National Mission on Drugs: annual monitoring report 2022-2023
Provides an analysis of the progress made against the National Mission on Drugs between April 2022 and March 2023. This is aimed at reducing the number of drug-related deaths and improving the lives of people affected by drugs in Scotland.
7. Outcome 3: People most at risk have access to treatment and recovery
7.1 Summary
Outcome 3: People most at risk have access to treatment and recovery
There were 14,055 referrals resulting in treatment starting in 2022/23
- This was a decrease of 8% since 2021/22. Stable but with some variation since the start of the National Mission
100% of ADP areas had referral pathways in place in 2022/23 for people who experience a near-fatal overdose
- This is the first year for which data is available
7.2 Background
Evidence has shown that receiving treatment and being known to services are protective factors against drug-related deaths and harms[29],[30] and so it is important to better understand the pathways into treatment. For people at most risk of drug related-related death and harm, this can be explored using existing data on the number of referrals to have successfully resulted in starting treatment and data on near-fatal overdose (NFO) pathways. As part of understanding pathways to treatment and recovery it is important to understand how long people have to wait before they receive support. It is also important to understand how people at risk are proactively identified and offered support (MAT3), and how different pathways operate such as pathways between the criminal justice system and specialist services.
7.3 Headline metrics
7.3.1 Headline metric: Number of referrals resulting in treatment starting
There were 14,055 referrals resulting in community-based specialist drug or co-dependency treatment starting in 2022/23 (Figure 10).[31] This is 8% (1,141) fewer than in 2021/22, when 15,196 referrals resulted in treatment starting.
Figure 10 : The number of referrals resulting in the start of specialist treatment has varied quarter on quarter but remains at a similar level to the start of the National Mission
Number of referrals resulting in specialist treatment starting (completed waits) for drugs and co-dependency, community settings, 2019/20 to 2022/23
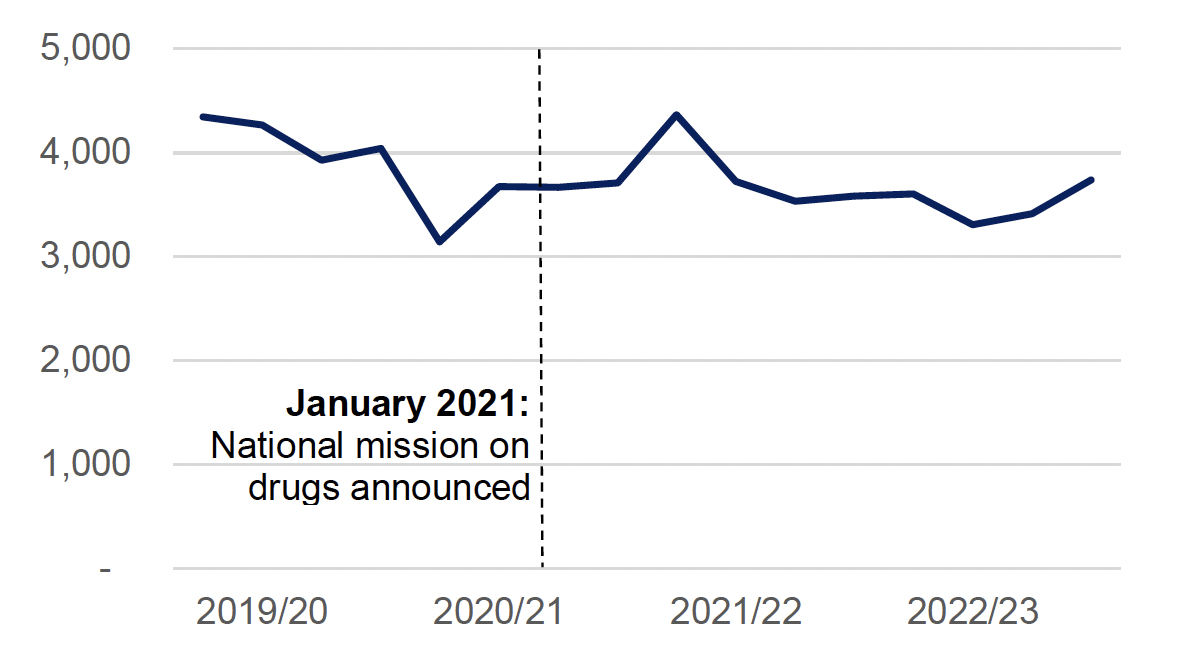
Source: National drug and alcohol treatment waiting times 1 April 2023 to 30 June 2023, Public Health Scotland, September 2023
There was a general downward trend in the number of referrals starting treatment since March 2019. This was exacerbated following the first COVID-19 lockdown measures implemented in March 2020, which affected referrals and the delivery of treatment through changes to service provision (for example less face-to-face interaction).[32] Following a spike in the first quarter of 2021/22,[33] the number of referrals resulting in treatment starting fluctuated quarter on quarter but remained broadly flat, with a slight increase in the final quarter of 2022/23.
Additional data provide insight about referrals for treatment for people in prison settings. In 2022/23, 1,433 referrals resulted in the start of specialist treatment for drug and co-dependency in prison settings. This is 20% (362) fewer than in 2021/22, when 1,795 referrals resulted in the start of treatment.
7.3.2 Headline metric: ADP areas where referral pathways are in place for people who experience a near-fatal overdose
In 2022/23, all ADPs reported having referral pathways in place in their area to ensure people who experience a near-fatal overdose are identified and offered support.[34] Moreover, every ADP also reported that people who have experienced a near-fatal overdose have been successfully referred using this pathway. This question was first included in the ADP Survey in 2022/23,[35] so is not comparable with historical data.
Caution must be exercised when interpreting these data – although near fatal overdose pathways are in place in all ADP areas across Scotland, the data does not provide any insight into the accessibility, use, or outcomes of people who are referred through these pathways.
7.4 Supporting metrics
7.4.1 Supporting metric: Percentage of referrals resulting in treatment starting within three weeks or less
In 2022/23, 92% of referrals for community-based specialist drug or co-dependency treatment resulted in treatment starting within three weeks or less. This is in line with 2021/22, but lower than in 2020/21 when 95% of referrals resulting in treatment starting within three weeks or less.[36]
The average wait time for community-based specialist drug treatment in 2022/23 was five days, a decrease from six days in 2021/22. The average wait time for community-based specialist co-dependency treatment was seven days in 2022/23, the same as in 2021/22.[37]
The waiting time standard that 90% of people should wait no longer than three weeks for specialist treatment is consistently met at a national level. However, there is substantial geographic variation. Only four NHS boards[38] have consistently met the waiting times target for both drugs and co-dependency every quarter since the start of the National Mission. By contrast, performance in other health boards is mixed.
The most common type of treatment in 2022/23 was structured preparatory intervention, which accounted for 46% and 52% of treatments started for drugs and co-dependency respectively. The second most common treatment type was structured psychosocial intervention, accounting for 31% and 38% of treatments started for drugs and co-dependency respectively. These two treatment types have accounted for the majority of new treatments started since 2019/20.
7.4.2 Supporting metric: Percentage of ADP areas where MAT standard 3 has been fully implemented
In 2023, 14 out of 29 ADP areas (48%) had fully implemented MAT standard 3 (all people at high risk of drug-related harm are proactively identified and offered support to commence or continue MAT). This is an increase of 8 ADP areas since 2022 (Figure 11). Of the 14 ADP areas where the standard was reported as fully implemented in 2023, 1 ADP area was assessed as ‘green’ and 13 as ‘provisional green’.[39]
Figure 11: Over the last year, ADPs have made substantial progress with implementation of MAT standard 3
Percentage of ADP areas where MAT standard 3 is reported as fully implemented (‘green’ or ’provisional green’), 2022 & 2023
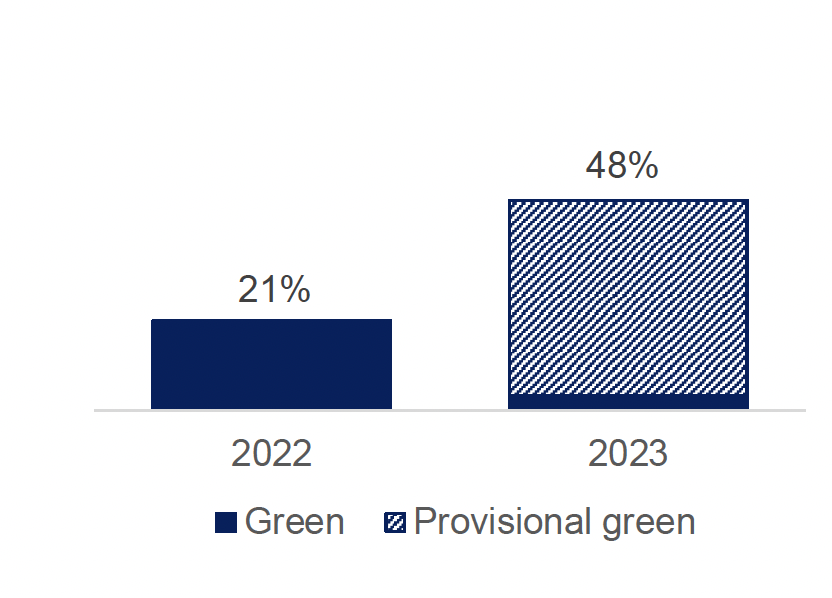
Source: National benchmarking report on implementation of the medication assisted treatment (MAT) standards 2022/23, Public Health Scotland, June 2023
The proportion of ADPs assessed as ‘green’ decreased between 2022 and 2023. This is explained by a change in methodology (stricter criteria in 2023 than 2022) and the introduction of the ‘provisional green’ category.
7.4.3 Supporting metric: Percentage of ADP areas supporting referrals within the criminal justice system to specialist treatment services
The percentage of ADP areas reporting that they fund or support referrals to substance use services in 2022/23 varied depending on the stage of engagement with the criminal justice system:
- Pre-arrest: 38%
- In police custody: 66%
- Upon release: 79%
- Community justice settings: 72%[40]
2022/23 was the first year this question was asked in the ADP Survey.
7.5 Discussion
The metrics present a fairly stable picture of access to treatment and recovery services, with evidence that processes within these pathways are improving.
The number of referrals resulting in the start of specialist treatment for drugs and co-dependency remains at a similar level to the start of the National Mission. While this indicates that there are active referral pathways in place, determining the extent to which people who are most at risk of drug related harms and death therefore have access to treatment and recovery is challenging based on the data currently available. At a national level, waiting times performance consistently exceeds the target level, as has been the case for a number of years. However, the variation in waiting times across the country suggests there are differences in people’s access to specialist treatment. PHS is currently undertaking analysis into recent trends in referrals to specialist drug and alcohol treatment services in Scotland, which will provide more insight into this area (data are expected in the summer of 2024).
All ADP areas reported having near-fatal overdose referral pathways in place, but no nationally comparable data are available to assess how accessible these pathways are, how many people have used them, and what their outcomes are.
Referral pathways between criminal justice settings and specialist treatment services are focused on supporting people who are among those at highest risk of drug related harms. Evidence at the ADP level indicates variation in support for referrals to specialist treatment services at the different stages of a person’s engagement with the justice system. ADPs support specialist drug treatment referrals at relatively high levels at the police custody stage, upon release and in community justice settings, but support pre-arrest is less widely available.
ADPs have also made substantial progress implementing MAT standard 3, which focuses on proactively identifying and offering support to engage with MAT for people at a high risk of drug-related harm. People at risk of drug-related harms often experience multiple concurrent risk factors, and risk assessment remains a major challenge for services. However, evidence collected as part of the MAT standards benchmarking exercise[41] demonstrates that some progress is being made to increase access to treatment for people most at-risk.
Overall, the metrics present a fairly stable picture of access to treatment and recovery services. There is evidence that processes within these pathways are improving, with substantial progress on the implementation of MAT standard 3.
Contact
There is a problem
Thanks for your feedback