National Mission on Drugs: annual monitoring report 2022-2023
Provides an analysis of the progress made against the National Mission on Drugs between April 2022 and March 2023. This is aimed at reducing the number of drug-related deaths and improving the lives of people affected by drugs in Scotland.
6. Outcome 2: Risk is reduced for people who use harmful drugs
6.1 Summary
Outcome 2: Risk is reduced for people who take harmful drugs
There were 3,641 ambulance service naloxone administrations in 2022/23
- This was a decrease of 26% since 2021/22, and represents a decreasing trend since the start of the National Mission
There were 235 drug-related hospital stays per 100,000 in 2021/22
- This was a decrease of 13% since 2020/21. Data for 2022/23 are not yet available
The data are indicative of a mixed picture regarding whether risk is reduced for people who take harmful drugs. More information is needed to draw conclusions from drug-related hospital admissions in particular.
6.2 Background
Targeted harm reduction interventions are vital at all parts of a person’s recovery journey and are known to reduce the likelihood of a drug related death. Naloxone is a medicine used to prevent fatal opioid overdoses and is carried by all Scottish Ambulance Service (SAS) staff. Both SAS naloxone administration data and data on drug related hospital stays provide an insight into the level of acute harms associated with problem drug use experienced by people in the community. Other community-based initiatives to reduce risk are wide-ranging and are aimed at promoting safer drug consumption practices and reducing the harms caused by injecting drug use – including blood borne viruses, injection site injuries and infection, and overdoses. Access to harm reduction is also a core part of the Medication Assisted Treatment (MAT) Standards.
6.3 Headline metrics
6.3.1 Headline metric: Number of ambulance service naloxone administrations
In 2022/23[19] there were 3,641 incidents in which naloxone was administered by Scottish Ambulance Service (SAS) clinicians. This was 26% (1,251) fewer than in 2021/22[20] when there were 4,482 incidents (Figure 4).
Figure 4 : There has been a decreasing trend in the number of ambulance service naloxone administrations since mid-2021
Number of naloxone administration incidents reported by the Scottish Ambulance Service, 2019 to 2022
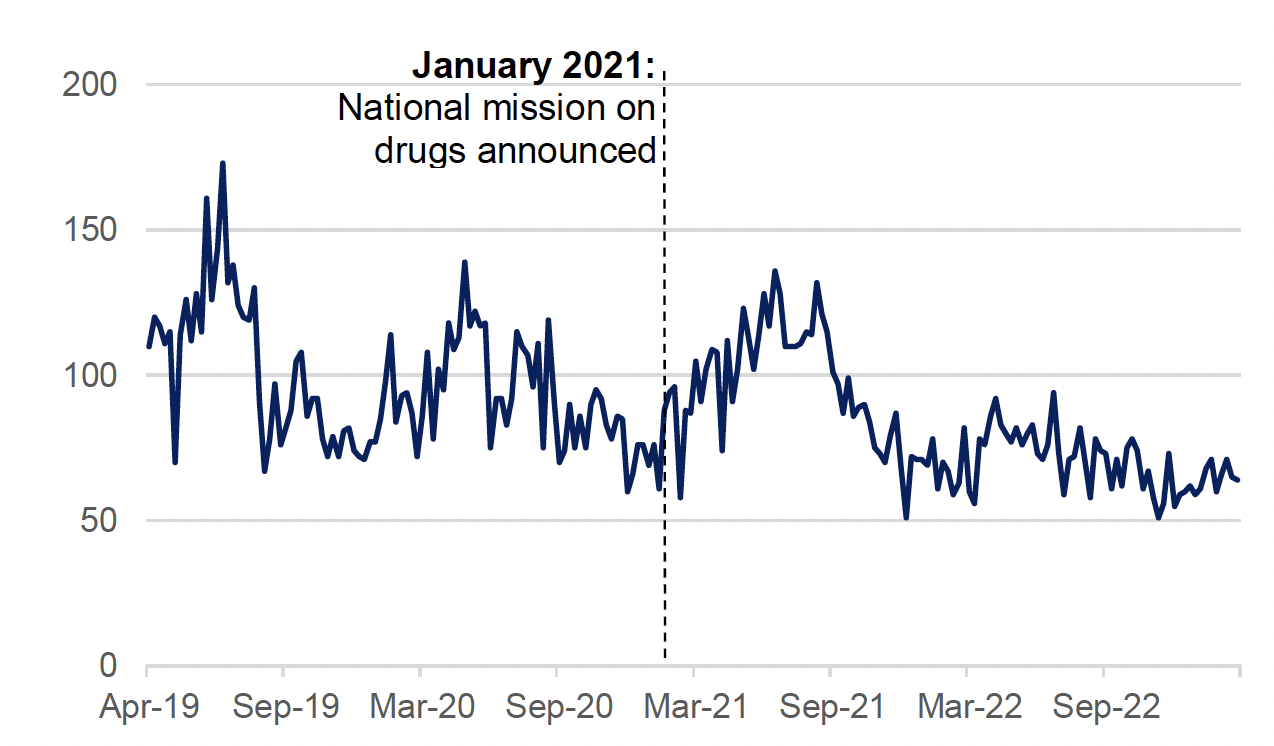
Source: Rapid Action Drug Alerts and Response (RADAR) quarterly report, Public Health Scotland, October 2023
The latest surveillance data suggests that there has recently been an increasing trend in the number of SAS naloxone administrations. There were 2,005 SAS naloxone administration incidents over the first 23 weeks of 2023/24 (the most recent data available), an increase of 15% (255) compared to the same period in 2022/23.[21]
Data on the administration of naloxone must be interpreted in the context of the significant activity undertaken in recent years to increase the distribution and carriage of naloxone in Scotland. The distribution of kits to people at risk has remained the priority, but further work specifically targeting peers of people using drugs, family members and emergency services has also been undertaken with partners. This increased availability of naloxone and wider range of people who may be carrying and administering naloxone (in both professional and non-professional settings) is likely to have had an impact on the number of SAS naloxone administrations.
6.3.2 Headline metric: Rate of drug-related hospital stays
During 2021/22 (the most recent data available) the age-standardised rate of drug-related hospital stays was 235 per 100,000 (Figure 5). This is a decrease of 13% compared to 2020/21 (270 stays per 100,000).
Figure 5: The drug-related hospital stay rate has decreased since 2019/20
Age-standardised rate of drug related hospital stays per 100,000 (any hospital type), 2019/20 to 2021/22
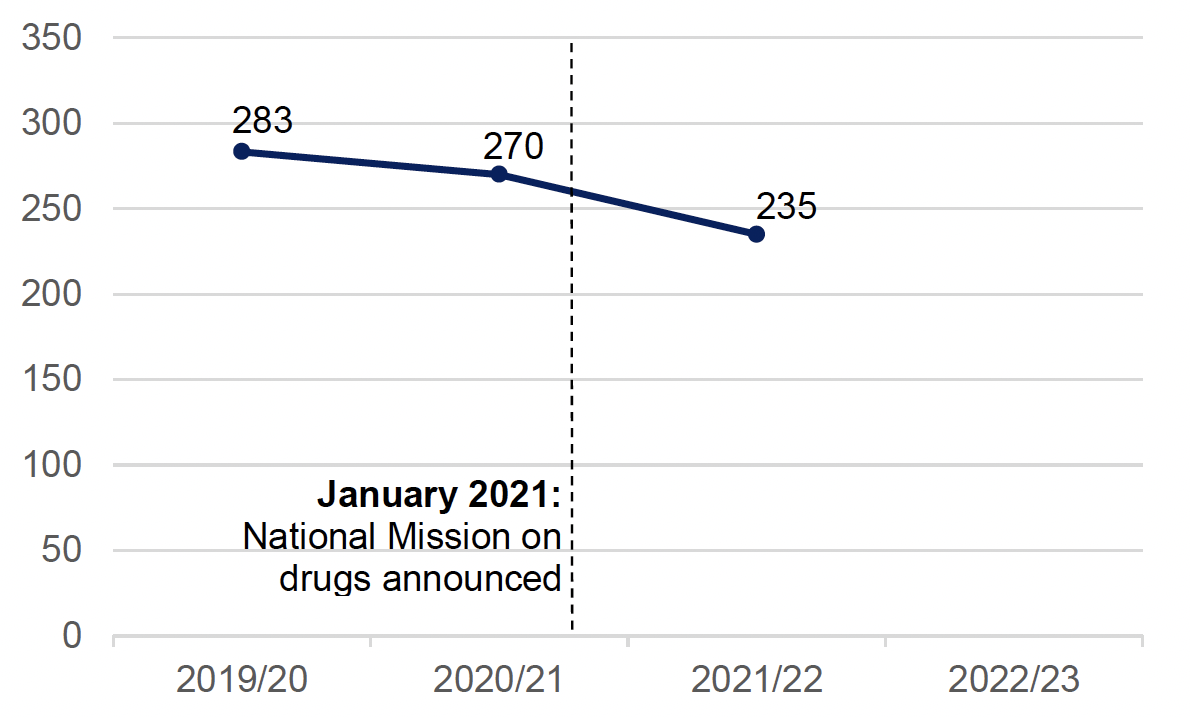
Source: Drug-related hospital statistics 2021 to 2022, Public Health Scotland, November 2022
Statistics for this metric for 2022/23 have not yet been published. However, RADAR reports weekly management information data on the number of acute drug-related hospital admissions[22] that provide some insight into more recent trends. After a decreasing trend from mid-2021 to the end of 2022, acute drug-related admissions have been increasing in recent months. It should be noted that this excludes psychiatric hospital admissions, which typically make up between 12% and 18% of total drug-related hospital admissions.
It is difficult to draw direct conclusions from changes in drug-related hospital admissions. The observed decreasing trend in admissions may not directly reflect a reduction in harms. The rate of hospital admissions may be affected by broader barriers experienced by people in accessing urgent care services and the capacity of hospital services more generally. Alternatively, it may be that people die before being admitted to hospital. However, it is not possible to conclusively determine whether this more recently observed increase in the rate of acute hospital admissions indicates a genuine rise in drug harms (for example changing risks and harms from evolving drug markets, polydrug use and emerging synthetic opioids), or that more people are accessing these services, thereby potentially resulting in previously unmet need being addressed.
6.4 Supporting metrics
6.4.1 Supporting metric: Number of new hepatitis C infections
There were 1,018 new diagnoses of hepatitis C antibody positivity in Scotland in 2022/23 (Figure 6). This is a decrease of 60 (6%) compared to 2021, when there were 1,078 new hepatitis C infections recorded, and represents one of the lowest annual totals on record.
Figure 6: The number of new hepatitis C infections in 2022 is comparable to the total numbers newly diagnosed in recent years since the COVID-19 pandemic
Number of new diagnoses of hepatitis C antibody positivity in Scotland, 2019 to 2022
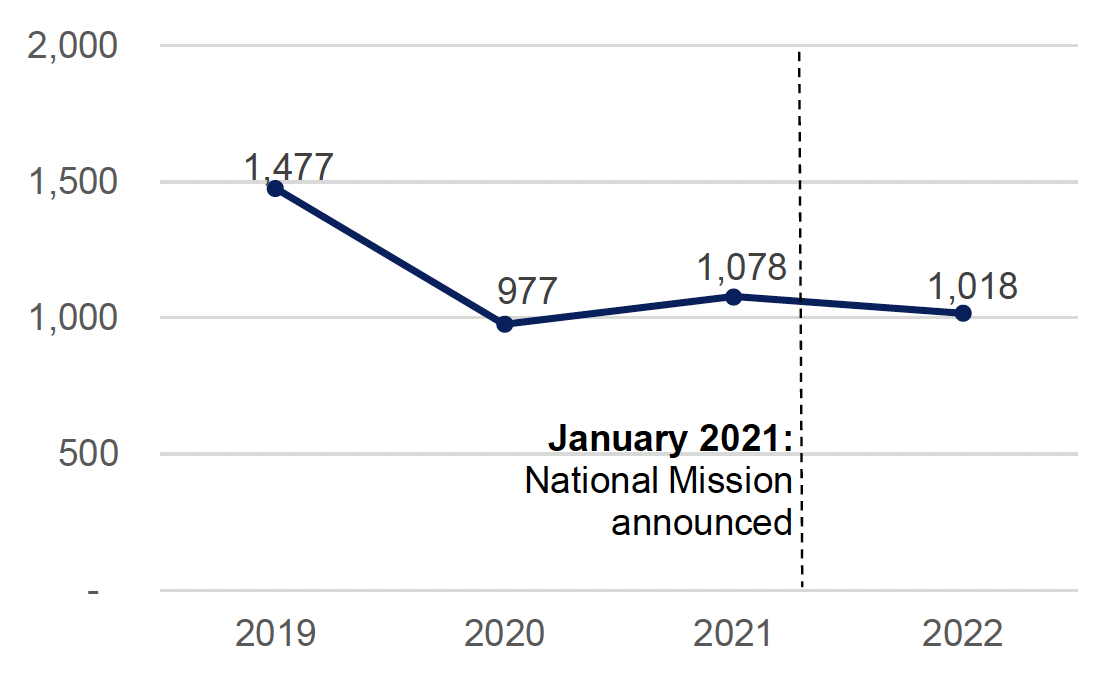
Source: Surveillance of hepatitis C in Scotland: Progress on elimination of hepatitis C as a major public health concern 2023 update, Public Health Scotland, December 2023
6.4.2 Supporting metric: Number of needles/syringes distributed per injecting equipment provision outlet attendance
An average of 17.6 needles/syringes were distributed per attendance at injecting equipment provision (IEP) outlets in 2022/23. This is a slight increase compared to 2021/22 when the average was 16.7 needles/syringes per attendance (Figure 7).[23]
Figure 7: The number of needles/syringes distributed per IEP attendance has increased slightly since the start of the National Mission
Number of needles and syringes distributed per IEP attendance, 2019/20 to 2022/23
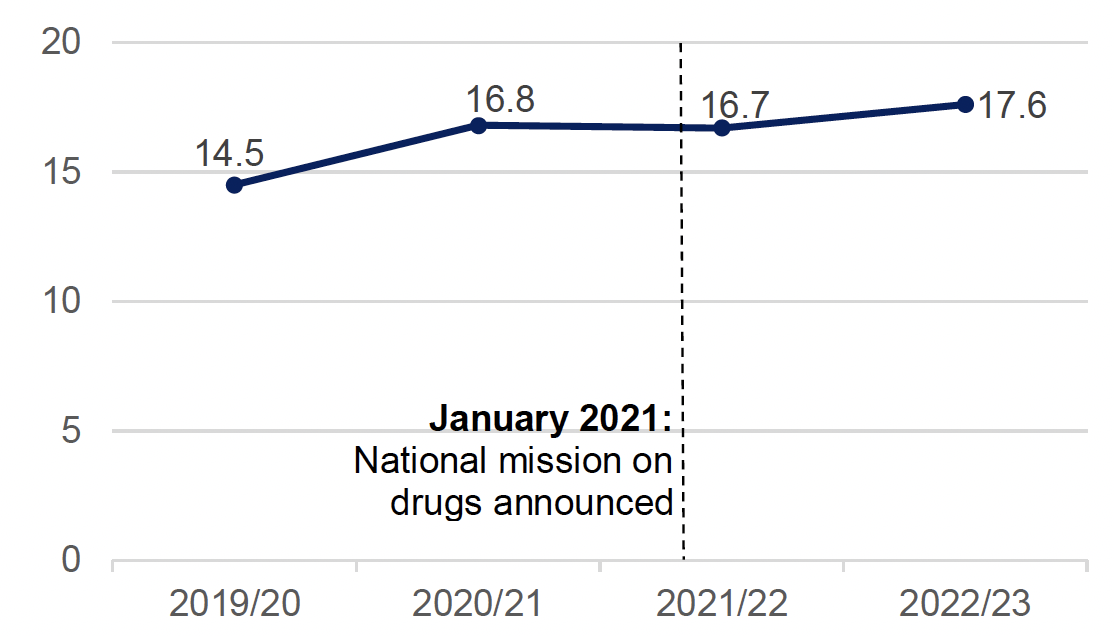
Source: Injecting equipment provision in Scotland 2022 to 2023, Public Health Scotland, September 2023
Changes to IEP services were implemented as part of the COVID-19 mitigation measures in early 2020 (for example changes in the availability of IEP services due to staff absence, asking service users to attend IEP services less often, and encouraging clients to take away additional supplies at each attendance). These changes may have contributed to the levels of IEP attendance and average number of needles/syringes distributed per attendance in 2019/20 and 2020/21.
Data around the number of IEP outlets and attendances provide additional context on IEP harm reduction activity. The number of attendances at IEP outlets has decreased steadily over the last ten years. However, this decrease is not correlated with a reduction in the number of IEP outlets, and the number of outlets reporting IEP provision has been fairly stable over recent years (there were 330 IEP outlets in 2022/23). Possible explanations for the decline in attendances includes changes in data recording, and changes in the accessibility and acceptability of IEP services to people who could benefit from them. Changes in the type of drugs being used or in the availability of alternatives to injecting are likely to be factors in the changing demand for injecting equipment. Data from the Drug and Alcohol Information System (DAISy)[24] suggests that, among people starting specialist treatment for drug use, the percentage of people reporting having injected drugs in the month prior has decreased from 28% in 2006/07 to 11% in 2022/23.[25],[26]
6.4.3 Supporting metric: Naloxone programme reach
In 2022/23, the ‘reach’ of the National Naloxone Programme (percentage of people at risk of an opioid overdose who have been supplied with take home naloxone[27]) was 70.4% (Figure 8). This is an increase of nearly six percentage points since 2021/22 (64.8%) and over 20 percentage points compared to 2019/20 (50.2%). The reach of the National Naloxone Programme has continually increased since data collection began.
Figure 8: The reach of the National Naloxone Programme has increased markedly since 2019/20
Reach of Scotland’s National Naloxone Programme, 2019/20 to 2022/23
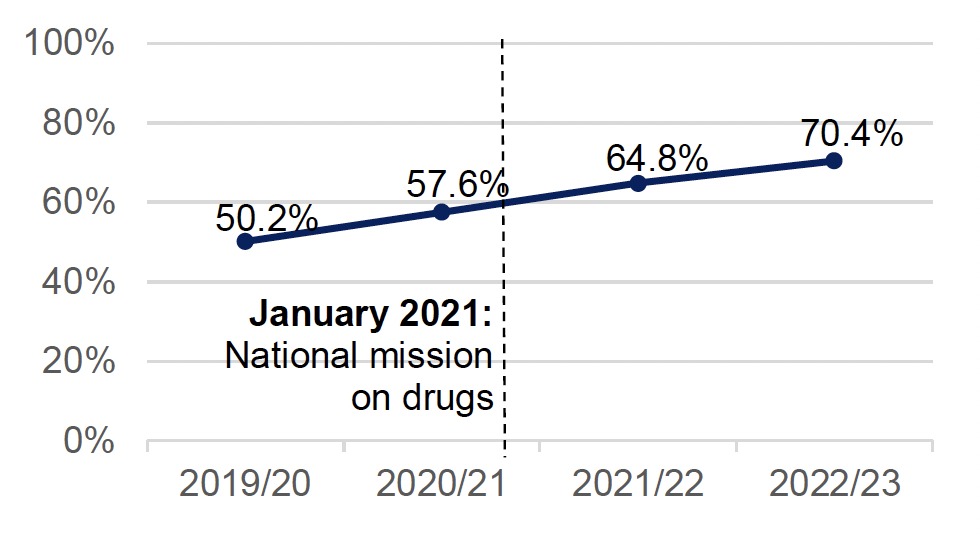
Source: National Naloxone Programme Scotland - Quarterly monitoring bulleting January to March 2022/23, Public Health Scotland, September 2023
6.4.4 Supporting metric: Percentage of ADP areas where MAT standard 4 has been fully implemented
In 2023, 18 out of 29 ADP areas (62%) had fully implemented MAT standard 4 (all people are offered evidence-based harm reduction at the point of MAT delivery). This is an increase of 10 ADPs areas since 2022 (Figure 9). Of the 18 ADP areas where the standard was reported as fully implemented in 2022, 4 were assessed as ‘green’ and 14 as ‘provisional green’.[28] While this does not provide measurement of outcomes, it does show the progress that ADPs across Scotland have made in implementing this standard within local areas.
Figure 9: Over the last year, ADPs have made substantial progress with implementation of MAT standard 4
Percentage of ADP areas where MAT standard 4 is reported as fully implemented (‘green’ or ’provisional green’), 2022 & 2023
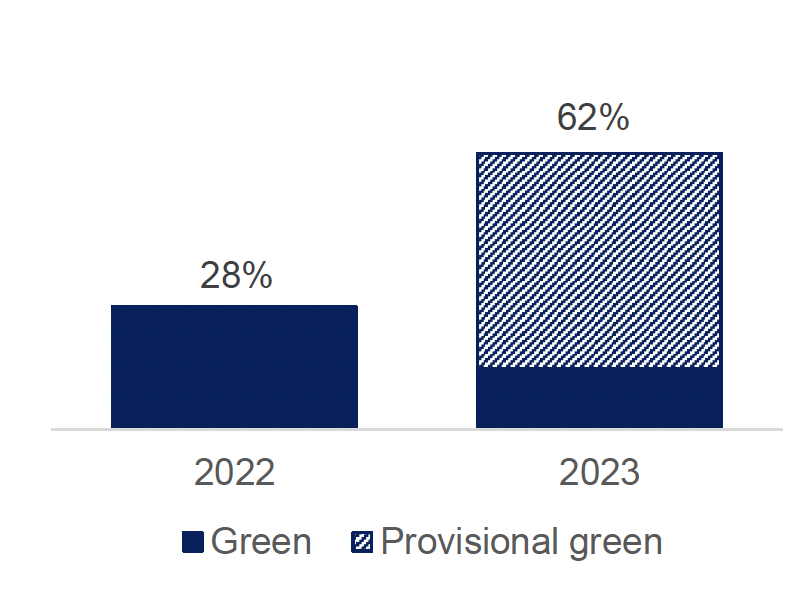
Source: National benchmarking report on implementation of the medication assisted treatment (MAT) standards 2022/23, Public Health Scotland, June 2023
The proportion of ADPs assessed as ‘green’ decreased between 2022 and 2023. This is explained by a change in methodology (stricter criteria in 2023 than 2022) and the introduction of the ‘provisional green’ category.
6.4.5 Supporting metric: Percentage of ADP areas offering specific harm reduction services
In 2022/23, in drug service settings (NHS, third sector and council):
- All ADP areas reported offering supply of naloxone.
- All but one ADP area (97%) reported offering hepatitis C testing.
- All ADP areas reported offering injecting equipment provision.
- All ADP areas reported offering wound care.
6.5 Discussion
The data are indicative of a mixed picture regarding whether risk is reduced for people who take harmful drugs. More information is needed to draw conclusions from drug-related hospital admissions in particular.
Naloxone administrations by the ambulance service have been falling since the start of the National Mission in January 2021. The drug-related hospital stay rate has also decreased over this period. However, this may not directly indicate a reduction in harms. The reduction in SAS naloxone administrations must be interpreted in the context of activities undertaken to increase the availability and carriage of naloxone in Scotland’s communities, following which the administration of naloxone by peers, family and other emergency services is likely to have increased. Hospital admissions may be affected by broader barriers experienced by people in accessing urgent care services and the capacity of hospital services more generally. More recent data also suggest that the number of both ambulance service naloxone administrations and drug-related hospital admissions are now increasing.
The supporting metrics provide a more encouraging picture of progress towards reducing risk for people who use harmful drugs. More people at risk of drug death have a naloxone kit as the reach of the National Naloxone Programme has been steadily rising. There is also continued engagement with IEP outlets and wide availability of other harm reduction services such as naloxone provision, wound care, and Hepatitis C testing across ADP areas. The number of ADP areas where MAT standard 4 has been fully implemented has more than doubled to over 6 in 10. Finally, progress continues to be made on hepatitis C elimination targets in Scotland, with the number of new hepatitis C infections in 2022 one of the lowest annual totals recorded in the last decade.
Taken together, this is indicative of a mixed picture. More information is needed to draw conclusions from drug-related hospital admissions in particular. Other data improvements that would support monitoring of outcome 2 include insight into naloxone administration by peers, family, and other emergency services, and near-fatal overdose incidents and outcomes.
Contact
There is a problem
Thanks for your feedback