Minimum Unit Pricing (MUP) Continuation and future pricing: Business and Regulatory Impact Assessment
Scottish Government developed a Business and Regulatory Impact Assessment to analyse the costs and benefits of the continuation and uprating of Minimum Unit Price (MUP) on businesses.
2. PURPOSE AND INTENDED EFFECT
2.1 Background
Despite progress, alcohol-related harm continues to be one of the key public health challenges in Scotland. In 2021 (the latest year for which data are available), across the population aged over 16, population purchase of alcohol averages 18.1 units per week per person[8]. This is nearly 30% more than the lower-risk UK Chief Medical Officers’ guidelines of 14 units per week. The high population-level alcohol consumption in Scotland causes a range of health and wider harms.
Overall population health has worsened in Scotland across key measures in the last ten years. Action across both primary prevention (tackling the causes of poorer health outcomes) and secondary prevention (mitigating or reducing the effects of partly established health harms) is key to supporting an improvement in population-wide health. Minimum unit pricing is part of the preventative approach to improving population health through behaviour change.
MUP was first implemented in 2018 and, according to analysis of its operation, has had a broadly positive impact on levels of alcohol-related harm. Public Health Scotland’s overall conclusion was:
‘Overall, the evidence supports that MUP has had a positive impact on health outcomes, including alcohol-related health inequalities. There was no clear evidence of substantial negative impacts on the alcoholic drinks industry or social harms at the population level’.
The evaluation from PHS found MUP was estimated to have reduced deaths wholly attributable to alcohol consumption by 13.4% and was likely to have reduced hospital admissions by 4.1% up to the end of 2020 compared to what would have happened if MUP was not in place[9]. MUP was estimated to reduce alcohol sales by 3% with the greatest reductions in sales for products that increased the most in price over the timeframe of the evaluation. They also found no consistent evidence of impact, positive or negative, on wider social harm due to alcohol, however, there is some qualitative evidence of negative consequences, particularly for those with alcohol dependence on low incomes.
There is no consistent evidence that MUP impacted either positively or negatively on the alcoholic drinks industry in Scotland as a whole. However, the Scottish Ministers note that some distributional impacts on some product types and businesses were found, for instance some instances of retailers delisting larger sizes of brands that had experienced the largest increase in price per unit, though no evidence of any product disappearing in all its package variants entirely.[10]
The legislation which underpins minimum unit pricing is the Alcohol (Minimum Pricing) (Scotland) Act 2012. The Act includes a ‘sunset clause’, which means that the legislation will expire after 6 years of being in force unless Scottish Ministers make an Order to continue its effect. Without such an Order, which would require the approval of the Scottish Parliament, the MUP provisions will expire on 30 April 2024. The Act also places a duty on Scottish Ministers to lay a report on the operation and effect of the minimum pricing provision as soon as practicable after 5 years of MUP being in force.
This final BRIA contains an assessment of two policy proposals: 1) continuing the effect of the MUP legislation and 2) in the event of continuation, an increase in the price per unit, to 65ppu.
The pence per unit (ppu), set when MUP was implemented in 2018, has remained at 50ppu, against a backdrop of general prices rising through inflation. The impact of MUP at 50ppu in 2018 will therefore, all other things being equal, have reduced over time with the impact of inflation. Continuing with MUP at 50ppu in 2024 would be unlikely to generate the intended benefits, as found in the evaluation to date, to the same extent. If the price were to remain at 50ppu, over time the benefits which have been evidenced to date would be reduced.
The Scottish Government commissioned the Sheffield Alcohol Research Group (SARG) to undertake new modelling work to inform a review of the current 50ppu threshold. The modelling uses 2019 as the baseline year (control arm) as this was the most recent year for which all data were available when data was input to the model. It takes account of the initial impacts of MUP at 50ppu and is prior to any impact COVID-19 has had on consumption and harms. The control arm of the model is that 50ppu remains in place, with the 50ppu threshold being uprated each year in line with inflation using the CPIH[11]. When modelling changes the MUP threshold it is assumed these changes are introduced at the start of 2019 and that any new threshold is also uprated in line with CPIH to keep ‘prices in constant real terms’.
The modelling estimates that increasing MUP would lead to a reduction in alcohol-related harms such as hospital admissions, mortality, and years of life lost. Conversely, the model estimates that if MUP was lowered, consumption would increase leading to higher levels of alcohol-related harms.
For this reason, the second policy proposal assessed in this Final BRIA is in relation to the increased minimum unit price of 65ppu.
Legislative Background
In 2012, the Scottish Parliament passed the Alcohol (Minimum Pricing) (Scotland) Act 2012 (the 2012 Act) which made provision for a system of minimum unit pricing for alcohol. It amended the Licensing (Scotland) Act 2005, and introduced a new mandatory licence condition, which requires that alcohol must not be sold at a price below its minimum price.
Implementation was delayed following challenge in the courts until the UK Supreme Court ruled the legislation was lawful in November 2017. Following consultation on the Scottish Government preferred price, the Alcohol (Minimum Price per Unit) (Scotland) Order 2018 was laid in March 2018 and approved in Parliament in April 2018. That legislation set the minimum price per unit for alcohol at 50 pence.
The 2012 Act also contains a ‘sunset clause’ that sets out that the minimum pricing provisions expire at the end of the six-year period, unless Scottish Ministers make provision (through the making of an Order agreed by the Scottish Parliament) to continue with the policy. This clause was inserted to enable robust evaluation of the overall impact of the policy following implementation to be conducted, and to assess the extent to which the policy has met its intended aim of reducing alcohol-related harm.
The 2012 Act also placed a duty on Scottish Ministers to lay a report on the operation and effect of the minimum pricing provisions. The report has now been laid and contains detail on the extent to which the policy has, to date, met its intended aim of reducing alcohol harm. This information was drawn from the evaluation of the policy led by Public Health Scotland and from the findings of a call for evidence which included Ministerial roundtable events, and engagement with relevant stakeholders and expert groups including public health and business sectors.
The overall conclusion in the PHS final evaluation report on MUP is that the evidence supports that MUP has had a positive impact on health outcomes - MUP was estimated to have reduced deaths directly caused by alcohol consumption by 13.4% and likely to have reduced hospital admissions by 4.1% up to the end of 2020 compared to what would have happened if MUP had not been in place.
The evaluation also concluded that MUP has contributed to reducing health inequalities, as the largest estimated reductions in deaths and hospital admissions wholly attributable to alcohol consumption were seen in those living in the 40% most deprived areas.
There was also strong and consistent evidence of a reduction in alcohol consumption following MUP implementation. The evaluation found that the reduction in consumption was driven by the heaviest purchasing households, and the majority of households were not affected, leading to the conclusion that MUP was well targeted. As MUP resulted in a decrease in alcohol-attributable deaths and hospital admissions related to chronic conditions, the evaluation has taken this as further evidence that MUP has reduced consumption in those that drink at hazardous and harmful levels.
The evaluation noted that there was limited evidence to suggest that MUP was effective in reducing consumption for people with alcohol dependence (at a population level, this is estimated to represent around 1% of adults, based on Scottish Health Survey ‘AUDIT’ scores of 16+ which indicate drinking at harmful and possibly dependent levels[12]). People with alcohol dependence are a particular subgroup of those who drink at harmful levels and have specific needs. People with alcohol dependence need timely and evidence-based treatment and wider support that addresses the root cause of their dependence.
Overall, there was no consistent evidence that MUP impacted either positively or negatively on the alcoholic drinks industry as a whole.
The evaluation concluded that compliance with the legislation was high and that sales of alcohol below £0.50 per unit largely disappeared following the implementation of MUP. There was also strong evidence of an immediate increase in the average price per unit of alcohol sold through the off-trade in Scotland, relative to other areas in Great Britain, following the implementation of MUP.
Roundtable events provided an opportunity for relevant stakeholders and expert groups including across health and business sectors to consider their own experiences of MUP which generated additional insight and perspective for Ministers to reflect upon.
The Scottish Government has published the Alcohol (Minimum Pricing) (Scotland) Act 2012: Report on the operation and effect of the minimum pricing provisions 2018 – 2023, and laid it before the Scottish Parliament.
2.2 Objective
The policy prospectus, setting out how the government will deliver for Scotland over the next three years, was published on 18 April 2023. It sets out three missions that will be central to the Scottish Government: equality, opportunity and community. With regard to alcohol specifically, there is a commitment that by 2026, Scottish Ministers will have:
Taken decisive preventative action to reduce alcohol harm, including reviewing minimum unit pricing…
The MUP policy aims to reduce health harms caused by alcohol consumption by setting a floor price below which alcohol cannot be sold. In particular, it targets a reduction in consumption of alcohol that is considered cheap, relative to its strength. It aims to reduce both the consumption of alcohol at population level and, in particular, among those who drink at hazardous and harmful levels. In doing so, it aims to reduce alcohol-related health harms among hazardous and harmful drinkers, and contribute to reducing harm at a whole population level.
People who drink at hazardous and harmful levels in lower socio-economic groups suffer greater harms than those who drink at these levels in higher socio-economic groups due to the impact of multiple drivers of health inequality[13]. MUP is also intended to address alcohol-related health inequalities by reducing consumption and therefore harm among hazardous and harmful drinkers as a whole, having a positive effect on health inequalities given the greater harms people in lower socio-economic groups experience in relation to alcohol.
The overall purpose of this Final BRIA is to set out the reasons for Scottish Ministers' decisions to continue with the policy and to increase the price to 65ppu. It also covers the likely costs, benefits, risks and impact on different sectors of a minimum unit price for alcohol at the increased price of 65ppu.
2.3 Rationale for Government intervention
Alcohol as a public health challenge
The Scottish Government recognises alcohol as a major public health challenge, with harmful drinking carrying a risk of physical and mental health problems, as well as social and economic losses to individuals and society[14]. Excessive alcohol consumption at a chronic level is associated with increased risk of high blood pressure, chronic liver disease and cirrhosis, pancreatitis, some cancers, mental ill-health, and accidents[15]. Links have also been established between harmful drinking and the incidence of infectious diseases such as tuberculosis and HIV/AIDS[16], and the risk of alcohol-related harm increases with greater levels of average alcohol consumption in a population[17]. Harms related to drinking are not solely limited to the drinker – they can include someone committing, or being a victim of, a crime[18]; alcohol can also play a complicated role in domestic abuse and violence. Alcohol’s harm to others is a key driver of international alcohol policy[19].
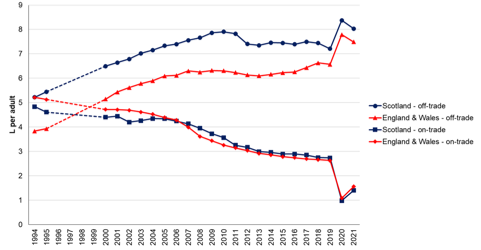
In 2021, people in Scotland bought enough alcohol for everyone aged over 16 to drink 18.1 units of alcohol every week (9.4 litres)[20]. This is nearly 30% more than the lower-risk UK Chief Medical Officers’ guidelines of 14 units per week. Although at the lowest level since 1994, total alcohol sales in Scotland are 4% more than in England & Wales[21]. Figure 1 shows the volume trend since 1994 for on-trade and off-trade sales.
It is well established that harms attributable to alcohol are related to both the quantity of alcohol consumed and the pattern of drinking[23]. A study found “Alcohol use is a leading risk factor for global disease burden and causes substantial health loss. We found that the risk of all-cause mortality, and of cancers specifically, rises with increasing levels of consumption, and the level of consumption that minimises health loss is zero”[24].
The most recent Scottish Health Survey 2022 (SHeS), published December 2023, shows that the prevalence of hazardous or harmful drinking has generally decreased over time, with levels dropping from 34% in 2003 to 22% in 2022.
Social desirability bias (under-reporting of less socially acceptable behaviours in self-report studies like surveys) is known to be an issue in relation to survey estimates of alcohol consumption[25], and so while evidence of population level reductions of harmful and hazardous drinking is welcome, it is important to interpret this evidence in the context of other well established international measures of population level consumption including sales data as above.
In 2022 1,276 people died from causes wholly attributable to alcohol[26] - an increase of 2% on the previous year. This is equivalent to an average of 3 people dying every day.
A PHS report published in March 2023, The impact of the COVID-19 pandemic on alcohol consumption and harm in Scotland and England: An evidence summary[27] found that alcohol-specific death rates increased for both Scotland and England from 2019 to 2020 (Scotland 15.6% increase; England 19.3% increase) and then again between 2020 and 2021 (Scotland 4.2% increase; England 6.9% increase), with percentage increases greater for England than Scotland. The impact of the pandemic on alcohol consumption and harms is covered in more detail later in this section.
In addition to deaths wholly caused by alcohol, some deaths are partly attributable to alcohol consumption. Analysis[28] found there were an estimated additional 3,705 deaths attributable to alcohol consumption in 2015. Of these, 1,048 (28%) were due to cancers, 544 deaths were from heart conditions and strokes, and 357 deaths were from unintentional injuries e.g. falls.
In the 2021/22 financial year, there were 35,187 alcohol-related hospital admissions (stays) in general acute hospitals in Scotland[29]. That’s around 670 hospital admissions every week at a time when the health service is meeting the challenges posed post-pandemic as it continues its recovery phase.
The most recent publication on avoidable mortality[30], shows the rate of avoidable mortality rose by 4% in 2021, with alcohol and drug related disorders the third leading cause of avoidable deaths: 2,641 avoidable deaths (of which 1,245 were from alcohol) with a rate of 53 per 100,000 people. Deaths from alcohol and drug disorders are preventable, meaning that they can be mainly avoided through effective public health and primary prevention interventions. People living in the most deprived areas in Scotland are 4.1 times as likely to die an avoidable death compared to those in the least deprived areas. The increase in avoidable mortality rates in 2021 has disproportionately occurred in the most deprived areas.
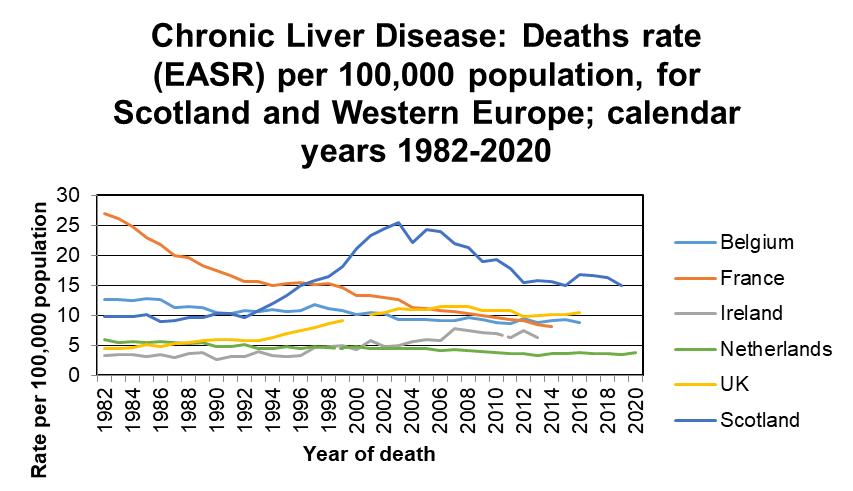
Whilst recognised as a problem across the UK, the evidence shows that alcohol-related harm through alcohol misuse is greater in Scotland, with rates of alcohol-specific deaths highest in Scotland.[31] Mortality rates for chronic liver disease (Figure 2), of which alcohol consumption is one of the most common causes, are also markedly higher in Scotland compared to the UK as a whole and other Western European countries.[32]
Evidence-based strategies to reduce alcohol harms
The World Health Organization’s (WHO) overview[34] of alcohol states:
“Alcohol is a toxic and psychoactive substance with dependence producing properties. In many of today’s societies, alcoholic beverages are a routine part of the social landscape for many in the population. This is particularly true for those in social environments with high visibility and societal influence, nationally and internationally, where alcohol frequently accompanies socializing. In this context, it is easy to overlook or discount the health and social damage caused or contributed to by drinking.
Alcohol consumption contributes to 3 million deaths each year globally as well as to the disabilities and poor health of millions of people. Overall, harmful use of alcohol is responsible for 5.1% of the global burden of disease. Harmful use of alcohol is accountable for 7.1% and 2.2% of the global burden of disease for males and females respectively. Alcohol is the leading risk factor for premature mortality and disability among those aged 15 to 49 years, accounting for 10 percent of all deaths in this age group. Disadvantaged and especially vulnerable populations have higher rates of alcohol-related death and hospitalization”.
WHO’s publication, Global strategy to reduce the harmful use of alcohol[35], sets out a variety of policy options that countries could consider in order to reduce alcohol consumption and alcohol harms. A Global Alcohol Action Plan 2022-2030[36] to implement the global strategy has been developed and was adopted by the 75th World Health Assembly in May 2022. The Plan aims to bring together the available evidence in alcohol control to tackle alcohol-related harms.
The latest edition of the WHO report, Alcohol: No Ordinary Commodity[37], building on previous editions, reviews the numerous policy options available in terms of their ability to reduce alcohol consumption and alcohol-related problems. The ‘best practices’ are strategies and interventions that are proposed by WHO as being highly effective, supported by evidence, impacting on the target group and relatively low cost. Policy measures in this category are restrictions on affordability, availability, and accessibility; marketing controls and drink-driving deterrents. The one with the strongest research support is alcohol pricing and tax policy.
WHO points to three ‘best buys’ as the most effective measures to prevent and tackle alcohol-related harms – reducing the Affordability, Availability and Attractiveness of alcohol[38]. In collaboration with international partners and following the United Nations high-level meeting on prevention and control of noncommunicable diseases (NCDs), WHO launched the SAFER initiative[39] in 2019 to deliver health and development gains in order to meet global, regional and country health and development goals and targets and to reduce human suffering and pain caused by the harmful use of alcohol.
The SAFER initiative is a package of five evidence-based, high impact strategies which WHO recommends governments should prioritise to tackle alcohol-related harm:
Strengthen restrictions on alcohol availability.
Advance and enforce drink driving countermeasures.
Facilitate access to screening, brief interventions, and treatment.
Enforce bans or comprehensive restrictions on alcohol advertising, sponsorship, and promotion.
Raise prices on alcohol through excise taxes and pricing policies.
In terms of cost effectiveness of policies, WHO showed the best buys alcohol controls achieve high returns on investment: for every additional US$ 1 invested in the most cost-effective interventions per person per year will yield a return of US$ 9.13 by 2030, a return that is higher than a similar investment in tobacco control (US$ 7.43) or prevention of physical inactivity (US$ 2.80). The notion that economic savings are greater than implementation costs for effective alcohol control policies is supported by recent OECD estimates, showing that every US$ 1 invested in a comprehensive policy package yields a return of up to US$ 16 in economic benefits.[40]
The WHO report, No place for cheap alcohol: The potential value of minimum pricing for protecting lives[41], identifies minimum pricing policies as among the most effective measures for policy-makers to address alcohol-related harms through its potential to reduce alcohol consumption. The report illustrates how the effectiveness of minimum pricing of alcohol as a mechanism for reducing the health and social harms caused by alcohol is supported by a substantial body of evidence, drawing on direct evaluation studies as well as evidence from modelling studies.
How proposals meet Scottish Government policy objectives
The Scottish Government, in its National Performance Framework provides a clear vision for Scotland with broad measures of national wellbeing covering a range of economic, health, social and environmental indicators and targets. Given evidence on impact of minimum unit pricing of alcohol on health harms, the policy (as part of the wider Alcohol Framework) contributes primarily to the National Outcome We are Healthy and Active.
The National Performance Framework is underpinned by the internationally recognised United Nations Sustainable Development Goals. MUP has a key contribution to two key aspects of that framework and the National Performance Framework:
3.4 By 2030, reduce by one third premature mortality from non-communicable diseases through prevention and treatment and promote mental health and well-being.
3.5 Strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol.
There is strong evidence that a key contributor to health harms over recent decades has been alcohol consumption and that this, in turn, is partly driven by the affordability and availability of alcohol. The overall conclusion in the PHS final evaluation report on MUP is that the evidence supports that MUP has had a positive impact on health outcomes, namely an estimated reduction in alcohol-attributable deaths and likely to have reduced hospital admissions compared to what would have happened if MUP had not been in place. That is why the Scottish Ministers’ agreed position set out below is to retain minimum unit pricing of alcohol as part of our overall approach and range of policies to tackle alcohol-related harms through improved prevention and treatment.
Contact
Email: MUP@gov.scot
There is a problem
Thanks for your feedback