Quality prescribing for Benzodiazepines and z-drugs: guide for improvement 2024 to 2027
Benzodiazepine and z-drug prescribing continues to slowly reduce across Scotland. Despite this, benzodiazepine and z-drug prescribing remains a challenge. This guide aims to further improve the care of individuals receiving these medicines and promote a holistic approach to person-centred care.
5. Reducing and stopping
This should be done in partnership with the individual.
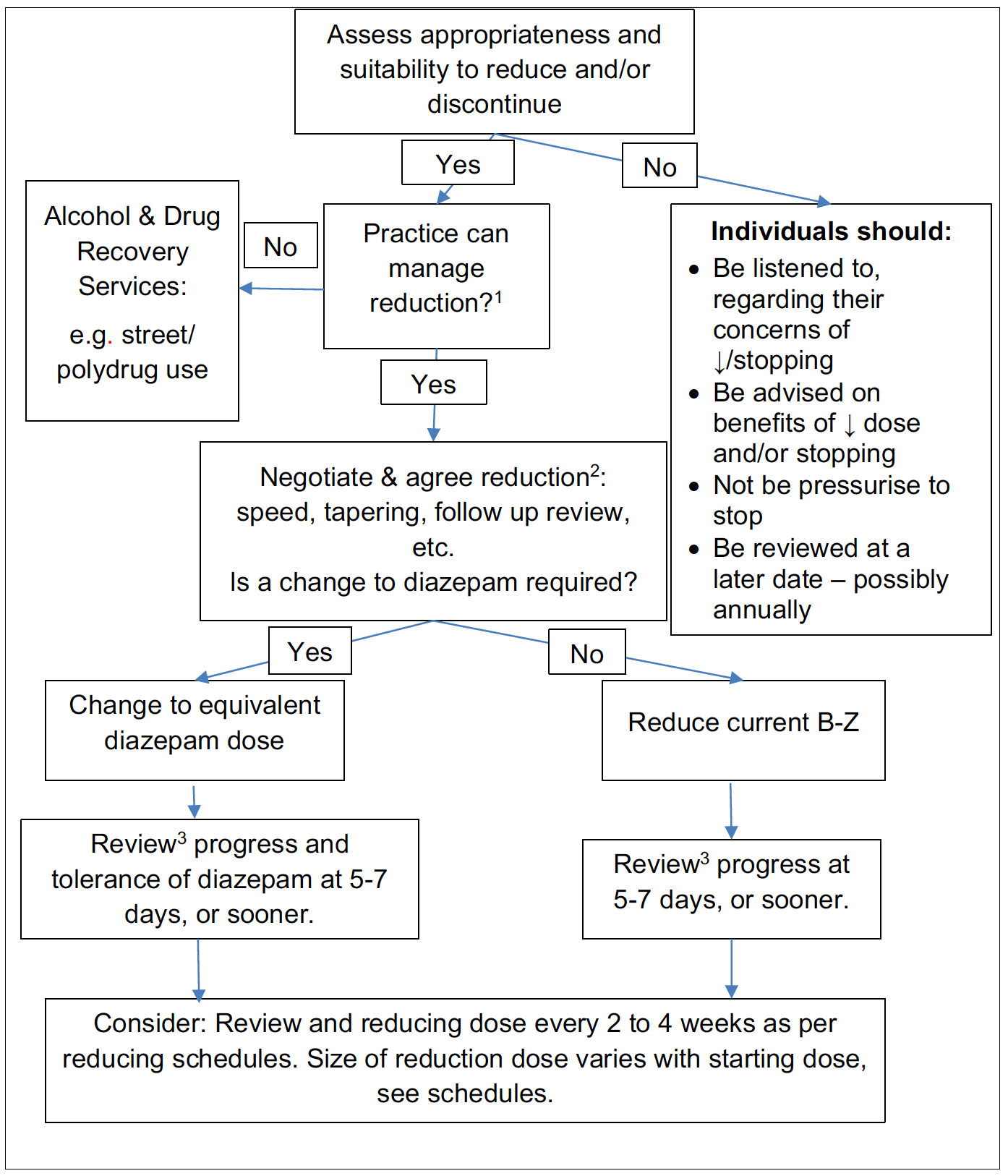
Graphic text below:
Assess the individual’s readiness to reduce and/or stop.
When an individual is not ready, they should be listened to about their concerns about reducing and stopping, be advised about the benefits of reducing and stopping but not pressurised to do so, and reviewed at a later date, possibly annually.
If they are ready, consider whether the practice can manage the reduction, or whether to signpost or refer to alcohol and drug recovery services.
Where the practice can manage the reduction, a gradual drug withdrawal schedule (dose tapering) that is flexible should be negotiated. The individual reducing/stopping treatment should guide adjustments so that they remain comfortable with the withdrawal.
If a change to diazepam is required, change to the equivalent diazepam dose and review progress and tolerance of diazepam at five to seven days, or sooner.
If no change to diazepam is required, reduce the current B-Z and review progress and tolerance of diazepam at five to seven days, or sooner.
In both scenarios, consider reviewing and reducing dose every two to four weeks as per reducing schedules. The size of reduction dose varies with the starting dose, [see schedules].
1. From previous work, general practices should be able to manage the reduction of prescribed B-Z for the majority of their practice population, see Section 6 case studies.34,37
2. A gradual drug withdrawal schedule (dose tapering) that is flexible should be negotiated. The individual reducing/stopping treatment should guide adjustments so that they remain comfortable with the withdrawal.
3. Reviews should be frequent to detect and manage problems early and to provide advice and encouragement during and after the drug withdrawal. If a person is not successful on their first attempt, they should be encouraged to try again.
The following narrative explains the flow chart in more detail.
Assess the individual’s readiness to reduce and/or stop
It is important that an individual’s motivation and readiness for reductions and/or discontinuation is adequately assessed, and where appropriate agreed and tailored dose reductions are planned, and where implemented, regularly reviewed. Signposting or referral for interventions to support changes to prescribing, including psychosocial and/or psychological interventions, should also be considered.
What is the risk-benefit balance of continuing current B-Z and doses?
Continuing to prescribe beyond four weeks is unlicensed. The risk of falls for older adults, or negative cognitive effects for people with depression or other common mental health considerations, as well as the tolerance and loss of effect that can develop within two to four weeks in the treatment of insomnia/anxiety should be acknowledged in any risk-benefit discussions.69 Prescribers may also consider that on balance some therapies may not benefit individuals and should explain their reasons to the individual and explore other options that might be available, including their right to seek a second opinion.[83]
Has the individual completed the planned and agreed course or trial of treatment?
For example, was the B-Z initiated for short-term use and has evolved into long-term use? Has a prescriber discussed the potential harms of continuing treatment and that B-Z are only licensed for maximum of four weeks’ use, and therefore it may be appropriate to plan and agree gradual reduction in therapy?
Discontinuation/withdrawal symptoms
B-Z dependence is recognised as a major clinical problem.[84] B-Z reduction should be gradual and tapered – for some this will be ‘low and slow reductions’.69,[85] Abrupt cessation may produce confusion, toxic psychosis, convulsions or a condition resembling delirium tremors.
Withdrawal symptoms may occur within a day of stopping a short-acting B-Z such as lorazepam, which is associated with more severe withdrawal than longer acting B-Z. However, withdrawal symptoms may occur at any time up to three weeks after stopping a long-acting B-Z (see List 3 and Table 3).69
Withdrawal effects may include insomnia, anxiety, depression, cognitive impairment and can be similar to the original presentation. Some withdrawal symptoms may continue for weeks or months after stopping the medication. Most people experience infrequent, mild or no withdrawal symptoms if the withdrawal is slow and tapered to their needs. However, if individuals do experience withdrawal, consider increasing the dose back up to the previous dose without withdrawal effects and after stabilising on that dose reduce more slowly, using smaller dose reduction steps. Smaller reduction steps may require the use of liquid preparations in some cases.69,84
List 3: Clinical presentation of discontinuation/withdrawal symptoms
Acute symptoms - most commonly anxiety
- Panic attacks, agoraphobia
- Insomnia, nightmares
- Depression
- Poor memory, loss of concentration
- Tremor, sweating, palpitations
Acute symptoms - others specific to B-Z
- Perceptual distortions, depersonalisation
- Tingling and loss of sensation, formication (a feeling of ants crawling all over the skin)
- Sensory hypersensitivity
- Muscle twitches and fasciculations (flickering or writhing muscles)
- Hallucinations (visual and auditory - rare and usually with rapid withdrawal from high doses)
- Psychotic symptoms, confusion, convulsions (rare and usually with rapid withdrawal from high doses)
Protracted symptoms - may affect up to 15% of people
- Anxiety - gradually recedes over a year
- Depression - may be a few months
- Insomnia - gradually recedes over 6-12 months
- Sensory symptoms - gradually recedes but may be a year and occasionally several years
- Motor symptoms - gradually recedes but may be a year and occasionally several years
- Poor memory and cognition - gradually recedes but may be a year and occasionally several years
- GI symptoms - gradually recedes but may be a year and occasionally several years
Adapted from the Ashton Manual and Maudsley Prescribing guidelines.84
Switching to diazepam
Diazepam is a longer acting B-Z. If alternative benzodiazepines are being taken, converting to the equivalent diazepam dose allows for smaller dose reductions steps, due to the range of licensed preparations available. Diazepam’s longer acting effects are less likely to be associated with withdrawal effects; especially for people receiving short acting B-Z and/or experiencing high levels of dependency.68,69,[86] Therefore this is the preferred method for gradual reduction.
Some individuals however may want to reduce by continuing their current B-Z. While this may be possible with nitrazepam and temazepam, due to a range of licensed preparations being available, it may be more challenging with other B-Z due to the range of tablet doses available. As a result the size of the dose reduction steps may be large - increasing the potential risk of withdrawal effects. Where individuals decide to reduce using their current B-Z, the risk-benefits should be discussed and closer follow up may be required.
Approximate dose equivalents and switching considerations:
- Due to individual variability and differing half-lives (Table 2) this means that these are approximate dose equivalents, not exact equivalence.
- Variability between individuals may be due to a range of effects e.g. liver impairment reducing/slowing drug excretion, which can increase B-Z half-lives and increase the risk of accumulation and drug effects.
- Dose equivalents can never be exact and should be interpreted considering your clinical knowledge and the individual's needs. Older adults and frail people may experience next day sedation due to the long half-life of diazepam.
- Drug interactions and drug-disease interactions should be considered.
- Dose equivalents vary between authors, they are based on clinical experience but may vary between individuals.[87]
| Drug | Approximate equivalent dose | Half-life (hours) (active metabolite) |
|---|---|---|
| Diazepam | 5mg | 20 – 100 (36 – 200) |
| Chlordiazepoxide | 12.5mg | 5 – 30 (36 – 200) |
| Clobazam* | 10mg | 12-60 |
| Clonazepam* | 0.25mg (250mcg) | 18 – 50 |
| Loprazolam | 0.5mg (500mcg) -1mg | 6 – 12 |
| Lorazepam | 0.5mg (500mcg) | 10 – 20 |
| Lormetazepam | 0.5mg (500mcg) -1mg | 10 – 12 |
| Oxazepam | 10mg | 4 – 15 |
| Nitrazepam | 5mg | 15 – 38 |
| Temazepam | 10mg | 8 – 22 |
| Zolpidem | 10mg | 2 |
| Zopiclone | 7.5mg | 5 – 6 |
Adapted from the Ashton Manual, Maudsley Prescribing guidelines, UK Medicines Information Question and Answer69,84,87
* Clobazam and clonazepam may be prescribed for intractable epilepsy, caution if considering reducing dose
Reduction schedules
When reducing B-Z do not prescribe other psychotropics to compensate unless a specific condition or disorder is being treated.
There are multiple tapering schedules, due to variations in medicines, doses and dose frequency, see The Ashton Manual for examples. There is also a need to tailor reductions to individual needs and preferences, such as stopping a morning dose rather than a lunch time dose. While the following reduction steps are considered appropriate, for some individuals smaller reductions may be necessary.69,84
Reduction dose varies with starting dose. Reduce by:
- 10mg/day every two to four weeks, down to a total daily dose of 50mg
- 5mg/day every two to four weeks, down to a total daily dose of 30mg
- 2mg/day every two to four weeks, down to a total daily dose of 20mg
- 1mg/day every two to four weeks, until stopped
| Step | Morning (mg) | Lunch (mg) | Night (mg) | Total daily dose (mg) |
|---|---|---|---|---|
| Starting dose | Diazepam 5 | Diazepam 5 | Diazepam 5 | 15 |
| Step 1 | 5 | 4 | 5 | 14 |
| Step 2 | 5 | 3 | 5 | 13 |
| Step 3 | 5 | 2 | 5 | 12 |
| Step 4 | 5 | 1 | 5 | 11 |
| Step 5 | 5 | Stop | 5 | 10 |
| Step 6 | 4 | - | 5 | 9 |
| Step 7 | 3 | - | 5 | 8 |
| Step 8 | 2 | - | 5 | 7 |
| Step 9 | 1 | - | 5 | 6 |
| Step 10 | Stop | - | 5 | 5 |
| Step 11 | - | - | 4 | 4 |
| Step 12 | - | - | 3 | 3 |
| Step 13 | - | - | 2 | 2 |
| Step 14 | - | - | 1 | 1 |
| Step 15 | Stop | Stop | Stop | 0 |
| Step | Morning (mg) | Teatime (mg) | Night (mg) | Total daily dose (diazepam mg) |
|---|---|---|---|---|
| Starting dose | Diazepam 5 | Diazepam 5 | Temazepam 20 | 20 |
| Step 1 | Diazepam 5 | Diazepam 5 | Diazepam 10 | 20 |
| Step 2 | 5 | 4 | 10 | 19 |
| Step 3 | 5 | 3 | 10 | 18 |
| Step 4 | 5 | 2 | 10 | 17 |
| Step 5 | 5 | 1 | 10 | 16 |
| Step 6 | 5 | Stop | 10 | 15 |
| Step 7 | 4 | - | 10 | 14 |
| Step 8 | 3 | - | 10 | 13 |
| Step 9 | 2 | - | 10 | 12 |
| Step 10 | 1 | - | 10 | 11 |
| Step 11 | Stop | - | 10 | 10 |
| Step 12 | - | - | 9 | 9 |
| Step 13 | - | - | 8 | 8 |
| Step 14 | - | - | 7 | 7 |
| Step 15 | - | - | 6 | 6 |
| Step 16 | - | - | 5 | 5 |
| Step 17 | - | - | 4 | 4 |
| Step 18 | - | - | 3 | 3 |
| Step 19 | - | - | 2 | 2 |
| Step 20 | - | - | 1 | 1 |
| Step 21 | Stop | Stop | Stop | 0 |
| Step | Morning (mg) | Night (mg) | Total daily dose (diazepam mg) |
|---|---|---|---|
| Starting dose | Lorazepam 1 | Lorazepam 1 | 20 |
| Step 1 | Lorazepam 1 | Diazepam 10 | 20 |
| Step 2 | Diazepam 10 | Diazepam 10 | 20 |
| Step 3 | 9 | 10 | 19 |
| Step 4 | 8 | 10 | 18 |
| Step 5 | 7 | 10 | 17 |
| Step 6 | 6 | 10 | 16 |
| Step 7 | 5 | 10 | 15 |
| Step 8 | 4 | 10 | 14 |
| Step 9 | 3 | 10 | 13 |
| Step 10 | 2 | 10 | 12 |
| Step 11 | 1 | 10 | 11 |
| Step 12 | Stop | 10 | 10 |
| Step 13 | - | 9 | 9 |
| Step 14 | - | 8 | 8 |
| Step 15 | - | 7 | 7 |
| Step 16 | - | 6 | 6 |
| Step 17 | - | 5 | 5 |
| Step 18 | - | 4 | 4 |
| Step 19 | - | 3 | 3 |
| Step 20 | - | 2 | 2 |
| Step 21 | - | 1 | 1 |
| Step 22 | - | Stop | Stop |
Note: See approximate dose equivalents and switching considerations above. Lorazepam is more potent and has a shorter half-life than diazepam. Therefore, cross tapering may be appropriate as a first step to allow assessment of tolerance and adverse effects (e.g. sedation, withdrawal) prior to active reduction.
| Step | Morning (mg) | Lunch (mg) | Tea (mg) | Night (mg) | Total daily dose (diazepam mg) |
|---|---|---|---|---|---|
| Starting dose | Diazepam 10 | Diazepam 10 | Diazepam 10 | Temazepam 20 | 40 |
| Step 1 | Diazepam 10 | Diazepam 10 | Diazepam 10 | Diazepam 10 | 40 |
| Step 2 | 10 | 5 | 10 | 10 | 35 |
| Step 3 | 10 | 5 | 5 | 10 | 30 |
| Step 4 | 10 | 4 | 4 | 10 | 28 |
| Step 5 | 8 | 4 | 4 | 10 | 26 |
| Step 6 | 6 | 4 | 4 | 10 | 24 |
| Step 7 | 4 | 4 | 4 | 10 | 22 |
| Step 8 | 4 | 2 | 4 | 10 | 20 |
| Step 9 | 4 | 1 | 4 | 10 | 19 |
| Step 10 | 4 | Stop | 4 | 10 | 18 |
| Step 11 | 4 | - | 3 | 10 | 17 |
| Step 12 | 4 | - | 2 | 10 | 16 |
| Step 13 | 4 | - | 1 | 10 | 15 |
| Step 14 | 4 | - | Stop | 10 | 14 |
| Step 15 | 4 | - | - | 9 | 13 |
| Step 16 | 4 | - | - | 8 | 12 |
| Step 17 | 4 | - | - | 7 | 11 |
| Step 18 | 4 | - | - | 6 | 10 |
| Step 19 | 3 | - | - | 6 | 9 |
| Step 20 | 2 | - | - | 6 | 8 |
| Step 21 | 1 | - | - | 6 | 7 |
| Step 22 | Stop | - | - | 6 | 6 |
| Step 23 | - | - | - | 5 | 5 |
| Step 24 | - | - | - | 4 | 4 |
| Step 25 | - | - | - | 3 | 3 |
| Step 26 | - | - | - | 2 | 2 |
| Step 27 | - | - | - | 1 | 1 |
| Step 28 | Stop | Stop | Stop | Stop | 0 |
Contact
Email: EPandT@gov.scot
There is a problem
Thanks for your feedback