National Mission on Drugs: annual monitoring report 2022-2023
Provides an analysis of the progress made against the National Mission on Drugs between April 2022 and March 2023. This is aimed at reducing the number of drug-related deaths and improving the lives of people affected by drugs in Scotland.
9. Outcome 5: Quality of life is improved by addressing multiple disadvantages
9.1 Summary
Outcome 5: Quality of life is improved by addressing multiple disadvantages
Adults who had used drugs in the last 12 months reported a mental wellbeing score of 45.4 in 2021
- This is the first year for which this data is available
People in the most deprived areas were 15.9 times more likely to die of a drug death compared to people in the least deprived areas in 2022
- This remains broadly unchanged since the start of the National Mission
9.2 Background
People with problem substance use often have complex needs and/or other comorbidities and so require support from multiple services. The effects of deprivation, homelessness, trauma, and co-occurring mental health problems on a person are known to be compounding factors that can greatly affect quality of life and the harms associated with substance use. National and local initiatives aimed at addressing these disparities include agreeing formal joint working protocols at an ADP level to support people with co-occurring substance use and mental health diagnoses to receive mental health care; the development of trauma-informed workforce and services; and the implementation of the MAT standards.
9.3 Headline metrics
9.3.1 Headline metric: Mental wellbeing score for adults who have used drugs
Adults who reported having used any drug in the last 12 months in 2021 had a significantly lower mental wellbeing score on average than those who did not report having used drugs in the last 12 months (Figure 15). Similar patterns were recorded among both males and females.[54], [55]
Figure 15 : Adults who had used drugs in the past 12 months reported lower mental wellbeing scores than those who did not report having used drugs
WEMWBS scores, adults who reported they had used drugs in last 12 months and adults who did not report having used drugs in the past 12 months
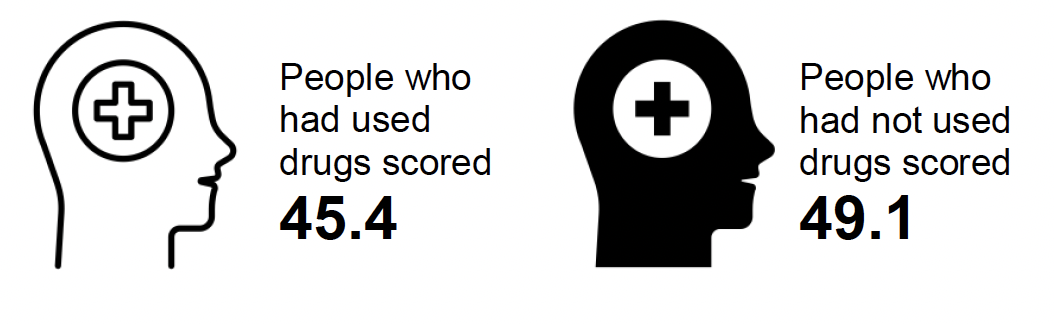
Source: Scottish Health Survey 2021, Scottish Government, November 2022
Questions on drugs were included in the Scottish Health Survey for the first time in 2021. These questions will be included biennially and will provide a measure of how mental wellbeing among adults who have used drugs in the past 12 months changes over time.
9.3.2 Headline metric: Ratio of drug death rate in the most deprived areas to rate in the least deprived areas
The age-standardised drug misuse[56] death rate for people living in the most deprived areas[57] was 15.9 times higher than in the least deprived areas in 2022 (52.4 and 3.3 per 100,000 respectively) (Figure 16). This is a slight increase compared to 2021 when the ratio was 15.3). The drug death deprivation ratio was highest in 2019 at 19.6, and lowest in 2011 at 8.4.
Figure 16: The deprivation ratio increased slightly in 2022 but is lower than its peak in 2019
Ratio of age-standardised drug misuse death rate per 100,000 in the most deprived quintile to that in the least deprived quintile, 2019-2022
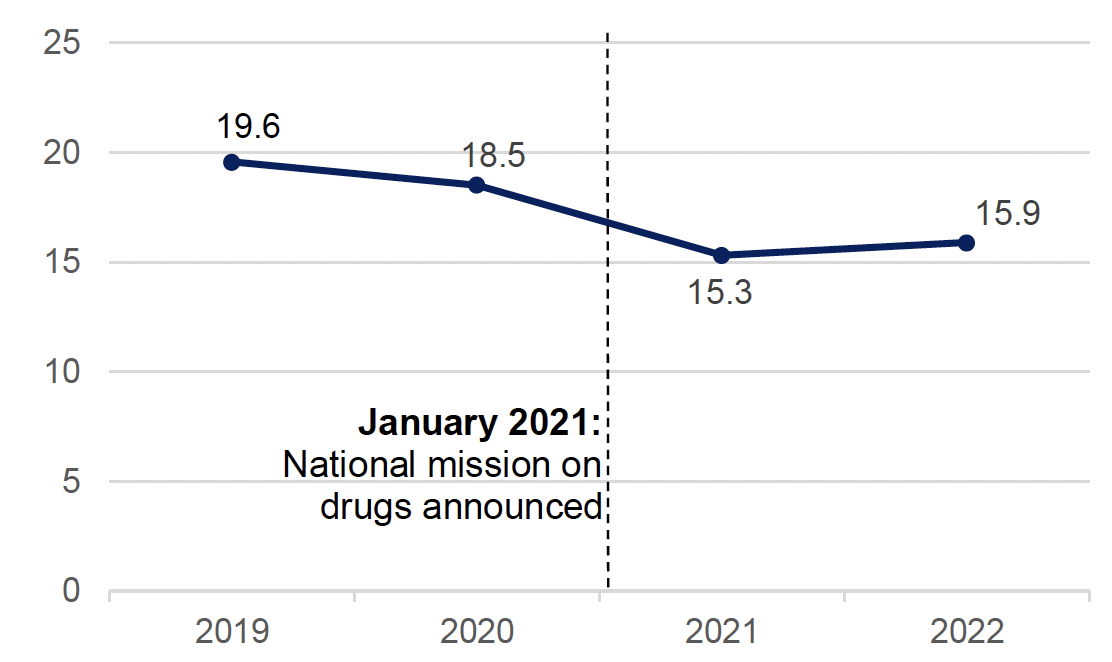
Source: Drug-related deaths in Scotland 2022, National Records of Scotland, August 2022
The ratio of the drug death rate in the most deprived areas to the rate in the least deprived areas has narrowed slightly since the start of the National Mission, but it is far higher than for all-cause deaths: people in the most deprived areas are around twice as likely to die from all-causes as those in the least deprived areas.
9.4 Supporting metrics
9.4.1 Supporting metric: Ratio of drug-related hospital stay rate in the most deprived areas to rate in the least deprived areas
In 2021/22 (the most recent data available), the drug-related hospital stay rate for people who live in the most deprived areas[58] was 15.3 times higher than for those in the least deprived areas (612.5 and 40.2 per 100,000 respectively) (Figure 17). This is a slight increase from 2021 when the ratio was 14.9. Approximately half of patients with a drug-related hospital stay lived in the 20% most deprived areas in Scotland.
Figure 17 : The ratio of the drug-related hospital stay rate in the most deprived areas to that in the least deprived areas has reduced slightly but remains high
Ratio of age-standardised drug-related hospital stay rate per 100,000 in the most deprived quintile to that in the least deprived quintile, 2019/20 to 2021/22
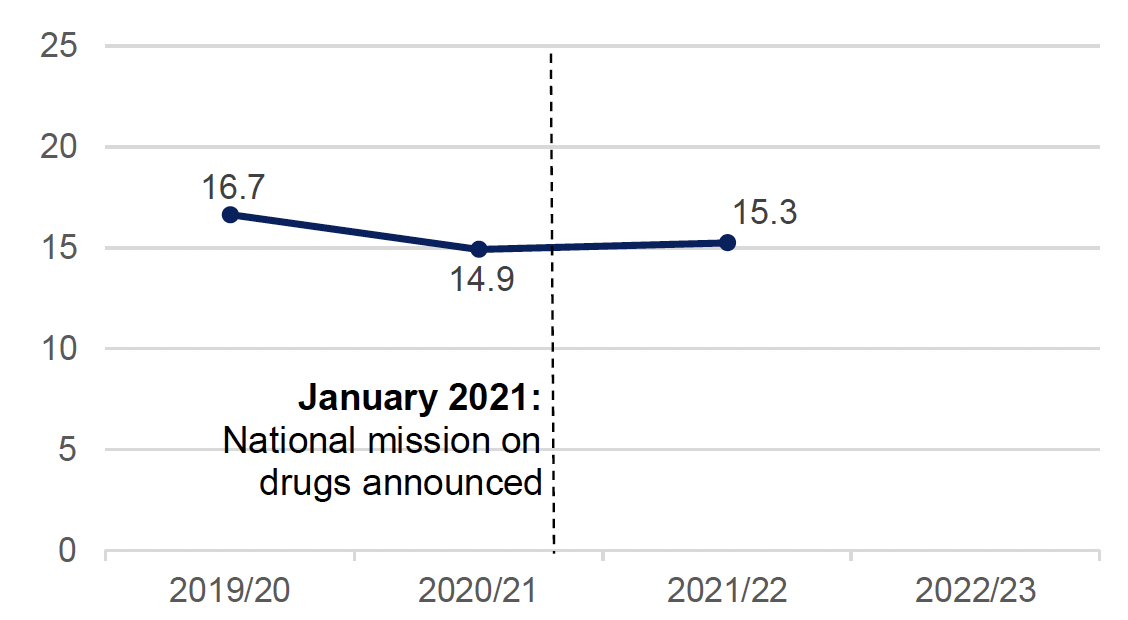
Source: Drug-related hospital statistics in Scotland 2021 to 2022, Public Health Scotland, November 2022
The ratio of the drug-related hospital stay rate for people living in the most deprived areas to the rate for those living in the least deprived areas has narrowed slightly since the start of the National Mission. However, it is far higher than for hospital stays from all causes, where people living in the most deprived areas are almost twice as likely to have a hospital stay as those living in the least deprived areas.[59]
9.4.2 Supporting metric: Number of drug deaths amongst people experiencing homelessness
There were an estimated[60] 89 people experiencing homelessness who died of drug misuse[61] in Scotland in 2022, a decrease of 38 (30%) compared to 2021 when there were 127 such deaths (Figure 18). In 2022, 36% of all homeless deaths were due to drug misuse, down from 51% in 2021 and 59% in 2020.
Figure 18: Following a steady increase in recent years, the number of drug deaths of people experiencing homelessness has declined since 2020
Estimated number of homeless drug misuse deaths, 2019 to 2022
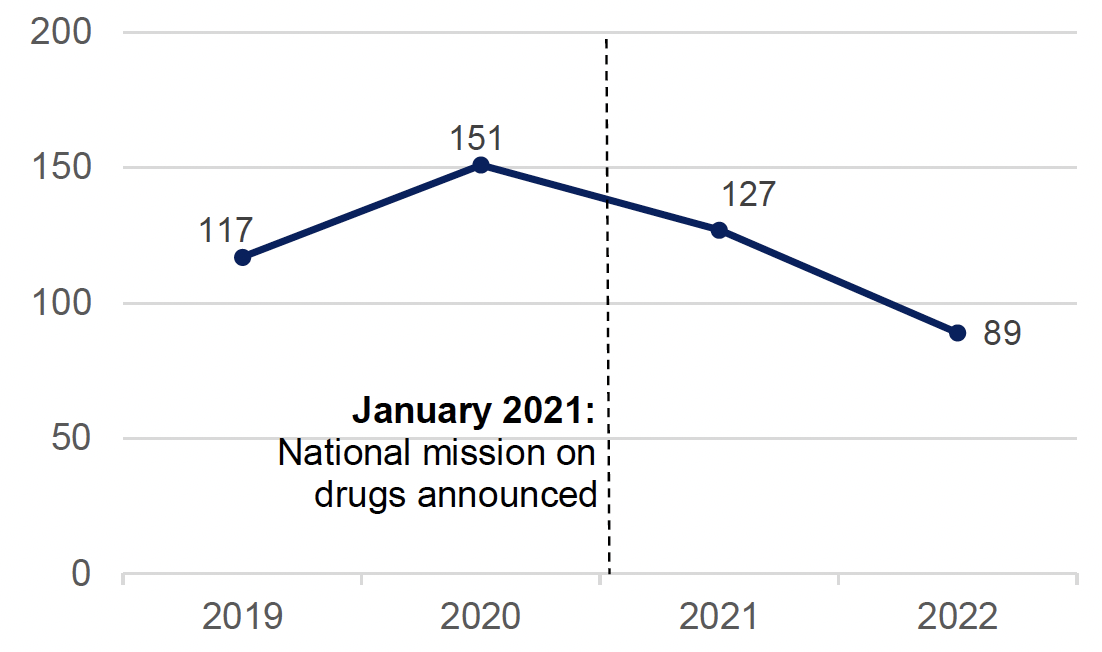
Source: Homeless deaths 2022, National Records of Scotland, November 2023
Drug deaths amongst people experiencing homelessness have declined since the National Mission began.
9.4.3 Supporting metric: Number of homeless households with a drug or alcohol dependency support need
There were 3,151 households[62] assessed as homeless or threatened with homelessness where drug or alcohol dependency support needs were identified in 2022/23 (Figure 19).[63] This is similar to 2021/22 when there were 3,184 such households.
Drug or alcohol dependency support needs were most common among people aged between 35 and 49 years. These trends contrast with overall increases observed in the number of households assessed as homeless since 2020/21.
Figure 19 : The number of homeless households with a drug or alcohol dependency support needs is relatively unchanged since the start of the National Mission
Number of homeless households where a drug or alcohol dependency support need was identified, 2019/20 to 2022/23
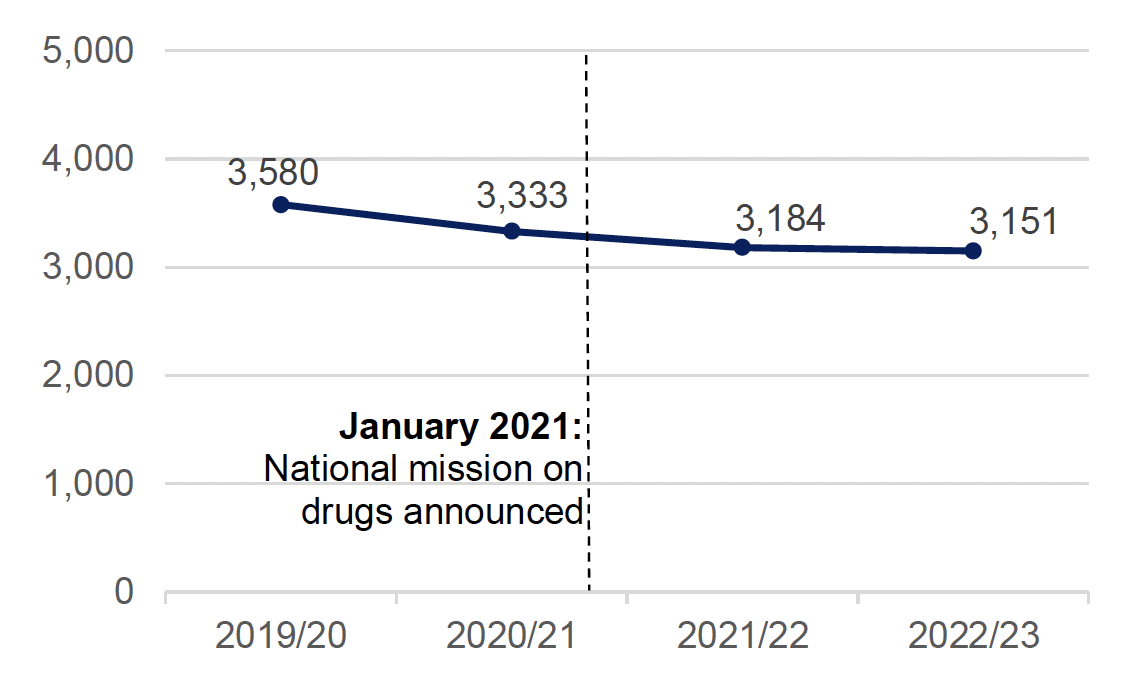
Source: Homelessness in Scotland 2022-23, Scottish Government, August 2023
The number of homeless households with a drug or alcohol dependency support need has been gradually declining since before the start of the National Mission.
9.4.4 Supporting metric: Percentage of ADP areas with formal joint working protocols with mental health services
In 2022/23, 59% of ADP areas reported that they had formal joint working protocols in place to support people with co-occurring substance use and mental health diagnoses to receive mental health care.[64] This is an improvement compared to 2021/22 when only a minority of ADP areas reported that they had these protocols in place.[65]
The ADP areas that did not have joint working protocols in place in 2022/23 indicated that these were in development, for example through establishing steering groups to formalise guidance and pathways around joint working, and ensuring a whole systems approach towards meeting needs of individuals with co-occurring diagnoses. Several ADPs specifically mentioned the development of these working protocols in relation to implementing MAT standard 9 (all people with co-occurring drug use and mental health difficulties can receive mental health care at the point of MAT delivery).
9.4.5 Supporting metric: Percentage of ADP areas undertaking activities to implement trauma-informed approach
All ADP areas reported that activities have been undertaken within local services in their areas in 2022/23 to implement a trauma-informed approach. Of these activities, every ADP reported training their existing workforce and 90% had engaged with third sector or community partners. ADPs also reported high rates of recruitment activity (83%), working groups (79%) and engaging with people with lived/living experience (76%).
9.5 Discussion
It is difficult to draw any firm conclusions on the progress towards improving quality of life by addressing multiple disadvantages. Drug-related mortality and hospital stays remain concentrated in the most deprived areas. Lower wellbeing is reported by people who have used drugs. There is some positive activity at the ADP level but more insight is needed directly from people using services.
There has been a wide range of individual policies and initiatives introduced as part of the National Mission to address the wider holistic needs of people who use drugs. Assessing the extent to which progress is being made in improving people’s quality of life and attributing this to any interventions associated with the National Mission, including any aimed at addressing multiple disadvantages, is therefore not possible in the context of this quantitative monitoring report. Short of attribution, it is possible to explore individual outcome measures (e.g. wellbeing) and rates of harms associated with disadvantage to understand if there has been any change since the start of the National Mission and, where possible, compare this to previous trend data.
Mental wellbeing provides a proxy measure for quality of life, and the recent Scottish Health Survey data on this measure for people who have recently used drugs provides a baseline for measuring progress in future years. Drug-related deaths and hospitalisations are heavily concentrated in Scotland’s most deprived areas and substantial inequalities remain despite the very slight narrowing of the deprivation gap since the start of the National Mission.
The effect of drug use and the associated harms on people experiencing homelessness – a population known to be associated with specific vulnerabilities and complex needs – provides insight into the extent of the progress being made towards improving the quality of life of people affected by drugs and experiencing multiple disadvantages. While the number of drug deaths among people experiencing homelessness have fallen since the start of the National Mission, they still represent over a third of the deaths in this population. The number of homeless households with a substance use support need has been gradually reducing since before the National Mission, but there remains a sizable demand for substance use-related support among people experiencing homelessness.
There is evidence of progress on activity at an ADP level. The vast majority of ADPs report that they are undertaking activities to implement a trauma-informed approach. Furthermore, the number of ADPs that report that they have formal joint working with mental health services in place to support people with co-occurring substance use and mental health diagnoses to receive mental health care has increased. Those without these protocols in place generally report that they are in development. These services will be crucial in tackling some of the multiple disadvantages people affected by drugs experience.
It is difficult to draw any firm conclusions on progress towards outcome 5. The burden of drug-related mortality and hospital stays remains heavily concentrated in Scotland’s most deprived areas. Adults who have recently used drugs report significantly lower mental wellbeing than those who have not used drugs, but there is no historical data enabling an assessment of change over time. While there is evidence of positive activity at an ADP level, more insight is needed directly from people using these services.
Contact
There is a problem
Thanks for your feedback