Maternity pathway and schedule of care: clinical guidance and schedule
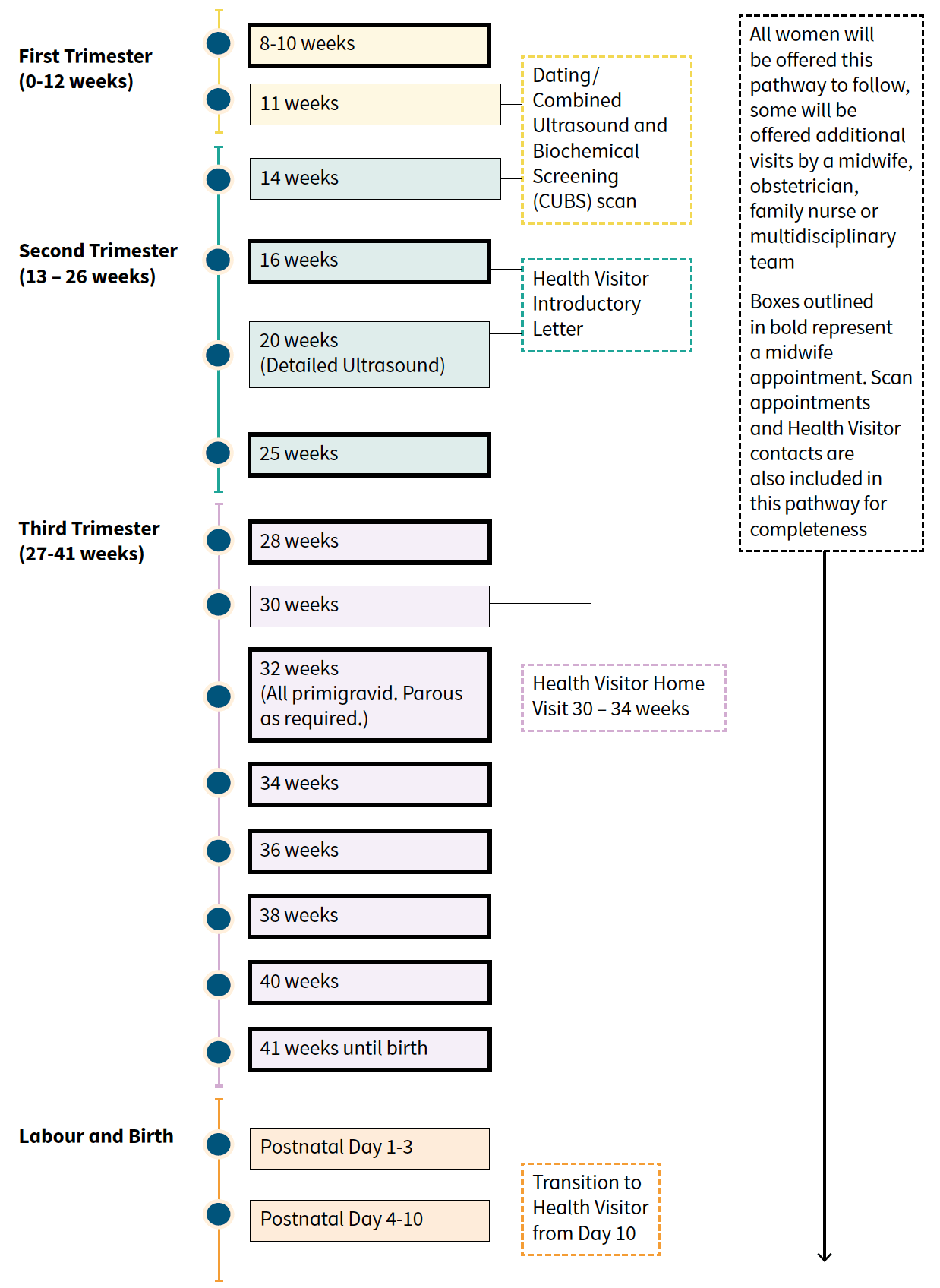
This pathway illustrates the core care that women and their babies should receive. All core contacts antenatally and postnatally (other than 32 weeks antenatal visit for primigravid and parous as required) should be face to face as they include physical examination.
2. Core Health Contacts for All Women and Babies (Conception to Postnatal)
Graphic text below:
First Trimester (0-12 weeks)
8-10 weeks
11 weeks
14 weeks
- Dating/ Combined Ultrasound and Biochemical Screening (CUBS) scan
16 weeks
- Health Visitor Introductory Letter
Second Trimester (13 – 26 weeks)
20 weeks (Detailed Ultrasound)
25 weeks
Third Trimester (27-41 weeks)
28 weeks
30 weeks
- Health Visitor Home Visit 30 – 34 weeks
32 weeks (All primigravid. Parous as required.)
34 weeks
36 weeks
38 weeks
40 weeks
41 weeks until birth
Labour and Birth
Postnatal Day 1-3
Postnatal Day 4-10
- Transition to Health Visitor from Day 10
All women will be offered this pathway to follow, some will be offered additional visits by a midwife, obstetrician, family nurse or multidisciplinary team
Boxes outlined in bold represent a midwife appointment. Scan appointments and Health Visitor contacts are also included in this pathway for completeness
Additional Antenatal and Postnatal Care
All women will receive the core care illustrated above. Some women with medical conditions, comorbidities, or complex social needs may need to be offered multidisciplinary team care. The primary midwife can offer additional appointments if the need is identified.
Primary Midwife
The primary midwife leads and co-ordinates care planning for women with additional needs and will continue to be the lead for midwifery care throughout.
Named Obstetrician
The named obstetrician leads care planning for women with additional clinical needs with input from a range of multidisciplinary partners as required.
| Pre-existing medical conditions where referral to an obstetrician for care planning is required. This list is not exhaustive. Any other conditions of concern should be considered for discussion with or referral to an obstetrician. | |||
|---|---|---|---|
| Confirmed cardiac disease | Pre-existing type 1 or 2 diabetes | Cystic fibrosis | Asthma with an increase in treatment or hospital admission in current pregnancy |
| Hypertensive disorders | Non-specific connective tissue disorders and systemic lupus erythematosus, scleroderma | Organ transplant | Epilepsy or other significant neurological conditions such as multiple sclerosis or myasthenia gravis |
| Hyperthyroid | BMI >40 | Haemoglobinopathies, such as sickle cell disease | Rhesus isoimmunisation |
| Atypical antibodies | Female Genital Mutilation | Past or current Malignancy | Hep B/C or liver disease with abnormal liver function |
| HIV | Bleeding or platelet disorder such as ITP | Von Wilibrands Disorder | History of thrombolic disorders |
| Inflammatory Bowel Disease (Crohn’s disease or Ulcerative colitis) | Current active Varicella Zoster, rubella, herpes | Abnormal renal function or renal disease requiring supervision by a renal specialist | |
| Family History of Genetic Conditions | Maternal age 40 or over at booking | Significant substance or alcohol use | |
| Previous cerebrovascular accident | Psychiatric disorder under current psychiatric care | Previous myomectomy or hysterotomy | |
| Unstable hypothyroid such that a change in treatment is needed | Spinal abnormalities | Previous significant cervical treatment | |
| Tuberculosis under current treatment | Previous history of bariatric surgery | ||
If you are unsure, please ask.
Some conditions, such as perinatal mental health or anaemia, will have an established local pathway that should be followed.
Previous pregnancy, labour and birth complications where referral to an obstetrician for care planning is required. This list is not exhaustive. Any other conditions of concern should be considered for discussion with or referral to an obstetrician. |
|||
|---|---|---|---|
| Previous shoulder dystocia | Eclampsia | Placental abruption | Uterine rupture |
| Primary postpartum haemorrhage | Previous caesarean birth | Stillbirth or neonatal death | Late miscarriage or recurrent miscarriage |
| Previous baby with neonatal encephalopathy | Pre-eclampsia requiring preterm birth | Extensive vaginal, cervical, or third- or fourth-degree perineal trauma | |
| Uterine anomaly such as bicornuate uterus | Previous growth restriction | Preterm birth or Premature Rupture of Membranes < 34 weeks | |
If you are unsure, please ask.
Some conditions, such as perinatal mental health or anaemia, will have an established local pathway that should be followed.
Choice of Place of Birth
Birth is generally very safe for women and their babies with low risk of complications.
Each NHS Board will provide the full range of choice of place of birth within their region.
A national Birthplace Decision Leaflet has been designed to support women with their decision on where to give birth and have informed discussions with their midwife and consultant obstetrician (where appropriate).
Additional care – labour and birth
Some women may have complex care needs which mean they will be advised that the optimal place in which to labour and birth should be in an obstetric unit.
In an obstetric unit care should continue to be individualised and options for labour and birth continue to be considered, acknowledging that not all women will be recommended the same package of care. For example, it may not be necessary to offer a women who has had a previous Post Partum haemorrhage (PPH) continuous electronic fetal monitoring (CEFM) in labour.
Obstetric conditions arising in this pregnancy where referral to an obstetrician for care planning is required. Most women with these conditions will be advised to birth in an obstetric unit. This list is not exhaustive. Any other conditions of concern should be considered for discussion with or referral to an obstetrician. |
|||
|---|---|---|---|
| Preeclampsia or pregnancy induced hypertension | Multiple pregnancy | Placenta praevia | Polyhydramnios |
| Fibroids >5cm | Fetal growth restriction | Oligohydramnios in the absence of ruptured membranes | Haemoglobin less than 85g/dl |
| Malpresentation – breech or transverse lie | Recurrent antepartum haemorrhage | Gestational Diabetes | Obstetric cholestasis |
| Fetal abnormality/anomaly | Ultrasound suspicion of macrosomia | Abnormal fetal heart rate, umbilical or fetal doppler studies | Preterm prelabour rupture of membranes |
If you are unsure, please ask.
Some conditions, such as perinatal mental health or anaemia, will have an established local pathway that should be followed.
Vaccines
| Vaccines discussed and offered (as per guidance) in antenatal period | |
|---|---|
| Flu vaccine | In season at any gestation |
| Whooping cough | From 16 weeks |
| Respiratory syncytial virus (RSV) | From 28 weeks |
Contact
There is a problem
Thanks for your feedback