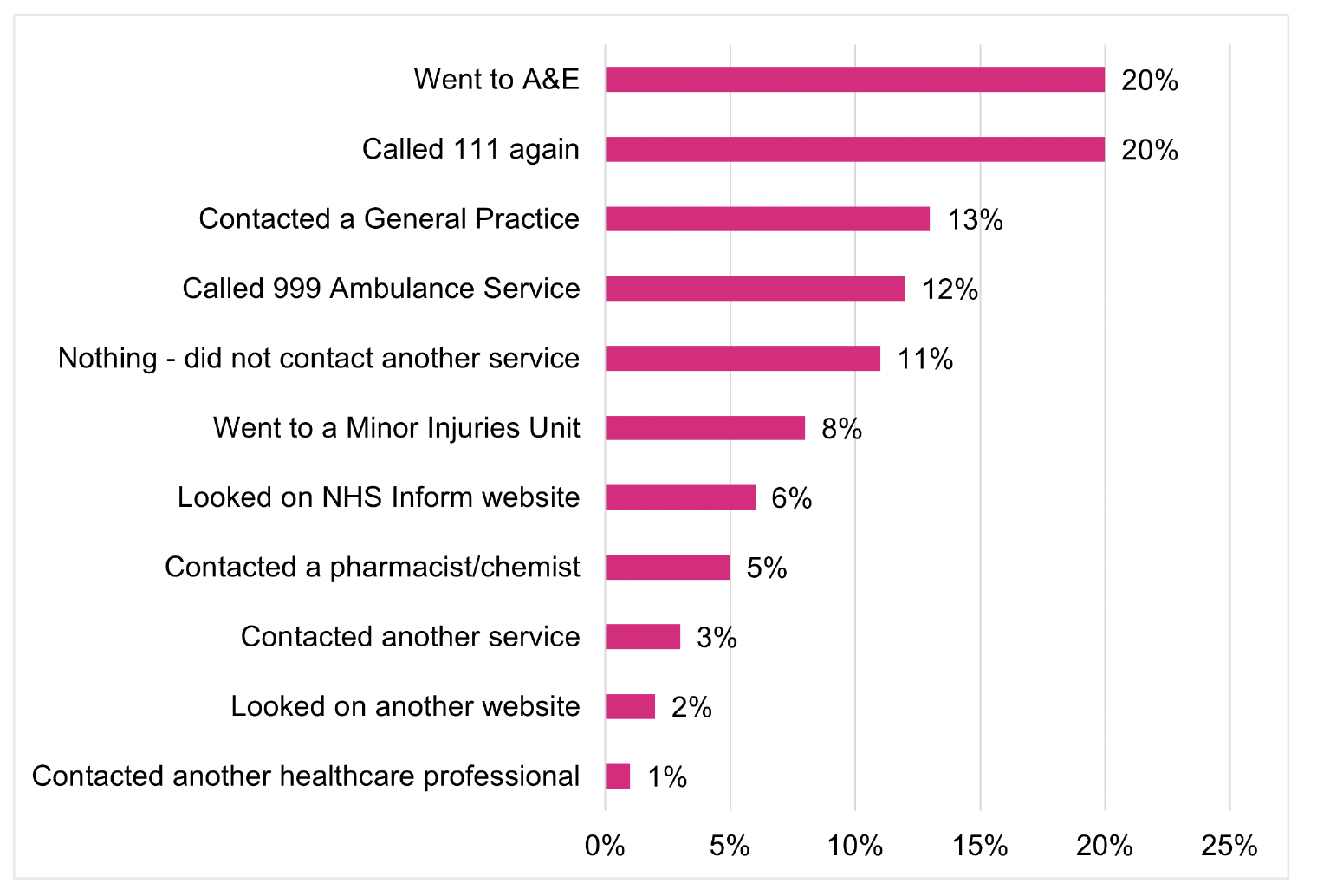
It is important to note that some respondents may have discontinued their call to NHS 24 111 to contact the Scottish Ambulance Service (SAS) after hearing the recorded message which instructs people to call 999 if it’s an emergency. Other findings from the survey appear to support this suggestion to some extent: of those that contacted SAS, 45% (n=21) thought they would get help more quickly from this service (see Figure 4.6) and 60% (n=29) contacted SAS within 30 minutes of discontinuing their call to NHS 24 111 (Figure 4.7).
Figure 4.5 shows the same proportion of respondents (28%) went to A&E or a MIU regardless of whether they discontinued their NHS 24 111 call in-hours (n=27) or out-of-hours (n=77). However, for all other actions taken after calls were discontinued, there were statistically significant differences between those that called in-hours to those that called out-of-hours (see Technical Report, Section 6.1, Table 3 for full details). For example, of those respondents who contacted NHS 24 111 out-of-hours, 22% (n=59) re-contacted NHS 24 111 compared to 16% (n=15) who called in-hours. In contrast, of those who contacted NHS 24 111 in-hours, 15% (n=14) called 999 Ambulance Services after ending their call compared to 11% (n=30) who called out-of-hours.
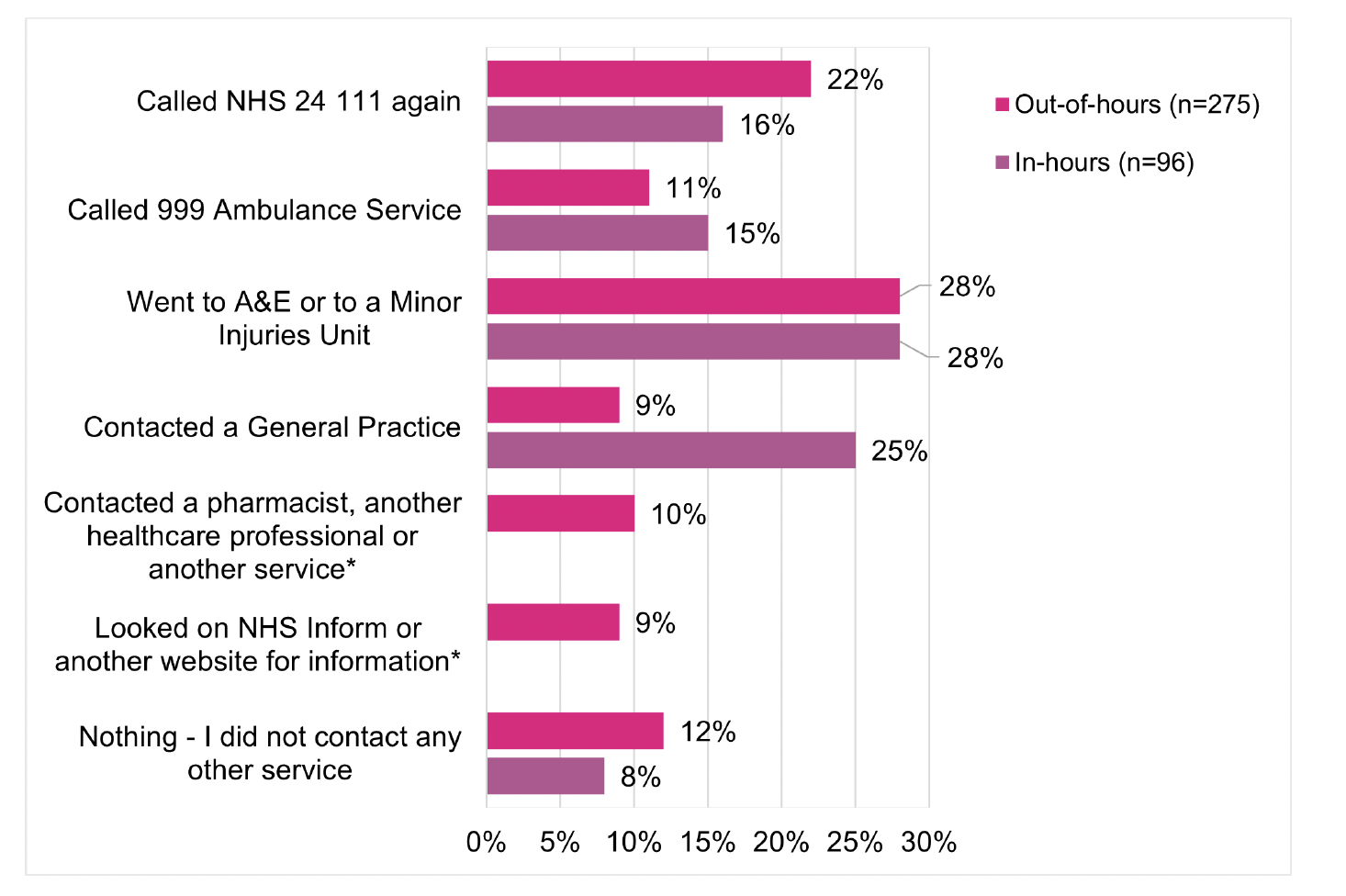
The action taken by respondents after discontinuing their NHS 24 111 call varied by whether they were calling to get help for themselves, for a child, or another adult (Technical Report, Section 6.1, Table 4).
- Of the respondents who called NHS 24 111 for themselves, a significantly higher proportion (19%; n=35) contacted a General Practice after ending their NHS 24 111 call when compared with those calling to get help for a child (7%; n=6) or another adult (7%; n=8).
- Of the respondents who called NHS 24 111 to get help for a child, a significantly higher proportion (39%; n=35) went to A&E or a Minor Injuries Unit after ending their NHS 24 111 call when compared with those calling to get help for themselves (21%; n=39) or another adult (30%; n=33).
- Of the respondents who called NHS 24 111 to get help for another adult, a significantly higher proportion (23%; n=25) called 999 Ambulance Service after ending their NHS 24 111 call when compared with those calling to get help for themselves (10%; n=18) or for a child (6%; n=5).
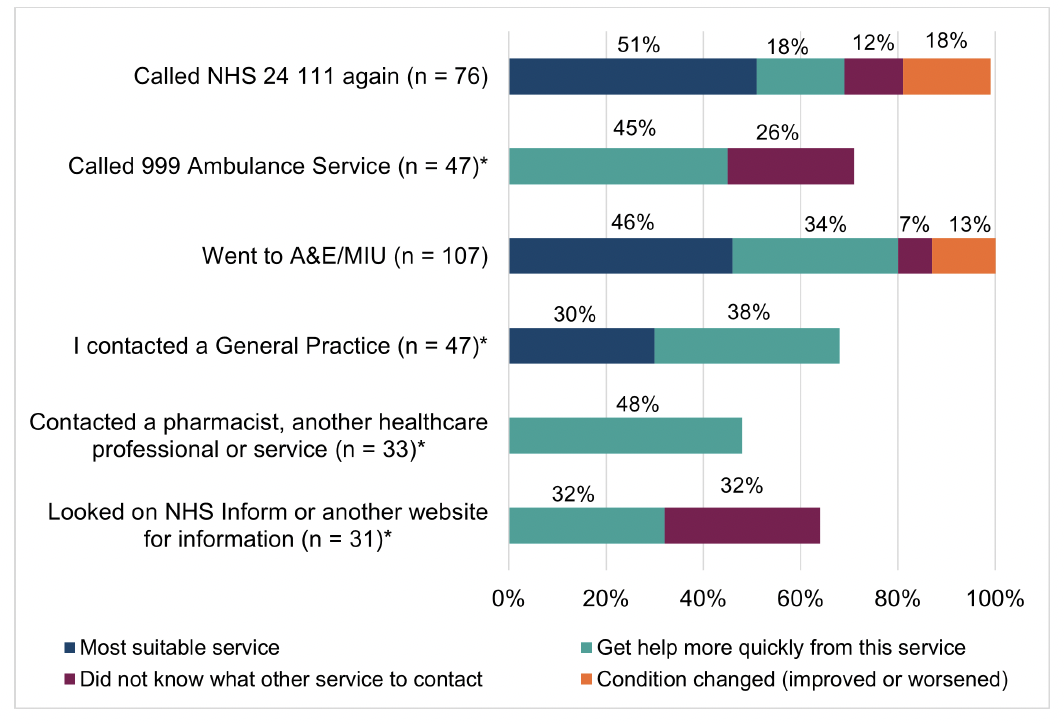
4.5 Reasons for taking actions after discontinuing the NHS 24 111 call
A crosstabulation of the action respondents took after ending the NHS 24 111 call and the reason for this action (Figure 4.6), shows that the most common reason given for calling NHS 24 111 again or going to A&E/MIU was because they thought it was most suitable for their health concern. Of those respondents that called 999 Ambulance Service after discontinuing their NHS 24 111 call, 45% (n=21) thought they would get help more quickly from this service and 26% (n=12) said they contacted this service as their condition changed. This is supported by the finding that of those who called 999 after discontinuing their call, 67% (n=30) said their health concern worsened in the time they waited after ending their NHS 24 111 call before contacting SAS (Technical Report, Section 6.1, Table 5).
4.5.1 Time waited before taking further action
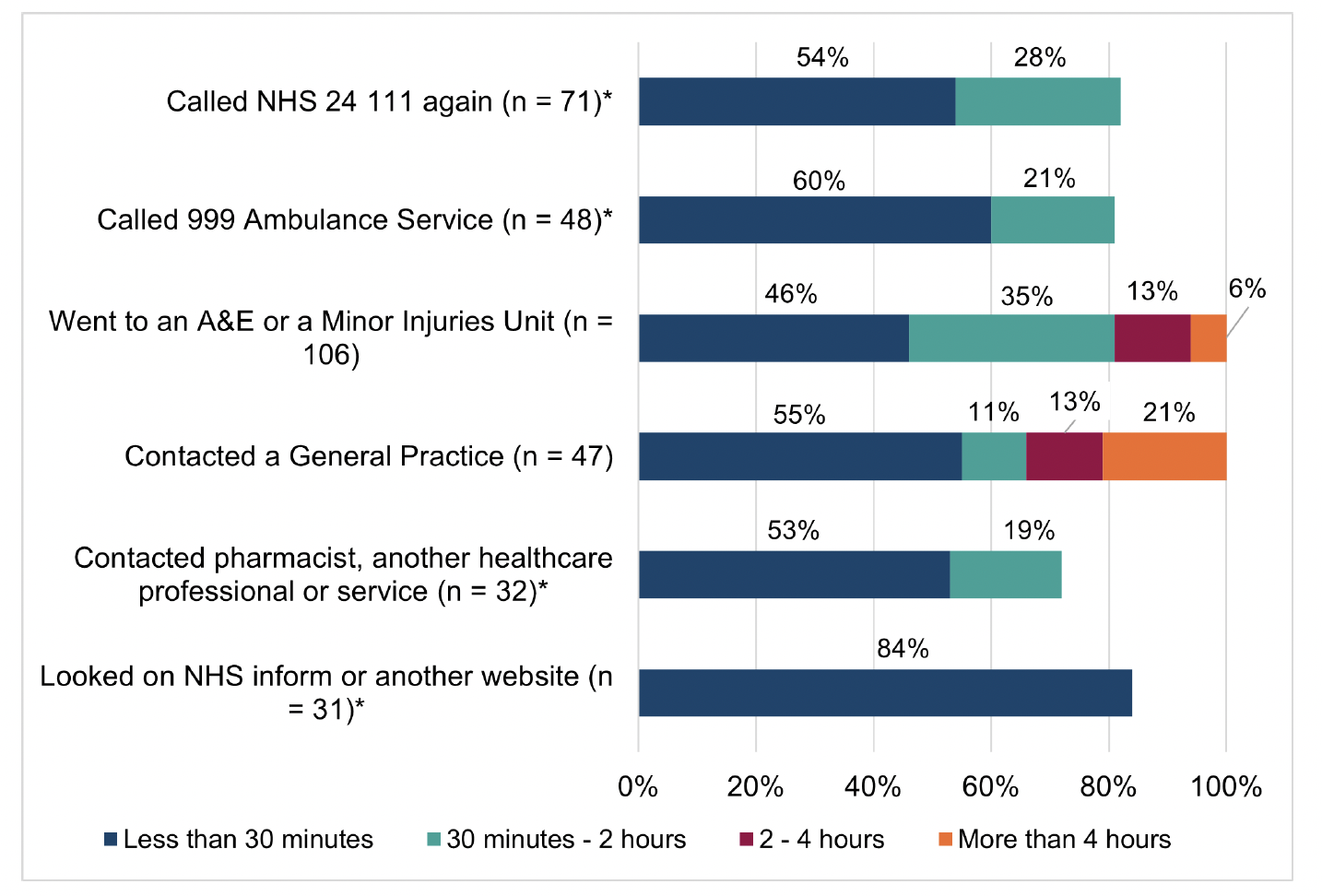
After discontinuing their call to NHS 24 111, just over half of the respondents (54%; n=185) said they waited less than 30 minutes before contacting a service or accessing information online. Only 4% (n=14) of respondents waited more than 8 hours before contacting/re-contacting a service for their health concern after ending the call to NHS 24 111 (Technical Report, Section 5, Table 15).
Figure 4.7 shows the action respondents took after discontinuing their call by the length of time they waited before taking this action. With the exception of those who went to A&E or a Minor Injuries Unit after ending the NHS 24 111 call, for all other services contacted/re-contacted (or information accessed online) at least half of the respondents did this in less than 30 minutes.
The survey asked people if their health concern changed in the time between ending the NHS 24 111 call and contacting/re-contacting a service. Almost half of respondents, 43% (n=148), said their health concern did not change in this time, although one third (33%; n=113) said their health concern worsened in the time that they waited before contacting another health service.
4.5.2 Experience of re-contacting NHS 24 111
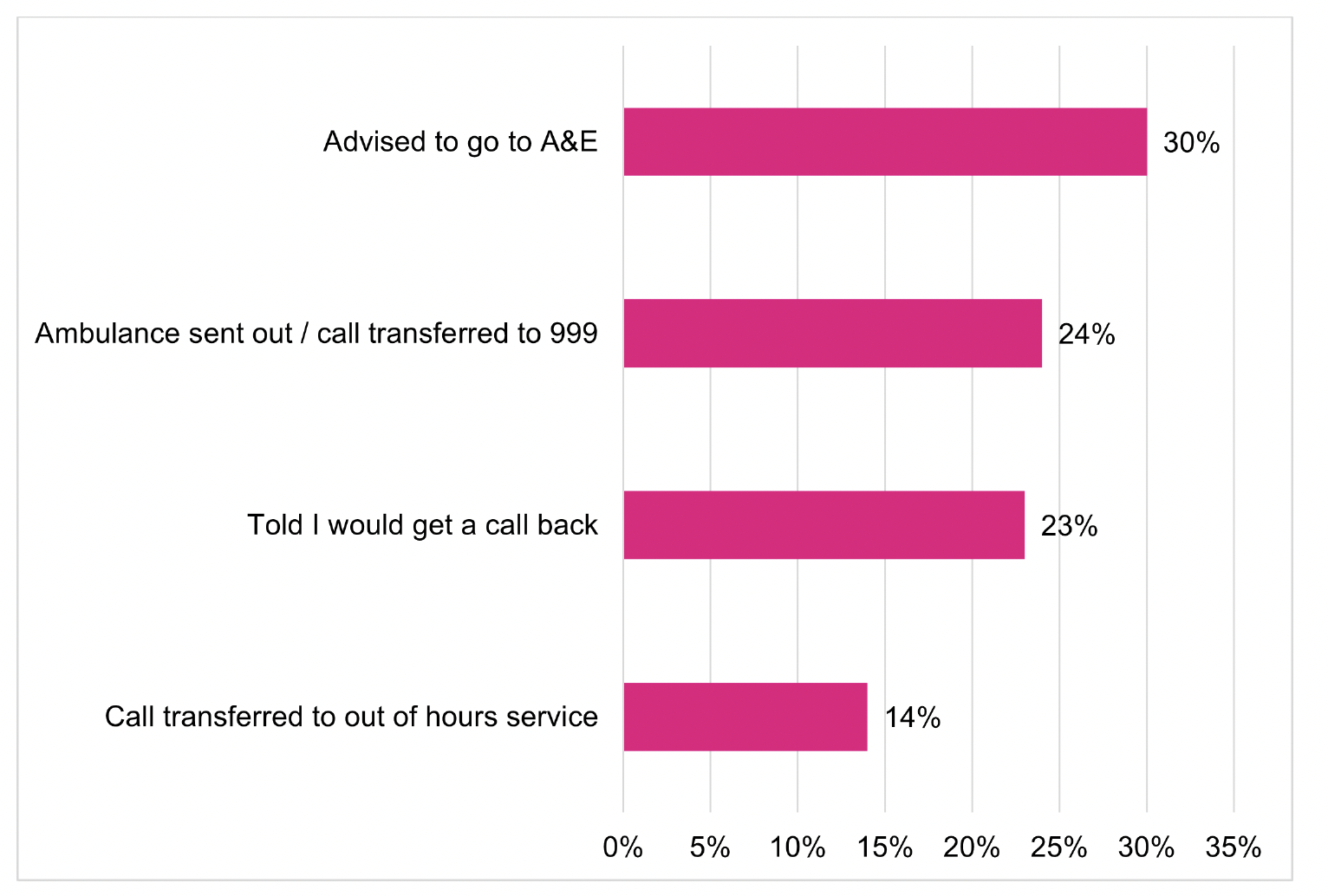
After discontinuing the initial call to NHS 24 111 before speaking to someone, 76 respondents (20%) called NHS 24 111 again later. For those that re-contacted NHS 24 111, nearly all (93%; n=71) said their call was answered that time.
Figure 4.8 shows the action taken or advice respondents received when they called NHS 24 111 back and spoke to someone. The most common action taken or advice respondents received when they re-contacted NHS 24 111 and spoke to someone was to go to an A&E Department (30%; n=21), an ambulance was sent/call was transferred to 999 (24%; n=17), they were told they would get a call back (23%; n=16), or their call was transferred to an out-of-hours service (14%; n=10). Therefore, just over three quarters of respondents (77%; n=54) reported receiving a secondary care endpoint advice or action (i.e. advised to go to A&E, ambulance sent/call transferred to SAS or told they would get a call back from FNC).
4.6 Respondents that took no further action
After ending the initial call to NHS 24 111 before speaking to someone, 11% (n=43) of respondents reported that they did not contact any other service.
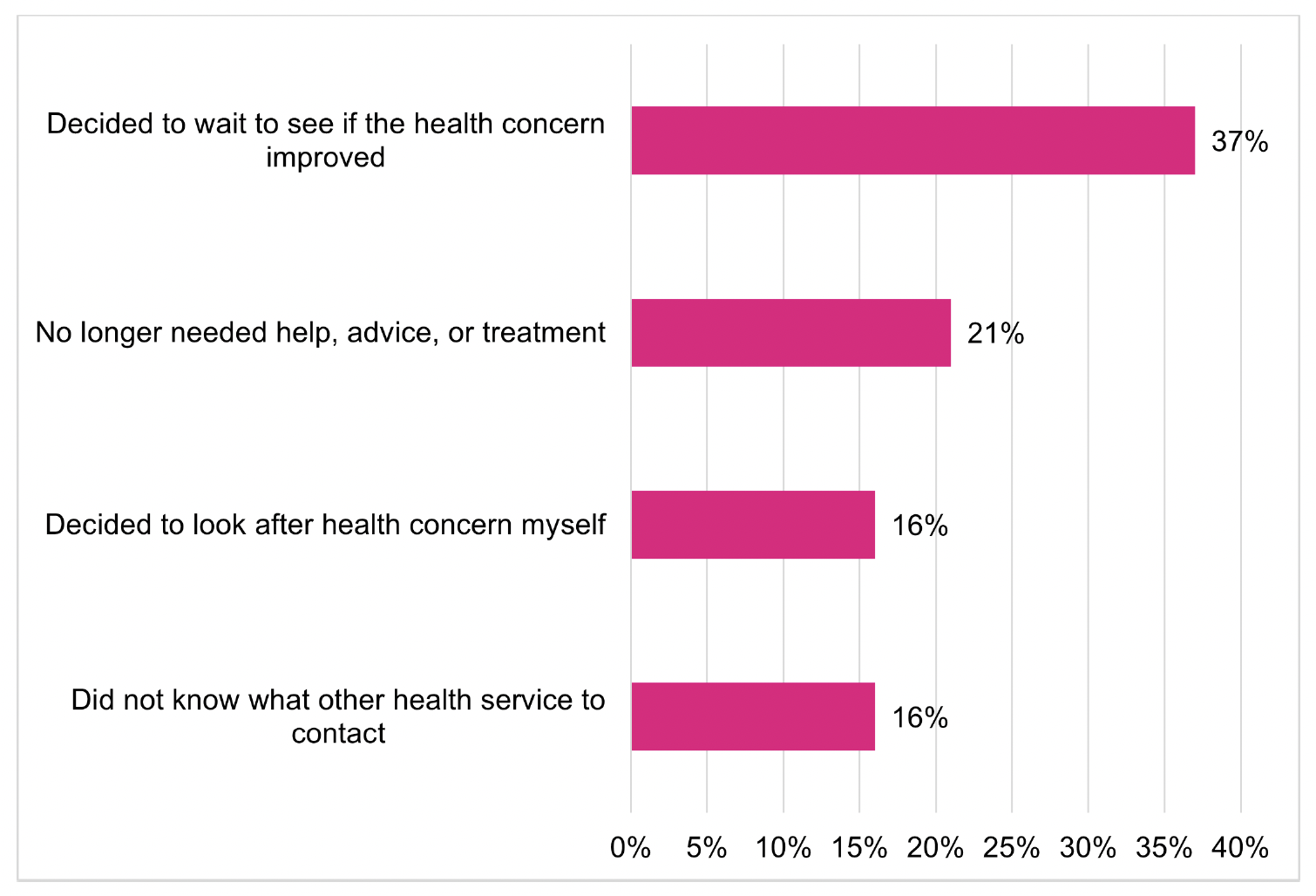
The reasons given by most respondents (37%; n=16) for not taking any further action was because they decided to wait to see if their health concern improved, whilst almost a quarter (21%; n=9) reported that they no longer needed help (Figure 4.9). Only a relatively small proportion of respondents reported that they did not take any further action because they did not know what other services were available (16%; n=7) or they decided to look after their health concern themselves (16%; n = 7). This suggests that most people who did not take any further action after discontinuing their NHS 24 111 call were able to manage their health concern themselves.
4.7 Overall experience
Differences were found in respondents’ ratings of their overall experience of contacting urgent care services by the action taken after discontinuing their call (Figure 4.10).
Of those who re-contacted NHS 24 111, 43% (n=33) rated their overall experience of urgent care services (from start to finish) as 8 or more out of 10. This was shown to be significantly higher than the proportions of respondents (who also rated their overall experience as 8 or more out of 10) that took one of the following actions after ending their call: those that went to A&E/MIU (24%; n=26); those that looked on NHS Inform or another website (23%, n=7); and those who did not contact any other service (16%; n=7). See Technical Report, Section 6.1, Table 7, for details.
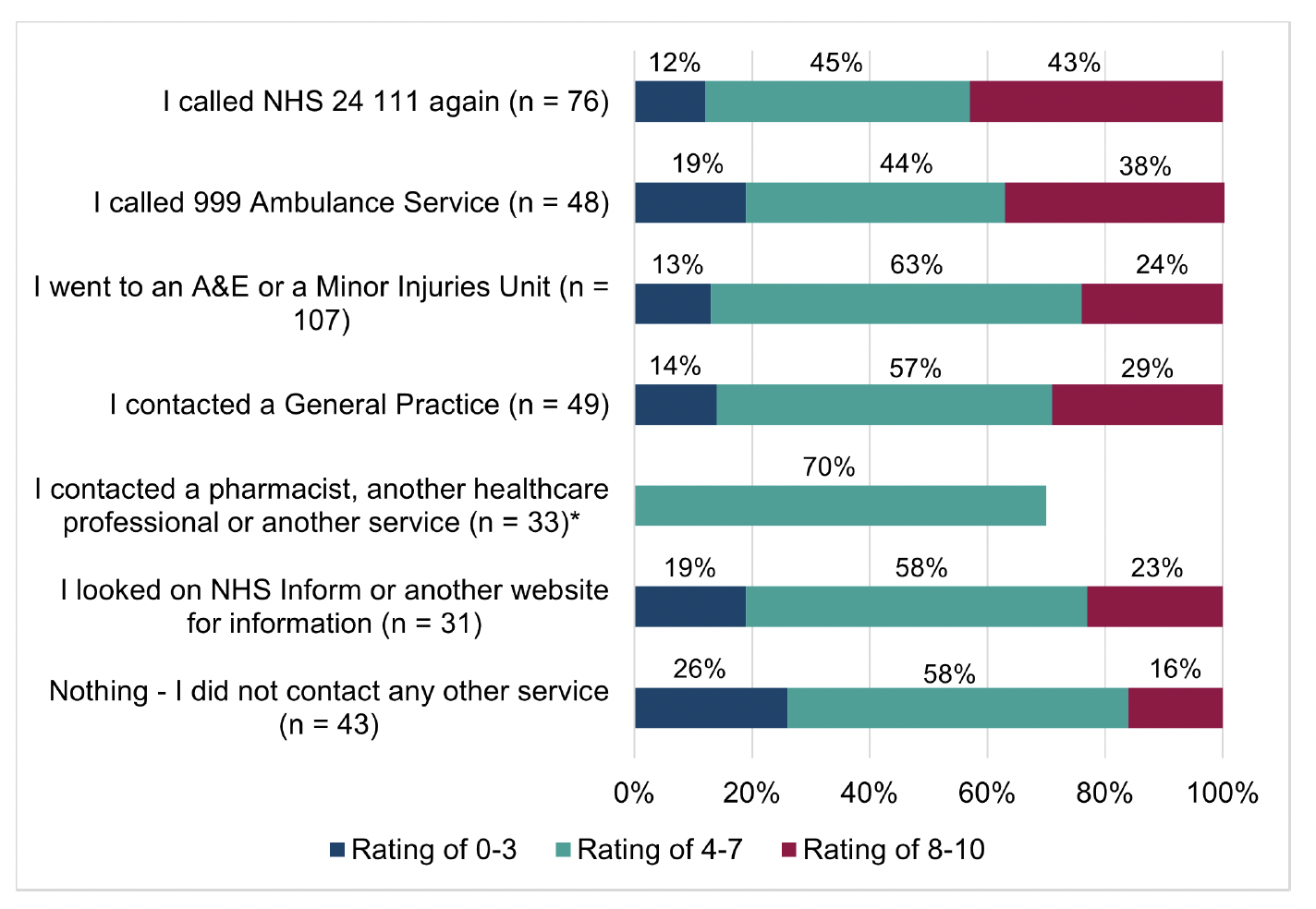
This finding suggests that those who re-contacted NHS 24 111 and accessed the RUC pathway via this entry point, reported more positively about their overall experience of contacting urgent care services than those who discontinued their call and accessed some services directly. However, it’s important to take into consideration the subsequent actions or advice given by NHS 24 111 to respondents, as this is likely to impact on overall experiences. As shown previously (Figure 4.8), of those respondents who re-contacted NHS 24 111, most (77%, n=54) reported that NHS 24 111 advised or actioned a secondary care endpoint.
The survey found some differences in respondents overall experiences of urgent care services by the length of time waited before ending the call, the day/time in which they contacted NHS 24 111 and whether they were calling for themselves or to get help for a child or another adult:
- Time waited before ending call
Of those respondents who waited less than 10 minutes before discontinuing their call, 40% (n=53) rated their overall experiences of urgent care services overall as 8 or more out of 10 (Technical Report, Section 6.1, Table 8). This is a significantly higher proportion when compared to those that waited 10-30 minutes (22%; n=31) or 30 minutes or longer before ending their call (18%; n=19). There was no clear pattern to respondents reports of whether they would call NHS 24 111 in the future if they had the same health concern (at the same time of day/night) by the length of time waited.
- Day/time contacted NHS 24 111
The survey showed that respondents who contacted NHS 24 111 in-hours were less likely to report that they would call NHS 24 111 again in the future when compared with those that called out-of-hours. Of those who contacted NHS 24 111 in-hours, a significantly smaller proportion (32%; n=29) reported that they would ‘definitely’ contact NHS 24 111 if they had the same problem (at the same time of day or night), compared to 43% (n=109) of those who contacted NHS 24 111 out-of-hours (Technical Report, Section 6.1, Table 9). There was no clear pattern to the respondents overall rating of urgent care services by day and time of call.
- Caller type
There were some differences in reported overall experiences by whether the respondent contacted NHS 24 111 for themself or for a child/another adult:
- A significantly smaller proportion of respondents who contacted NHS 24 111 to get help for another adult (34%; n=34) said they would ‘definitely’ contact NHS 24 111 again if they had the same health concern when compared to those that called for themselves (42%; n=71) or for a child (46%; n=39). See Technical Report, Section 8.1, Table 10 for more detail.
- Of those respondents that contacted NHS 24 111 for a child, a significantly smaller proportion (11%; n=10) rated their overall experience of urgent care services between 0 (‘I had a very poor experience’) and 3 out of 10 when compared to those that called for themselves (17%; n=31) or for another adult (21%; n=23). There were no significant differences by caller type in the proportion who rated their overall experience as 8 or more out of 10 (Technical Report, Section 6.1, Table 11).
Contact
Email: dlhscbwsiawsiaa@gov.scot
There is a problem
Thanks for your feedback