Palliative care strategy - service mapping survey: main findings report
Our clinical advisory and working groups undertook four complementary surveys to determine how general and specialist palliative care services at a Health Board level are addressing the needs of adults, children, their families and carers. This report covers the main findings from all four surveys.
3. Key findings
Structures and Planning
- Collaborative working relationships between HSCPs and NHS Boards are varied and complex. Ways of working and reporting on general palliative care and specialist palliative care services varied by NHS Board areas and even within them. Respondents identified a pressing need for more robust arrangements for ensuring integrated working and equitable resourcing across all places of care for palliative care and care of people who are dying.
- Nominated leads for palliative care were described by most HSCP and NHS Board respondents (86% and 78% respectively). The nominated lead described was often in a clinical leadership role not an executive or managerial leadership role.
- Most HSCPs indicated that they had specific planning for palliative care within their strategic plans for 2023-24, yet detailed or specific plans for commissioning or directing care delivery for general palliative care and/ or specialist palliative care services were uncommon in published plans.
- Across the surveys, different proportions of respondents reported a Managed Care Network (MCN) or equivalent in their NHS Board area making it difficult to interpret a national picture. Respondents in several areas highlighted the need to restart an effective MCN or develop one if not in place at present.
- Partnership working was evident between NHS and third sector providers in delivering paediatric palliative care, including leadership models, case studies of good practice in community care, transitions, collaboration with adult palliative care services and bereavement support.
Adult Specialist Palliative Care Services
- Of the 38 Adult Specialist Palliative Care Services (ASPCS) responding, 56.5% described themselves as Independent or Third Sector, 41% as NHS Scotland and 2.5% as Other or Joint Funding. Three NHS Board areas reported no palliative medicine consultants in their Board area, these palliative care services linked to specialist palliative medicine consultant input in another Board area.
- ASPCS described providing specialist care to people at home, in care homes, in hospital, as outpatients and within hospices/specialist palliative care units. Care delivery included direct, collaborative, advisory specialist care as well as provision of clinical education and training. This varied across NHS Board areas in terms of resourcing, service models and provision (see Annex B for a breakdown of results by NHS Board).
- Over 11,022 Community referrals were reported by 19 ASPCS in 2021-2022. ASPCS described offering community based palliative care services in all NHS Boards. These varied in approach, operational structure and resourcing. Survey data suggests community based specialist palliative care services are predominantly led and delivered by clinical nurse specialists.
- Most NHS Board respondents described having hospital specialist palliative care teams, and these varied in team structure and resourcing. In 2021-2022, 16,765 hospital referrals were reported by 12 ASPCS with hospitals services. Fewer than half of the responding NHS Boards had in-hospital inpatient palliative care beds.
- ASPCS described having 138 whole-time equivalent (WTE) community clinical nurse specialists (2.5 per 100,000), 53 WTE hospital nurse specialists (0.98 per 100,000). Adult Specialist Palliative Care units (n=18; 245 beds) reported 244 WTE Band 5 registered nurses, 52 WTE Band 6 registered nurses and 19 senior charge nurses.
- Five NHS Board areas reported having a nurse consultant with specific responsibilities for palliative care. Lead nurse roles for palliative care or combined roles with cancer care or other specialities were also described. One professor of palliative care nursing was identified.
- ASPCS survey responses highlighted a wide range of roles provided by palliative medicine consultants. Respondents reported 0.9 WTE palliative medicine consultant per 100,000 population in 2021-2022 which includes time given to wider roles beyond palliative care service (e.g. university roles, realistic medicine). Three NHS Boards had no palliative medicine consultants in their area but linked virtually with another NHS Board to access Palliative Medicine support.[4]
- Less than half of ASPCS described funding or time allocated for social work, lymphoedema and clinical psychology. Services described access to these through working with other services or as gaps.
- Gaps in resourced time for pharmacy, occupational therapy and physiotherapy were also highlighted in the ASPCS survey.
- 245 inpatient specialist palliative care beds were reported, representing 4.5 specialist inpatient beds per 100,000 of the Scottish population. Three NHS Board areas had inpatient beds that were not supported by a palliative medicine consultant on-site. Ten NHS Board areas reported offering a palliative care outpatient clinic. In 2021-2022, 3,795 new admissions to a hospice or adult specialist palliative care unit were reported.
- Of 22 HSCP respondents, 13 reported access to out of hours specialist palliative care telephone advice to support care of patients in all settings (community including care homes, community hospitals and acute hospitals). In NHS Board areas, 8 (57%) described a direct public phone line for palliative care advice or access to services (see Annex C for a breakdown of results by NHS Board).
Babies, Children and Young People
- There were 359 referrals to Paediatric Palliative Care services in 2022-2023, and three services reported 80% of these referrals.[5]
- The number of young adults transitioning from paediatric services was small (28 in 2022-2023)[6], but numbers are under-reported, increasing and cases complex. Only third sector services have dedicated transition teams. Partnership between third sector partners offers a transitions pathway in four NHS Board areas.

- Few ASPCS provided data on transition from paediatric to adult palliative care. The reported number of young adults admitted to adult palliative care units was small (23 in 2021-2022, 0.6% of admissions), but respondents noted partnership working approaches to transitions of care with other services and as outpatients. One adult specialist service reported the majority of the data and had a majority of the admissions.
- The majority of specialist paediatric palliative care staff were funded by the third sector to deliver many services, particularly in the community, as well as bereavement support and transitions to adult services.
Palliative Care Data
- Most HSCP respondents (73%) reported using service management data available to all HSCPs via the Public Health Scotland confidential dashboards. However, few described information systems that allowed them to understand population palliative care needs or make sure activities to address identified needs were in place or effective.
- Few HSCPs (5) and NHS Boards (2) reported any dedicated resource for managing, reporting or collecting data on palliative care or care around dying. Some areas had difficulty accessing outcome data or had issues with time-consuming data gathering and/or analyses, while others used data extensively.
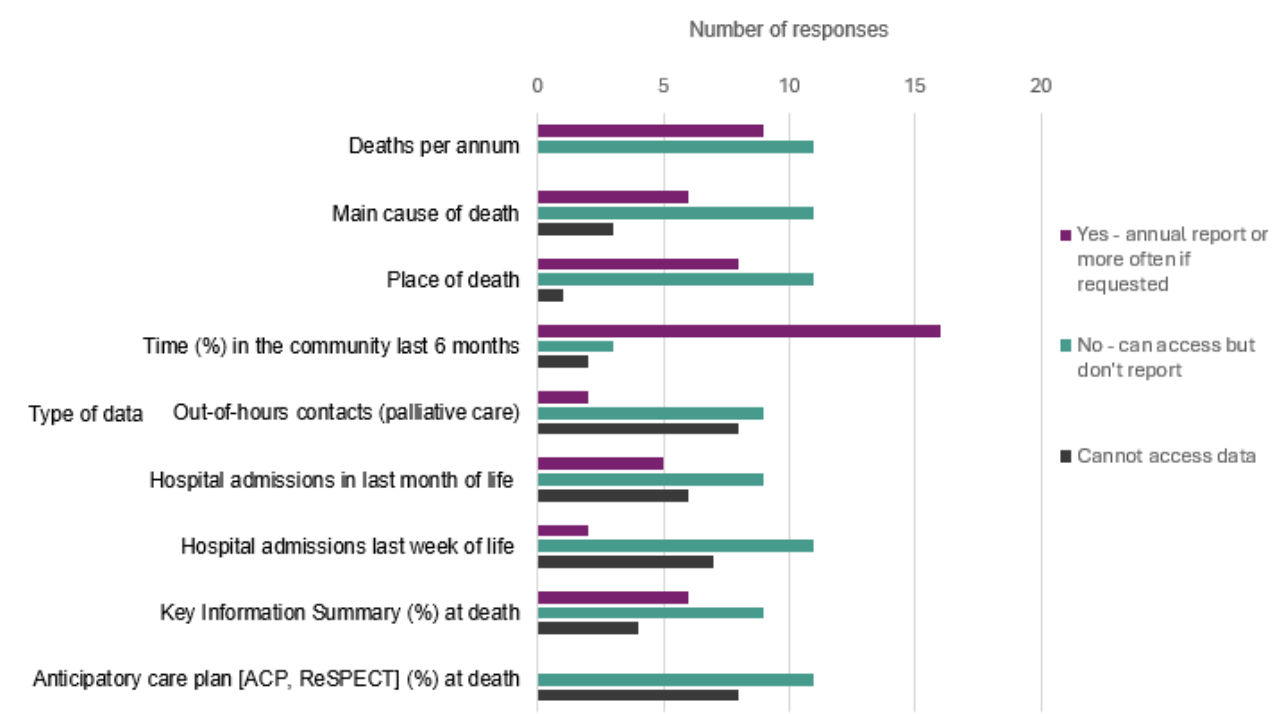
- The percentage of time spent in the community in the last 6 months of life was the most common data item reported by HSCPs (see Figure 2). There were some examples of population assessment and service utilisation data, but most HSCPs and NHS Boards indicated that they do not report data such as causes of death, location of death, place of care in the last week of life, or illness profiles related to palliative care.
- Data related to experience of illness and care was highlighted as challenging to access, with specific challenges related to care around dying and being limited by selection bias. The majority of HSCPs and NHS Boards described complaints as the main source of experience feedback, followed by Care Opinion and then by service satisfaction surveys. Few described public engagement groups or public consultations.
- Data challenges were identified clearly by ASPCS regarding collation, access, resourcing, sharing to and from other partner organisations, national returns of data and complexities of data. Completion of these mapping surveys was challenging for some services in terms of accessing data and staff time needed.
- Data challenges were recognised by paediatric palliative care services regarding sharing between different organisations, definitions, complexities and under-reporting. There was overlap and duplication identified in paediatric data submitted for the mapping survey. Distinct differences between size of population, data and context for paediatric palliative care from adult palliative care were described alongside areas of commonality.
Identification and Assessment
- A variety of tools were being used to identify patients with palliative care needs across Scotland ranging from 1-6 tools in individual Health and Social Care Partnerships. A few used a recommended carer assessment tool.
- In ASPCS, tools most reported were the Palliative Performance Scale, Integrated Palliative Outcome Scale, Phase of Illness and Modified Karnofsky Performance Status. Comments described limits of the tools, as well as examples of their use being integrated into services and the importance of distinguishing identification of people who may have palliative care needs from subsequent individual assessment of needs and assets.
- Few NHS Boards (2) and HSCPs (5) reported using any specific ways to identify, assess and address the palliative care needs of people from minority ethnic groups or those with protected characteristics. Some noted they are developing these resources.
Referrals
- For ASPCS, reported referrals of people with cancer or a non-cancer illness varied by place of care. Admissions of people with non-cancer illnesses to hospices/specialist palliative care units outside of acute settings averaged 10.2% (range 3-20%), and community, day care and outpatient referrals averaged 12.8% (range 0-60%); with daycare services more likely to report higher numbers of referrals for people who did not have cancer. Referrals for people with non-cancer illnesses were highest in hospital settings, averaging 38.3% (range 2-63% with one hospital being a cancer hospital).
- There was large variation in referral patterns and referral routes in paediatric palliative care. Respondents mentioned the third sector as an important referral partner.
Future Care Planning
- Future care planning recorded using a Recommended Summary Plan for Emergency Care and Treatment (ReSPECT) plan and/or Treatment Escalation Plan was reported to be used by staff in hospitals but respondents noted that it has not been implemented across all clinical areas. Having a consistent digital solution across settings and boundaries was highlighted as a key enabler for future care planning.
- HSCPs provided examples of future care planning incorporated into online palliative care training and future planning information being available online or via partners to the public.
- A national conversation on future care plans, forums to share good practice, a Scotland-wide Future Care Plan and resources for future care planning were raised as areas for development.
Care Homes
- The number of care home beds designated for provision of palliative care and care around dying varied across NHS Boards, as did the total number of care home beds. Some areas reported that palliative care is accessible to all residents and other areas described specific models and beds for enhanced palliative care or care around dying.
- Care home staff sought support regarding palliative care and care around dying most commonly through primary care services, both in hours and out of hours.
- Less than 50% of ASPCS across NHS Boards described specific and direct arrangements for supporting care homes in 2021-22. However, the majority of services described linking with primary care teams and wider community teams to provide support. Few ASPCS were able to provide data specific to residents of care homes.
Getting support
- ASPCS recognised that most of the compassionate community[7] aspects of public health palliative care are located best within communities themselves. ASPCS also gave examples of supporting and working in partnership as members of compassionate community partnerships (see ‘Innovations and Opportunities’ below).
- Carers support, such as carer centres, bereavement groups and cafes, respite services and carers support groups, were described by NHS Boards and an area of innovation in some areas.
- Paediatric services noted that arrangements differed greatly for bereavement care across the country and could also differ within localities. There could be multiple providers involved and a reliance on third sector partners. Few HSCPs described leads for bereavement or strategic planning specific to bereavement.
- ASPCS reported varied but high-level support from unpaid volunteers. Data was limited, but nearly 14,000 days of volunteer work was described by 10 responding services. A range of volunteer activity was described including practical care, driving, counselling, listening services, fundraising and befriending.
- Less than 50% of ASPCS described funded or allocated time for spiritual care practitioners, with most linking to wider spiritual care services within the NHS. Opportunities to link with the Spiritual Care Framework were highlighted.
Education, Training and Resourcing
- Only one NHS Board area reported use of the Scottish Government Guideline “Caring for people in the last few days and hours of life” to support care around death in hospitals, although five NHS Boards said they provide specific training in palliative care for non-specialist hospital staff giving care in the last few days and hours of life.
- Online training on palliative care was reported as widely accessible to staff delivering general palliative care in the surveys, but there was variability of access across NHS Board areas for training available during work hours and training focused on bereavement.
- From the paediatric palliative care survey, there was a reported lack of clear training pathways for specialists in paediatric palliative care and varied support for other staff delivering paediatric palliative care at different levels of expertise within many areas. Respondents noted that paediatric staff often support paediatric palliative care delivery without recognition, support or training.
- ASPCS based in half of the NHS Boards reported having an adult specialist palliative care education practitioner as part of their service. Services utilised a wide range of approaches to education across different settings and online, and reported being limited by lack of resources to meet education and training needs across the health and social care system that they saw as needed.
- Financial and human resourcing challenges were identified by adult and paediatric specialist palliative care service respondents. Concerns were raised that services are not sustainable, they cannot extend or develop their services to meet population needs, or have limited staff succession planning. There were also concerns raised of being unable to meet demands for education and training provision for other services and for the public.
Innovation and Opportunities
- Respondents indicated a wide range of innovations and opportunities in palliative care, see examples below.
- A patient passport for relevant stakeholders to access care information, improved IT systems, a national approach to future care planning and better access to community nursing 24/7 were suggested as ‘Once for Scotland’ approaches.
- NHS Boards and HSCPs noted that the new palliative care strategy presents an opportunity for a common framework, better training, equity of care and knowledge sharing across areas.
Examples of innovations and opportunities described or suggested:
Public
24/7 Public access telephone line for palliative care advice and services
Compassionate Communities and other community based networks
‘No one dies alone’ work
More public engagement around experience of palliative care
Local memorial book for early miscarriage
Person/Patient held Future Care Plan
Scotland-wide Children and Young People’s future care plan
Medicines and equipment supporting palliative care
Care homes holding stock of palliative care medications to facilitate timely access
Medicine prescribing charts for palliative care that work across secondary and primary care
National Syringe Pump Policy for use and supply
Rapid provision of hospital beds at home for care around dying
Services
‘Front door’ palliative care (providing support at front door in order to reduce admissions to acute beds, reduce bed days and provide better end of life care)
‘Call before you convey' (collaboration between ambulance service and the NHS whereby patient care is discussed with appropriate professionals to achieve right care, right place, right time)
Integrated single point of access to general and specialist palliative care for professionals
National Cancer Pain Interventional Service
Pharmacy led, nurse led outpatient clinics
Rapid social care provision for care around death
7 day service delivery for specialist palliative care services in all settings
Review resource workforce for palliative care
National on call model for paediatric palliative care
Embedding telemedicine across health boards for adult and paediatric palliative care
Outpatient services at children’s hospices
Neonatal to paediatric care pathways described and resourced
Hospice care at home
Rapid provision of hospital beds at home to support those dying at home
Palliative Care beds in Care Home setting with supporting staff models
Acute Palliative Care expanded multi-disciplinary team models
Education, Training and Research
National Education Platform for Palliative Care
Online Training Expansion e.g. Project ECHO
Dedicated Health and Social Care Partnership Education Practitioners for Palliative Care
Public education resources e.g. End of Life Aide Skills for Everyone (EASE) and Last Aid
Integrated research teams and portfolios
Scotland-based training for Community Children’s Nurses
Bereavement training for generalist staff (adult and paediatric)
Scotland based training for Community Children’s Nurses
SAS Project on Transitions of Care Models
Contact
Email: Palliativecareteam@gov.scot
There is a problem
Thanks for your feedback