Maternity pathway and schedule of care: clinical guidance and schedule
This pathway illustrates the core care that women and their babies should receive. All core contacts antenatally and postnatally (other than 32 weeks antenatal visit for primigravid and parous as required) should be face to face as they include physical examination.
1. Introduction
All women and babies, whatever their circumstances, will have high quality and safe maternity and neonatal care, which takes account of their individual needs and preferences. Women, their partners and families will be aware of the support and choices that are available to them in order that care can be provided in partnership to achieve the best outcomes.
This pathway illustrates the core care that women and their babies should receive. All core contacts antenatally and postnatally (other than 32 weeks antenatal visit for primigravid and parous as required) should be face to face as they include physical examination.
The foundation of care is to offer a strengths based, family-centred, trauma informed, safe and compassionate approach to care that is individualised to each family entering into the maternity setting. This will support pregnant women, and their families, to optimise their birth and parenting potential.
Care provided will be tailored to each individual with continued ongoing assessment of needs throughout pregnancy, birth and the postnatal period to inform the range of birth choices available. This will be enabled by delivery of continuity of carer.
This Pathway includes schedules outlining the core contacts every woman should receive and is intended to cover the majority of care and clinical judgement required. When deciding it is not appropriate to follow the guidance this decision should be discussed with the woman and recorded.
This document will support conversations with women through their maternity journey. It is to be used in conjunction with and complement existing local information and/or guidance.
The information in this document complements the information in the Birth Place Decisions Leaflet, which is available for pregnant women to support informed decision making.
Health professionals should facilitate conversations and encourage questions.
There are different tools available to support quality conversations. The BRAN framework and It’s OK to Ask resource can enable women to be more involved and make informed decisions about their own care and treatment.
Care provided should be responsive and adaptable to individual needs circumstances and preferences.
The terms woman/women have been used throughout this document as this is the way that the majority of those who are pregnant and having a baby will identify. For the purpose of this document, this term includes girls. It also includes people whose gender identity does not correspond with their birth sex or who may have a non-binary identity.
All healthcare services should be respectful and responsive to individual needs, and all individuals should be asked how they wish to be addressed throughout their care.
An Equality Impact Assessment has been produced to accompany this publication.
Informed choice/consent:
Clinical practice requires clinicians to have discussions with women and give information regarding risks, benefits and alternatives throughout their maternity journey to enable women to make informed decisions that are right for their own situation.
Each consultation between women and healthcare professionals should be based on the assumption that they may suggest a set of clinical recommendations and care pathways that can be accepted or declined. Decisions about care should be documented, implemented and shared with the multi-disciplinary team as appropriate.
All discussions about decisions regarding maternity care should be clearly documented.
The principles of informed choice and consent must be applied when offering the care described in this Pathway.
Refer to Consent | RCOG
Refer to care_outside_guidance.pdf (rcm.org.uk)
1.1 Best Start Vision and Principles of Care
The Best Start: A Five Year Forward Plan for Maternity and Neonatal Care in Scotland (2017) outlined a vision for maternity care in Scotland where:
All mothers/birthing parents and babies are offered a truly family-centred, safe and compassionate approach to their care, recognising their own unique circumstances and preferences
Fathers, partners, co-parents and other family members are actively encouraged and supported to become an integral part of all aspects of maternal and newborn care
Birthing parents experience real continuity of care and carer, across the whole maternity journey, with families offered additional support tailored to their specific circumstances.
Services are redesigned using the best available evidence, to ensure optimal outcomes and sustainability, and maximise the opportunity to support normal birth processes and avoid unnecessary complications
Staff are empathetic, skilled and well supported to deliver high quality safe services, every time
Multi-professional team working is the norm with an open and honest team culture, with everyone’s contribution being equally valued
Principles of care:
- Care is supported by evidence
- The impact of inequality is recognised
- Consistently high quality communication is promoted
- Women are supported to take an active central role in their care and that of their baby/babies
- It is recognised that women’s situations are dynamic and circumstances may change over time
- All women have the same level of core care regardless of additional need.
- When offering care health professionals should be mindful of the UNICEF UK Baby Friendly Initiative standards.
The foundations of care are to offer every woman, every family, every time care which is:
- strengths based
- family-centred
- trauma informed
- safe
- compassionate
Care will be individualised. This will support women and their families to optimise their birth and parenting potential. Further information about how to support individualising care can be found in this guide on Personalised Care and Support.
Women are provided with advice and services to promote lifestyle changes during their pregnancy in order to improve their own health and the health of their baby.
1.2 Getting it right for every child (GIRFEC)
The primary midwife is responsible for carrying out the ‘Getting it right for every child’ (GIRFEC) wellbeing assessment and implementing and revisiting the resulting wellbeing plan. GIRFEC provides Scotland with a consistent framework and shared language for promoting, supporting, and safeguarding the wellbeing of all children and young people. GIRFEC is the key underpinning policy and approach to our collective work across the country to improving outcomes for babies, children and young people. GIRFEC supports families by making sure children and young people can receive the right help, at the right time, from the right people.
GIRFEC and the UNCRC (United Nations Convention on the Rights of the Child) (which Scottish Government has incorporated into Scots law) applies to everyone up to the age of 18. Before birth, midwives and maternity professionals can apply the values and principles of GIRFEC and support to the parents in considering their wellbeing, and that of the unborn baby. Following birth, the UNCRC captures children’s rights and articulates them within the context of a child’s life and experiences. These rights apply equally to all children either individually, or as a group, and apply in all settings including at home, in the community, at school, or in other protective settings such as in secure primary care facilities. The best interests of the child should be a primary consideration, and the views of the child must be given due weight in accordance with their age and maturity. GIRFEC also continues to apply to all children and young people up to the age of 18, or older if still at school, including young people who have left school but are not yet 18. As such, midwives and maternity professionals should consider that GIRFEC and the duties in the UNCRC (Incorporation) (Scotland) Act will also apply to young parents up to the age of 18.
GIRFEC takes account of the 8 SHANARRI indicators when considering the wellbeing and specific needs of women throughout pregnancy and birth. These indicators are shown in the diagram below.
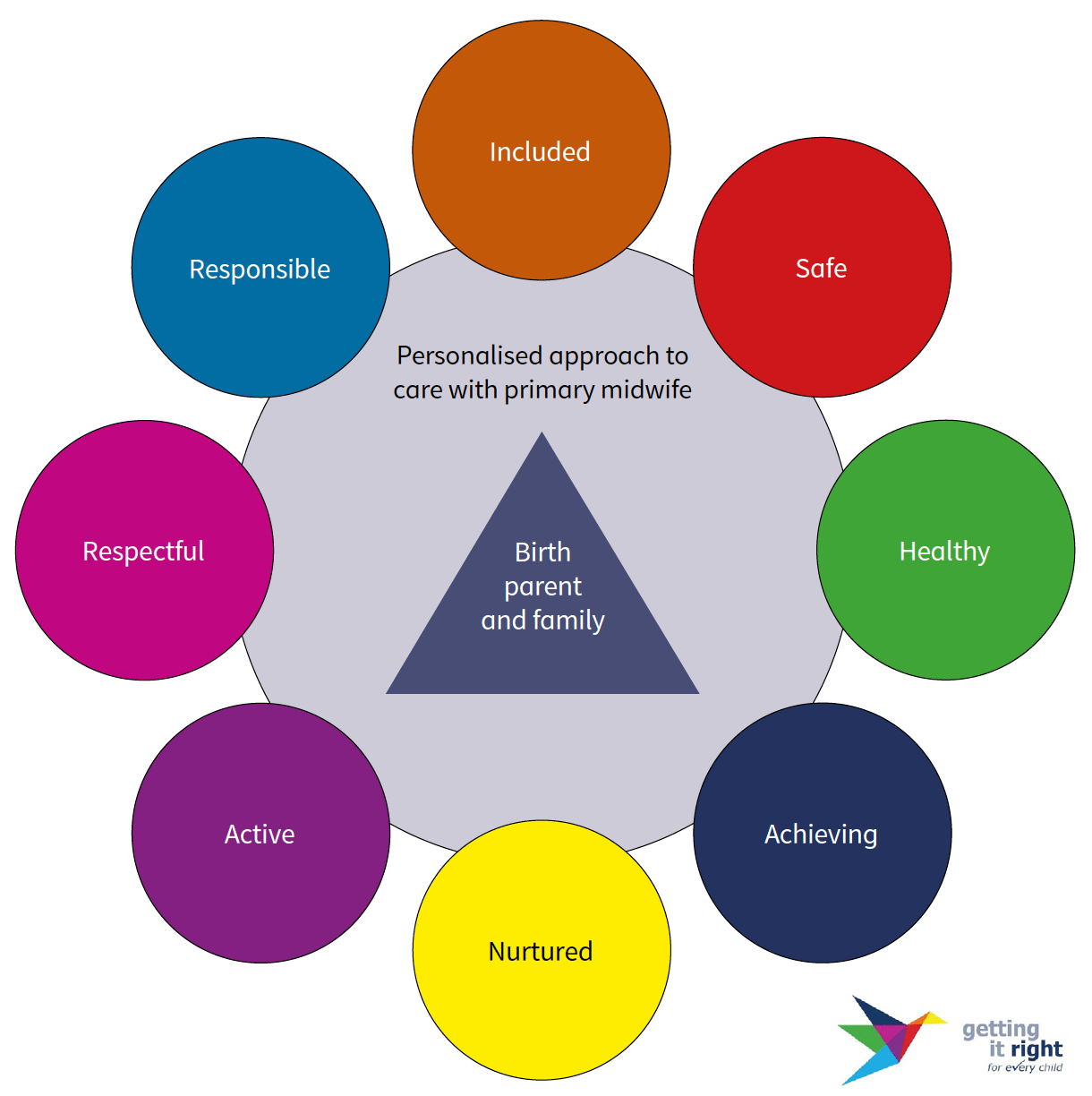
Graphic text below:
Outer circle:
Included • Responsible • Safe • Respectful • Healthy • Active • Achieving • Nurtured
Inner circle:
- Personalised approach to care with primary midwife
- Birth parent and family
1.3 Continuity of Carer
The Best Start recommends that every woman will have continuity of carer from a primary midwife working within a continuity of care model who will provide the majority of their antenatal, intrapartum and postnatal care. Relationships are key and it is vital that parents are receiving consistent care from one person. Where appropriate, women will also have continuity of obstetric care.
The woman and her primary midwife will develop a plan of care to ensure all aspects of the woman’s clinical, personal, cultural and lifestyle circumstances are considered and addressed. Any additional care offered, clinical and social, will be brought around the woman, with the woman at the centre, coordinated by and in partnership with their primary midwife. Keeping care close to home, where possible, will allow parents and their babies to stay together.
Midwives delivering continuity of care and carer, and the named obstetricians, build strong working relationships, focused around a specific caseload of women. This supports effective team working, enables on-going discussions between women, their primary midwife and their named obstetrician or wider team where required. By embedding a supportive decision making approach across Scotland involving healthcare professionals, women and families working together, the best care possible can be delivered.
Evidence shows that outcomes for both women and babies are improved when they receive continuity of midwifery care, and this should be provided to every woman. Women who need the input of an obstetrician will have continuity of a named obstetrician throughout their antenatal and postnatal care.
1.4 Personalised Care
The principle of personalised or individualised care is that it is always centred around the needs and choices of the woman (and her baby/ies) and not the needs of the service. Choice is supported with unbiased, evidence based and non judgemental information sharing and any plan is co produced with woman and care givers. Further information about how to support individualising care can be found in this guide on Personalised Care and Support.
1.5 Social Complexities
There are degrees to complexities, so it is vital that all midwives are equipped as the first point of contact, to recognise and work with women with social complexities appropriately. The work of the primary midwife is likely to be particularly important for women with social complexities, and caseloads may need to be reviewed to support this position.
Women with more complex needs may be offered referral into specialist, multi-professional and multi-agency teams, but many women can be supported as part of routine care, with extra support from their primary midwife and the wider team.
In all cases it is important to ensure that the team care is constructed around the women’s needs, and is accessible.
The National Autism Implementation Team have produced some Key Messages for Perinatal Teams, which can be used by teams to help them support neurodivergent women in their care.
Contact
There is a problem
Thanks for your feedback