Quality prescribing for antidepressants: guide for improvement 2024 to 2027
Antidepressant prescribing continues to increase in Scotland with one in five adults receiving one or more antidepressant prescriptions in a year. This guide aims to further improve the care of individuals receiving antidepressant medication and promote a holistic approach to person-centred care.
2. Recommendations and guidance for healthcare professionals
Healthcare professionals should:
Consider non-medicalised and non-pharmacological options where appropriate
Non-medicalised and psychosocial [65],[66],[67]
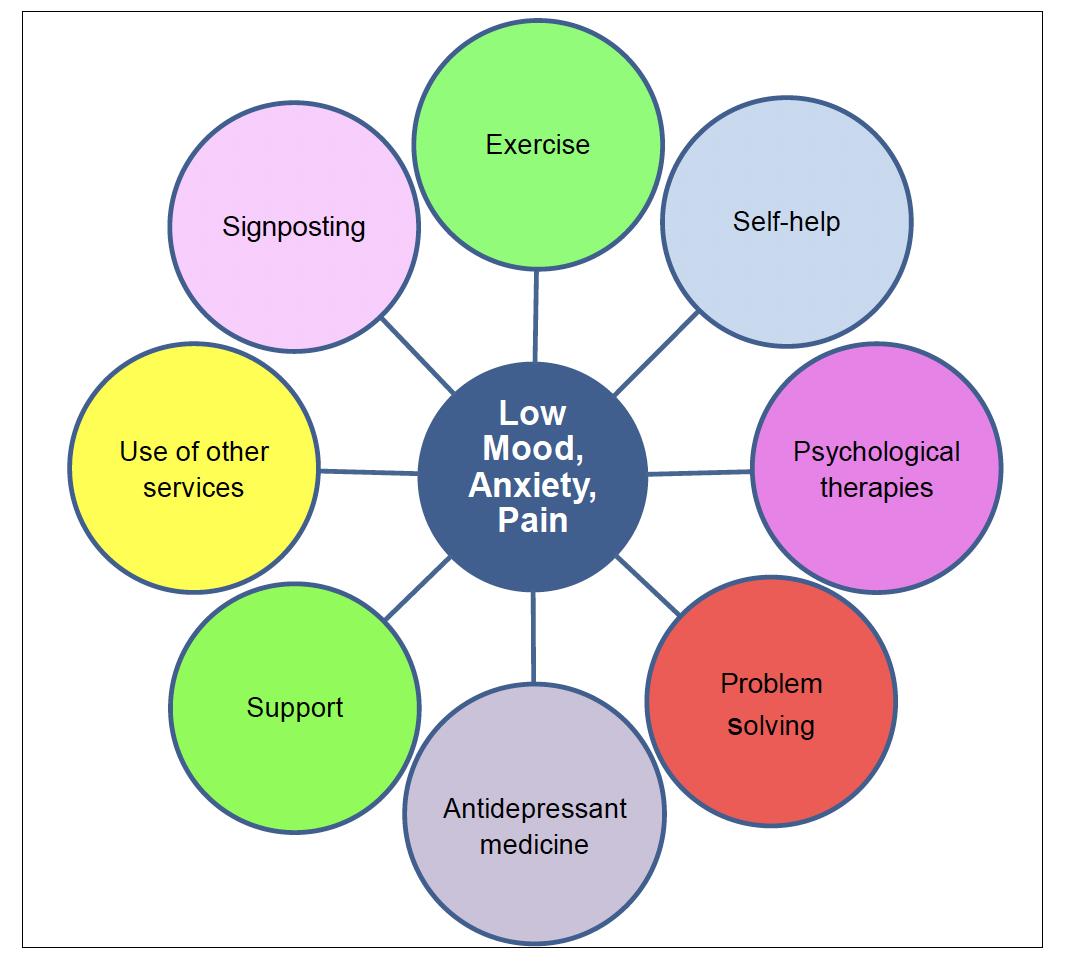
While a range of activities may help with common mental health problems and pain management, these will vary with individuals’ preferences, capabilities, and locality. Some of the following may be appropriate and should be considered and discussed before initiating an antidepressant, as well as when continuing an antidepressant for more severe illness. Where appropriate and available, a Community Link Worker may be able to support and enable individuals to access or develop some of the options below.
- exercise and regular physical activity e.g. 30-minute walks
- debt advice and/or money management e.g. seeking advice from appropriate agencies such as Citizens Advice
- hobbies and interests e.g. gardening, crafts, etc.
- ensuring a healthy work-life balance
- lunch clubs and other activities which help to reduce social isolation
- discussing problems, where appropriate, with a close friend or confidante that is willing and able to listen
Psychosocial and psychological Interventions
The Psychological Therapies Matrix (2015) outlines a matched care approach to support the safe and effective delivery of evidence based psychological interventions. Both the Matrix and clinical guidelines advocate decisions regarding psychological interventions based on a comprehensive assessment of need and suitability, individual preferences, availability of trained practitioners and cultural appropriateness.36,37 This matched care model considers ‘high volume’, low intensity interventions for mild to moderate symptoms, in addition to high intensity and highly specialist interventions delivered by practitioners with additional competences, for those presenting with more complex presentations. The Matrix acknowledges those in primary care who regularly identify and support those presenting with psychological issues and mental health disorders. They are often able to provide support for low intensity interventions and referral to specialist mental health services where indicated.
Low intensity interventions
For mild to moderate symptoms of depression and/or anxiety these include guided self-help and computerised cognitive behavioural therapy (cCBT). Psychoeducation can support self-management. A range of evidence based cCBT programmes and telephone supports are available to support general mental wellbeing, sleep problems (including insomnia) and mild to moderate symptoms of depression. Links to these programmes can be accessed via NHS Inform (Mental Health). Please refer to Appendix 1 and 2 for a detailed description and links to these resources.
High intensity and highly specialist interventions
For those individuals who present with moderate to severe symptoms of depression and/or anxiety, a referral for High Intensity and/or Highly Specialist Interventions may be indicated and may include CBT. These interventions are usually delivered within NHS or non-NHS specialist services. (Note: non-NHS services: ensure non-NHS practitioners providing psychological therapies are registered with appropriate professional bodies e.g. Health and Care Professions Council, British Association of Behavioural and Cognitive Psychotherapy, British Association of Counselling and Psychotherapy.)
Follow a person-centred approach to initiating antidepressants
A holistic assessment that includes assessment of severity of symptoms and discussion of the risks, benefits and limitations of prescribing, should inform decisions to initiate antidepressants, considering the psychological components of care. This can be done using the 7-Steps medication review process.
- Consider comorbidities prior to initiating an antidepressant as part of the biopsychosocial assessment and the potential for interactions with other medicines and diseases e.g. QTc prolongation, etc.
- Depression:
- The stepped-care approach should be used to help choose the most appropriate intervention - self-help, non-pharmacological, with or without antidepressant therapy.[36]
- Consider that for 50% of individuals depressive symptoms can spontaneously resolve within 12 weeks of diagnosis.[68]
- Less severe depression (i.e. PHQ-9 score <16) commonly referred to as mild depression, may respond better to non-pharmacological approaches as antidepressants are not effective for less severe illness.[20],[36]
- ‘Do not routinely offer antidepressant medication as first-line treatment for less severe depression, unless that is the person's preference’.
- Moderate to severe depression. Antidepressants are effective for reducing symptoms of moderate to severe depression and/or helping people achieve remission, especially in combination with non-pharmacological treatment and/or self-help, see Figure 5 and Table 2.[20],[36]
- Anxiety disorders:
- The stepped-care approach should be used to help choose the most appropriate intervention; self-help, non-pharmacological with or without antidepressants,[37],[38] in supporting individuals to achieve a reduction in anxiety symptoms and/or achieve remission, see Figure 5.
- Different antidepressants demonstrate variable efficacy depending on which anxiety disorder is being treated – generalized anxiety disorder (GAD), panic disorder, obsessive compulsive disorder (OCD), etc.[37], [69]
- Pain:
- Neuropathic pain. Tricyclic antidepressants (TCAs) and duloxetine demonstrate modest effects for the treatment of neuropathic pain (Table 2).[33]
- Low back pain and sciatica. NICE indicates that ‘there was no evidence on the use of antidepressants for sciatica. The committee agreed that antidepressants were commonly prescribed for sciatica, and clinical experience suggests they may be of benefit in some people. The committee considered the potential for harm to be less than the harms of prolonged use of opioids.’[70]
- Chronic pain. The evidence for use of antidepressants (amitriptyline, citalopram, duloxetine, fluoxetine, paroxetine and sertraline) in chronic pain is conflicting. Antidepressants improved quality of life, pain, sleep and psychological distress compared with placebo.[71],[72]
Discuss:
- individual and prescriber’s expectations
- stepped-care and watchful-waiting for common mental health conditions
- effective non-pharmacological interventions (e.g. physical activity, self-help)
- drug effects and limitations (e.g. dose response) including dose ranges for treatment of different conditions (e.g. SSRI flat dose response effects for depression: meaning that ‘20’s plenty and 50’s enough’ – using standard doses of 20mg daily of citalopram/fluoxetine/paroxetine or 50mg daily of sertraline – to provide the full antidepressant effect,[40]-[42],[44] or for neuropathic pain response TCAs at doses ≤75mg per day)[33]
- the potential for short and long-term adverse drug effects e.g. nausea, agitation, sedation, sexual dysfunction. It is also important to discuss and consider how and when the antidepressant will be reduced and stopped in the future to minimise potential drug-related harms
Provide appropriate information about the condition (NHS Inform website), antidepressant treatment and stopping. The Choice and Medications website contains a variety of information and leaflets which may be helpful.
Plan and agree follow up in relation to the condition being treated
In depression, it is a widely held belief that antidepressants do not exert their effects for four to six weeks. However, all antidepressants show a pattern of response and rate of improvement which is greater in the first one to two weeks.[18],[20], [73] Therefore, for those with no response at three to four weeks, review diagnosis; adherence with treatment; and where appropriate consider switching to an alternative antidepressant. Studies demonstrate that prescribers may change the antidepressant or optimise the dose at eight weeks, which creates a lag in treatment and may slow recovery.[5],[21] Where appropriate, communicate changes in prescribing to the individual’s specialist in secondary care.
Agree, plan and record the criteria for reducing and stopping the antidepressant in the future, or if adverse drug effects become intolerable e.g. severe restlessness, more frequent thoughts of suicide or deliberate self-harm. Although younger people less than 25 years old are considered at greatest risk of antidepressant associated self-harm, there are multiple age, gender and regional effects that are associated with self-harm and suicide,[74],[75] therefore these should also be explored.
Encourage people that are prescribed antidepressants, or any other medicine, to initiate open discussions regarding the appropriate continuation, reduction and discontinuation of pharmacological treatment.
Review effectiveness, tolerability and adherence on an ongoing basis as part of a medication review, and where appropriate reduce the number and doses of medicines to minimise avoidable adverse effects and harms and to optimise adherence. Consider inviting individuals for proactive medication reviews. See Appendix 3 for an example review invite letter.
In relation to mental health and emotional distress, where appropriate complete and record a biopsychosocial assessment including:
- asking individuals directly about thoughts and/or plans of self-harm or suicide, and record severity as outlined in appropriate guidelines.[37],[76]
- consider and exclude physical causes of signs and symptoms including:
- alcohol (FAST tool)
- problem substance use
- bereavement
- organic disease as a cause for symptoms
As depression and other mental health conditions are associated with an increased risk of deliberate self-harm and suicide, ask the individual directly about any thoughts or plans for self-harm or suicide. Although some individuals may have suicidal thoughts when visiting their health professional, they may withhold and not share their thoughts.[11], [77] Where healthcare professionals are uncomfortable asking directly about self-harm or suicide, the PHQ-9 assessment tool includes a self-harm question that may help facilitate and enable further discussion around this. As outlined in guidelines, such as the NICE depression guidelines, antidepressants may be appropriate in treating depression as part of the stepped-care model for the treatment of moderate to severe depression.36 Continue to use and record the results of valid assessment tools such as PHQ-9, CORE 10 or other suitable rating scales to support continuity of care.
Develop a clear management plan collaboratively with the individual and carers where appropriate
Prescribers and individuals should aim to develop mutually supportive and constructive discussions when reviewing antidepressants and ongoing treatment needs. Where appropriate consider the fears and apprehensions associated with reducing/stopping antidepressant therapy and tailor treatment to the individual’s needs.
The stepped-care approach should be used to tailor the most appropriate intervention to the individual’s needs. This can be done according to the severity of the condition being treated, such as self-help resources or non-pharmacological interventions with or without antidepressant therapy.[36],[37]
Include realistic expectations and review dates that can be read coded for recall and pre-planned follow-up.
Indication |
Antidepressant |
NNT |
NNH |
Reference |
|---|---|---|---|---|
Depression |
Antidepressants |
5 to 7* |
- |
Cleare et al 2015[20] |
Depression |
TCA |
8.5* |
- |
Arroll et al 2016[78] |
Depression |
SSRI |
6.5* |
- |
|
Depression |
TCA |
4* |
4 to 30† |
Arroll et al 2009[79] |
Depression |
SSRI |
6* |
20 to 90† |
|
Neuropathic pain |
TCA |
4+ |
13† |
Finnerup et al 2015[33] |
Neuropathic pain |
SNRI |
6+ |
12† |
|
OCD |
SSRI |
6 to 12± |
- |
Soomro et al 2008[80] |
Bipolar depression |
Antidepressants |
4* |
- |
Leucht et al 2012[81] |
* Response: usually defined as a ≥50% reduction in depression rating scale scores or remission.
† Withdrawal from study due to adverse drug effects
+ ≥50% reduction in pain intensity scores
± ≥25% reduction in Yale Brown Obsessive Compulsive Scale
Common adverse drug effects/harms from antidepressants
Antidepressants are associated with a variety of adverse drug effects. Short-term effects can include symptoms such as nausea, with long-term effects including weight gain, weight loss or cognitive effects. Other short- or long-term drug effects include sexual dysfunction, insomnia, sedation, anxiety, falls, fatigue, gastric bleeding, hyponatraemia and QTc prolongation.[82] People may experience weight changes during antidepressant treatment. Weight gain may be associated with depression recovery and improved appetite on one hand and undesirable antidepressant effects on the other; [83] however, many placebo controlled studies report no weight data making it difficult to accurately estimate weight changes.[82] SSRIs have been seen as weight neutral, or in some cases associated with weight loss in the short-term (≤8wk studies) and weight gain in the long-term.[83],[49], [84], [85]
Ensure individuals are assessed and read coded for the condition being treated
Only a minority of individuals have a clear electronically recorded (read code) indication for receiving an antidepressant.[7] Although the indication for the antidepressant can be identified from free-text entries in electronic and paper clinical notes, these are not easily identified unless an individual’s clinical record is accessed and specifically searched for.[7] Therefore, appropriately coding of individuals’ records would support easier identification for proactive medication reviews in general practice and specialist services, as prescribers have indicated that:
‘...patients can get lost in the system, and that systems which adequately prompt medication reviews would be useful in broaching discontinuation with patients.’[14]
Healthcare practitioners and clinical teams should ensure individuals are appropriately coded in their electronic clinical systems:
- Depression (code E2B), anxiety with depression (E2003), bipolar affective disorder (Eu32), etc.
- Anxiety disorder such as generalised anxiety disorder (GAD, E2002), post-traumatic stress disorder (PTSD, Eu431), etc.
- Chronic pain (1M52), neuropathic pain (N2423), diabetic neuropathic pain (1M8) and chronic pain review recorded as 66n when a review is undertaken.
- For a polypharmacy review, if reviewing existing treatment prior to initiation of antidepressant medicines, use read code 8B31B Polypharmacy medication review.
- Where the condition has resolved and the antidepressant has been stopped, please use the appropriate read code e.g. depression resolved (212S), anxiety resolved (2126J). (Other read codes for resolution of symptoms are not currently available on general practice systems.)
Boards and HSCPs should:
Consider the prescribing advice within this guidance alongside local prescribing and clinical data to plan, resource and drive quality improvement and prescribing initiatives.
Nominate local leads/champions – one medical and one within or with strong links to medicines management teams, or equivalent, to drive delivery and recommendations within this guidance.
Consider and engage a whole system approach to delivering quality improvements in prescribing
- Ensure primary and secondary care are informed to support continuity of care and overall goals of reviewing and minimising inappropriate prescribing, especially given the significant influence of secondary care.
- Work with third sector (non-medicalised) organisations to further develop support and capacity for self-management.
Hospitals and specialist outpatient clinics should:
Secondary care specialists should ensure that prescribing records reconcile with the individual's current prescription and review what medicines they are taking. It is known that prescribing discrepancies can occur between primary and secondary care records.[86],[87],[88] Where appropriate, specialists should access, check and update current prescribing information using the individual’s Emergency Care Summary.
Secondary care should establish and communicate changes in antidepressant prescriptions started in hospital, stating intended treatment duration or where a drug has been reduced or stopped, including the rationale for the prescriber’s actions.
General practice clusters:
Engage with local prescribing support teams, who have a wealth of experience improving the quality of prescribing using local and national measures, datasets and tools.
Contact
Email: EPandT@gov.scot
There is a problem
Thanks for your feedback