Quality prescribing for Benzodiazepines and z-drugs: guide for improvement 2024 to 2027
Benzodiazepine and z-drug prescribing continues to slowly reduce across Scotland. Despite this, benzodiazepine and z-drug prescribing remains a challenge. This guide aims to further improve the care of individuals receiving these medicines and promote a holistic approach to person-centred care.
Executive Summary
Benzodiazepine and z-drug (B-Z) prescribing continues to slowly reduce across Scotland. In part this is due to a range of work carried out over the years, at general practice, health and social care partnership and health board levels, as well as individuals engaging with these initiatives to enable reductions in inappropriate use and prescribing of these medicines.
Despite this reduction, benzodiazepine and z-drug prescribing remains a challenge in Scotland. Over the last 30 years prescribers have managed to reverse the significant growth that was seen in the 1970s and 80s, when more than one in ten people in the UK received a benzodiazepine.[1],[2]
It is recognised that B-Z can provide some benefits in the treatment of insomnia and some anxiety disorders in the short term, however, there is increased mortality associated with B-Z use in a range of populations and their use is associated with tolerance, dependence and avoidable medicine related harms. They are associated with an increased incidence of depressive symptoms and can have a cumulative effect when used together with other sedating medication, such as opioids or gabapentinoids, increasing the risk of medicine related harms.
While we have come a long way in addressing inappropriate use, there is still work to be done to further reduce chronic benzodiazepine and z-drug use. Therefore, this quality prescribing guide is intended to support key stakeholders and prescribers to deliver proactive person-centred medication reviews to ensure effective use of benzodiazepine and z-drugs and minimise risks associated with their use. Where appropriate, and in line with current guidance, consideration should be given to non-pharmacological and evidence-based psychological interventions, either to support treatment or as alternative treatment option [see Recommendations].
This guide has been developed by the collaborative efforts of a multidisciplinary team of clinicians, academics, experts by lived experience, patient groups and policy makers from Scottish Government and NHS Scotland, who are already delivering work around benzodiazepine and z-drug prescribing to improve outcomes for the people of Scotland. It offers practical and evidenced based recommendations to prescribers and does not override existing local and national guidelines for the treatment and management of common mental health conditions. [see Background].
This guide recommends that there is shared decision-making between individuals and prescribers when reviewing benzodiazepines or z-drug treatment using the 7-Steps review process. Where appropriate, consider the fears and apprehensions associated with reducing or stopping these medicines in order to tailor treatment plans to the needs of the individual [see Recommendations].
The 7-Steps review process provides a clear person-centred approach to the initiation of new and review of existing treatments, placing an emphasis on ‘what matters to you’? Although this guide does not cover the use of benzodiazepines in the treatment for problem substance use, the 7-Steps process should be used when reviewing treatment for harm reduction.
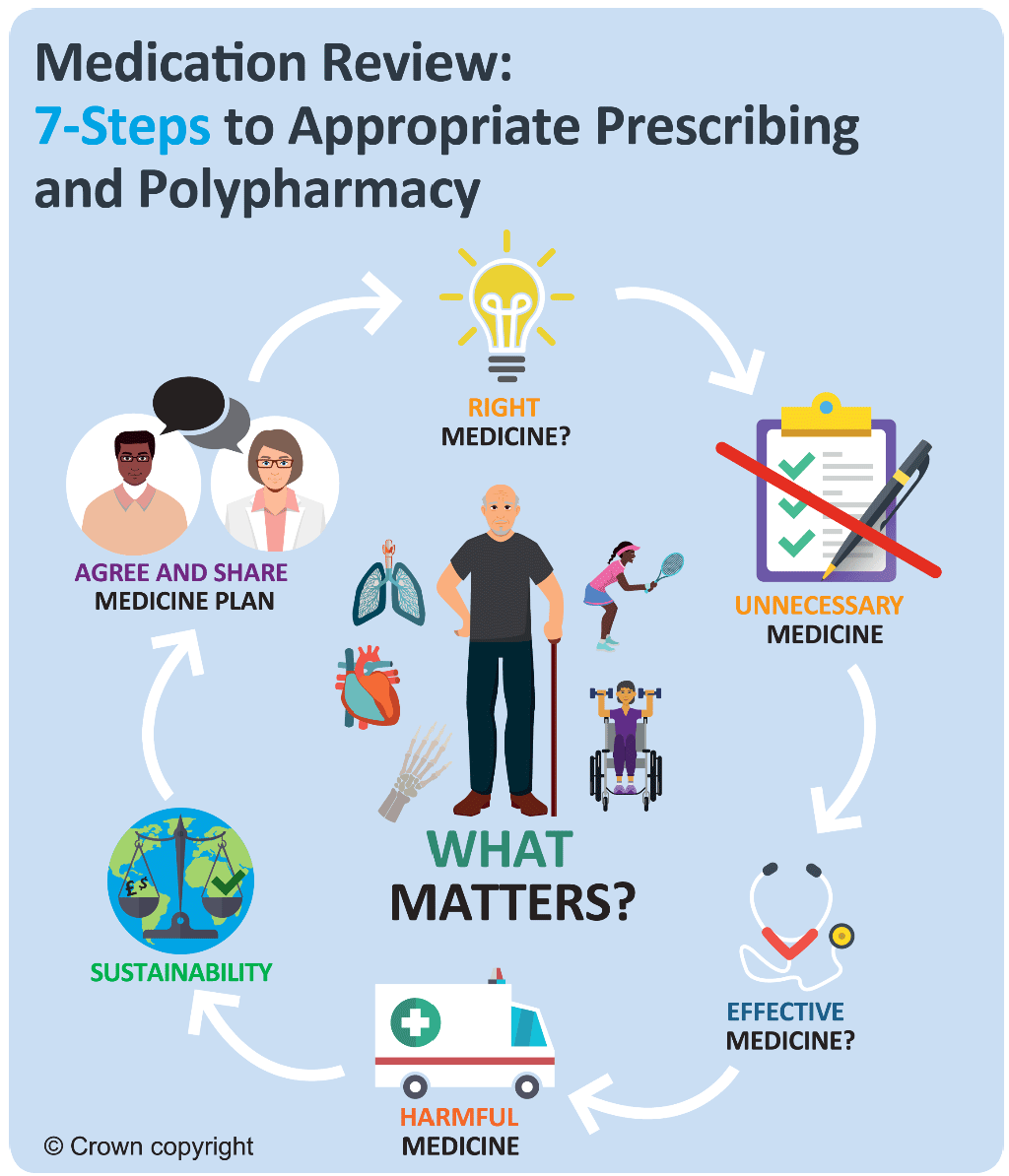
The 7-Steps review process provides a framework for this, considering:
1. Aim: what matters to the person?
2. Need: identify essential medication.
3. Need: any unnecessary medication?
4. Effectiveness: are therapeutic objectives met?
5. Safety: any ADRs/side effects or a risk of them?
6. Sustainability: cost-effective and environmentally sustainable
7. Person-centred: is the person willing and able to take drug therapy as intended?
Contact
Email: EPandT@gov.scot
There is a problem
Thanks for your feedback