National Trauma Transformation Programme: workforce survey 2024
This report presents the main findings from a survey carried out with the workforce in Scotland exploring awareness and attitudes to psychological trauma and trauma-informed practice. The survey was carried out by the Improvement Service as part of the National Trauma Transformation Programme.
5. Barriers and Support
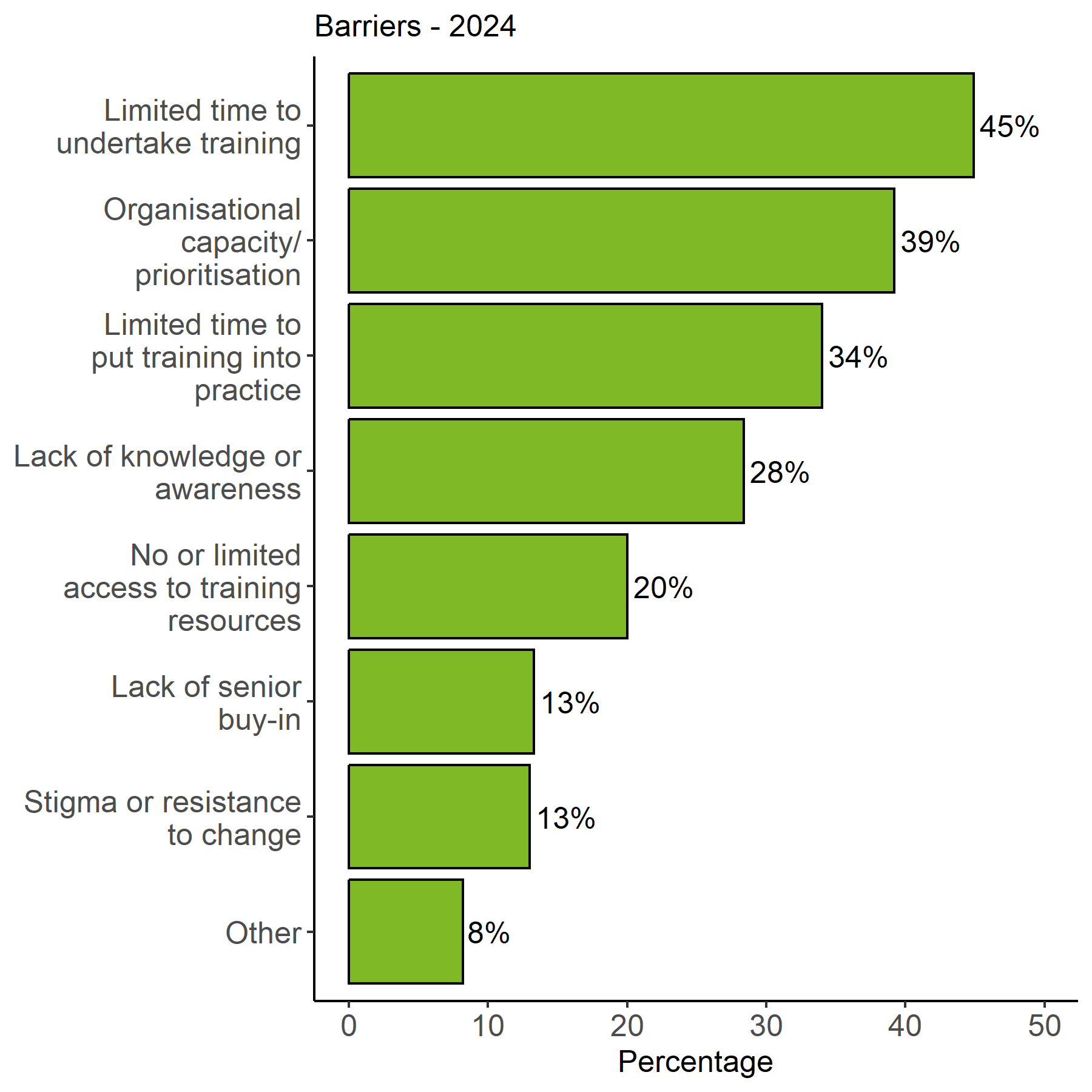
Respondents were asked to identify any barriers to working in a trauma-informed way, with a follow-up question that asked what support could help organisations or individuals to overcome these.
Respondents were provided with a multiple-choice range of potential barriers. The options used for this multiple-choice question were based on the most frequently cited responses in the previous iteration of the survey. Respondents could select more than one barrier and were also provided with an “other” option for barriers not included within the multiple-choice options.
The most common barriers highlighted were related to time and capacity, with almost 45 percent of respondents stating that “limited time to undertake training” was a barrier. Whilst lack of knowledge or awareness was less likely to be highlighted as a barrier this was still selected by 28 percent of respondents, suggesting more can be done to raise the profile of trauma-informed practice.
The proportion of respondents selecting each barrier are shown in Figure 21.
Respondent comments: “Implementing Trauma-informed practice is a long-term project and should be given the financial support and commitment to reflect the remit of the programme, to support sustained system change at a local level.”
The issues identified under “Other” included a lack of financial resources which featured very heavily. This included issues with paying for access to training, a limited number of staff to lead in this area, as well as long-term uncertainty, which meant there was an inability to commit long-term to embedding trauma-informed practice. Other issues included limited staff numbers; cultural challenges, including preconceptions about trauma; and physical challenges, such as the nature and number of spaces where services could be delivered. Many respondents did not feel that the topic was of relevance to them.
Respondents were asked to follow up with any further comments about these barriers. Some of the main themes and selected comments are shown below.
Limits to finance, staffing, and capacity were discussed by a large number of respondents who highlighted that this means that it is more difficult to attend and implement training. Some respondents noted that this has been exacerbated by the COVID-19 pandemic.
“Front line staff (and management) are experiencing unprecedented challenges in terms of resources and capacity at the same time of increasing demands on services. Staff are experiencing trauma (both personal and vicarious) this makes attending training and applying learning challenging. Lack of resources leads to reduced choices for staff and those they work with.”
“I often think it is more about the financial capability. In my workplace there is a lot of strain on many services and therefore I don't imagine my workplace allowing trauma-informed training taking place as it is also not seen as a necessity to our roles/ department.”
“Time commitment to undertake training is a critical factor. Whilst the prioritisation is recognised, it is the time availability from delivering services that causes difficulties.”
“I would want to be very clear that within my organisation there is no lack of commitment or motivation to practice in a way that is trauma informed. However, the impact of the past five years on organisational, staff and community resilience has to be placed at the centre of this question. As such we are aiming to support a more vulnerable community with increasingly complex needs with a greatly diminished resource.”
A number of responses also felt that there was a cultural barrier to implementation with trauma-informed practice described as a “buzzword”. It should be noted that embedding trauma-informed practice requires a whole systems approach, rather than just training, and could reflect these concerns.
“‘Trauma informed practice’ is fast becoming a tokenistic buzzword in the social work/care sector. Much in the same way as "person centred". What does it really mean for a service to practice in a trauma informed way? Any input to improve understanding of trauma is undoubtedly worthwhile but I think we need to seek to understand trauma in a more meaningful way than simply through undertaking generic training and then claiming the service is trauma informed.”
“Sometimes it can feel like the learning is tick-box rather than genuinely intended to make changes/be included in work. Often, other well-known policies e.g. The Promise are prioritised in terms of planning/engagement, even though trauma-informed approaches are a key part of such policy areas.”
“Cynicism and complacency among some staff is a barrier to implementation. The idea that ‘What I'm doing works fine, why should I change it?’”
Respondents were also keen to compare trauma-informed approaches at an organisational and service level. In some cases, the service was far more advanced in adopting these practices, while others did note a greater commitment at an organisational level and a gap in implementation within services.
“Our service operates a fully trauma informed and person-centred approach. However, the organisation does not. It feels as if they use those words regularly including staff wellbeing but do not put that into practice at senior management level.”
“The service I lead is part of a bigger organisation. I feel the service the team I lead provides has no barriers to adopting trauma informed practices. The bigger organisation may feel there are barriers because of the size and complexity of the workforce.”
“The organisation as a whole has bought into trauma informed practice but at a service delivery level it has been left to individuals to sign up to available training. This has resulted in a disparity of knowledge between those who are willing/able to make time to educate themselves and improve practice and those who are not.”
Support Required
Respondents were then asked about additional support they or their organisation would need to help overcome barriers and better implement trauma informed practice. Several themes emerged from responses.
One of the most common requests was an ask for more training, particularly training at a more advanced level. Many respondents also noted that they were not aware of the training options available to them and that a comprehensive list of options would be useful. Others suggested that more awareness raising for all staff, rather than training, was needed so that everyone could understand the concept of trauma informed practice and how it related to their work.
“There needs to be more focus on bringing this to services such as ours [social care and social work]. I don't feel there is the same impetus in our services and certainly not the same opportunities for training.”
“A higher level of understanding at all levels of how trauma affects individuals within the workplace”.
“Wider availability of training / awareness raising sessions appropriate to job role”.
“Although there are pockets of excellent practice, I think there is generally a lack of awareness across the organisation as a whole. I also think there is resistance to costs/hours lost for training. I have suggested lots of times departments that I think should get at least a high-level trauma informed training course but to my knowledge there hasn't been uptake.”
Some also suggested that trauma-informed training should be mandatory or built into existing induction or other training resources. There was a recognition that this would require dedicated time allocated so that staff had time to take part in this training and reflect on how to put these lessons into practice.
“Introduction of a mandatory module in the induction programme for new staff.”
“Trauma informed training needs to be compulsory for all with annual top up and it needs to be considered by all departments including business support, finance, back of house not just front of house - and even they need it made compulsory.”
“Regular, protected time to think about how we, as a service, adopt a trauma informed approach. Time to reflect on examples of good trauma informed practice. Time to consider how we can continue to improve our trauma informed practice. Trauma informed at point of contact would require protected time for primary care/emergency service colleagues to upskill.”
Linked to this was a further ask for training on how to bridge the gap between the theory and implementation of trauma-informed approaches in practice.
“Support or guidelines on how to implement these and what it actually looks like when successfully implemented.”
“Talk needs to translate into action and this needs to be applied across the whole of the organisation, recognising that all staff have a role to play and need to develop their knowledge in this area.”
“Guidance on how to embed this into strategic frameworks and how to begin conversations about trauma-informed practice with your team and colleagues.”
Many respondents also highlighted the need for more resources to free up staff time and reduce caseloads to undertake training and put this into practice.
“Staff require a more manageable caseload in order to provide the trauma informed practice that they strive to deliver”.
“We are working in challenging times with completing priorities. We need to have a full and settled staffing complement to embed a trauma informed approach.”
Respondents also discussed the methods in which training is made available. While there was an ask for more online training, there were many respondents who felt that face-to-face training delivered locally with a more in-depth approach would be valuable.
“One-off in line training is not enough, and frankly what I have had to do has not been good quality. Online modules are not enough, and there needs to be follow up, reflection, a chance for "supervision" in the sense that counsellors get supervision i.e. non- judgemental, accepting, safe, empathetic support from a qualified person. “
“Proper in-depth training other than just a short overview via teams. Also, any training we have had is around recognising the impact of trauma however not on any interventions which can help a child or young person who has suffered trauma.”
“Face to face training rather than e-learning modules or virtual delivery of training. People learn more from face-to-face interaction and opens more opportunity for discussion and support if an individual is struggling (re-traumatised)”
Another area of support identified was audit or evaluation of practices to identify whether training had led to the implementation of more trauma-informed practice, with goals to work towards. Respondents also asked for sharing of good practice and mentoring from areas or teams where there had been successful implementation.
“Workbook with step-by-step guide to create a trauma-informed organisation. I am aware there are the training guides and the framework. I am meaning something like a bronze, silver, gold level chartership where we have specific goals to work towards and evidence to show the organisation has met the targets”.
“Increase awareness of resources available and provide real case study examples showing trauma informed good practice. have them relate to the activities of a local authority.”
“Maybe both encouraging prompts via comms and sharing examples of good practice and learning examples. Perhaps spot checks or audit tools that create a space for friendly critic/ feedback that can offer opportunities that can drive up standards and buy-in to being actively trauma aware and trauma informed.”
One of the most common themes was leadership. Many responses suggested that leaders, and particularly senior leaders, could do more to buy into this approach and embody trauma-informed ways of working. Some suggested that greater training resource should be targeted at leaders so that it could filter down through their organisation.
“Training for executive board members and chief officers to help them understand the importance of this agenda within a performing service.”
“At this stage I think we need our Leaders to show a commitment to trauma informed practice and to ensure it is embodied in the Council plans, service plans and it’s reflected in all our commitments and policies going forward utilising a trauma informed lens.”
“I think it would be helpful for all senior managers to have more understanding so that this is prioritised. There is definitely more understanding and nurture is now prioritised, but all staff need to have a good understanding so that they can work as an informed team.”
Contact
Email: ACEstrauma@gov.scot
There is a problem
Thanks for your feedback