Respiratory conditions - quality prescribing strategy: improvement guide 2024 to 2027
Respiratory conditions are a major contributor to ill health, disability, and premature death – the most common conditions being asthma and COPD. This quality prescribing guide is designed to ensure people with respiratory conditions are at the centre of their treatment.
3. Introduction
What is the purpose of this guidance?
Respiratory conditions are a major contributor to ill health, disability, and premature death, with the most common conditions being asthma and COPD.[1] The Scottish Health Survey reported the average incidence of asthma as 16% and COPD as 4%.[2]
The World Health Organisation has identified chronic respiratory disease as a non-communicable disease (NCD) along with diabetes, cancers and cardiovascular disease. NCDs are responsible for 71% of global death annually.[3]
The impact of respiratory conditions can vary depending on many factors. There is often a high prevalence of comorbidities such as heart disease, hypertension and diabetes in individuals with respiratory conditions, which should also be addressed during a prescribing review. Optimising pharmacological treatment of these conditions is vital to help control symptoms and increase the quality of life for the individual.
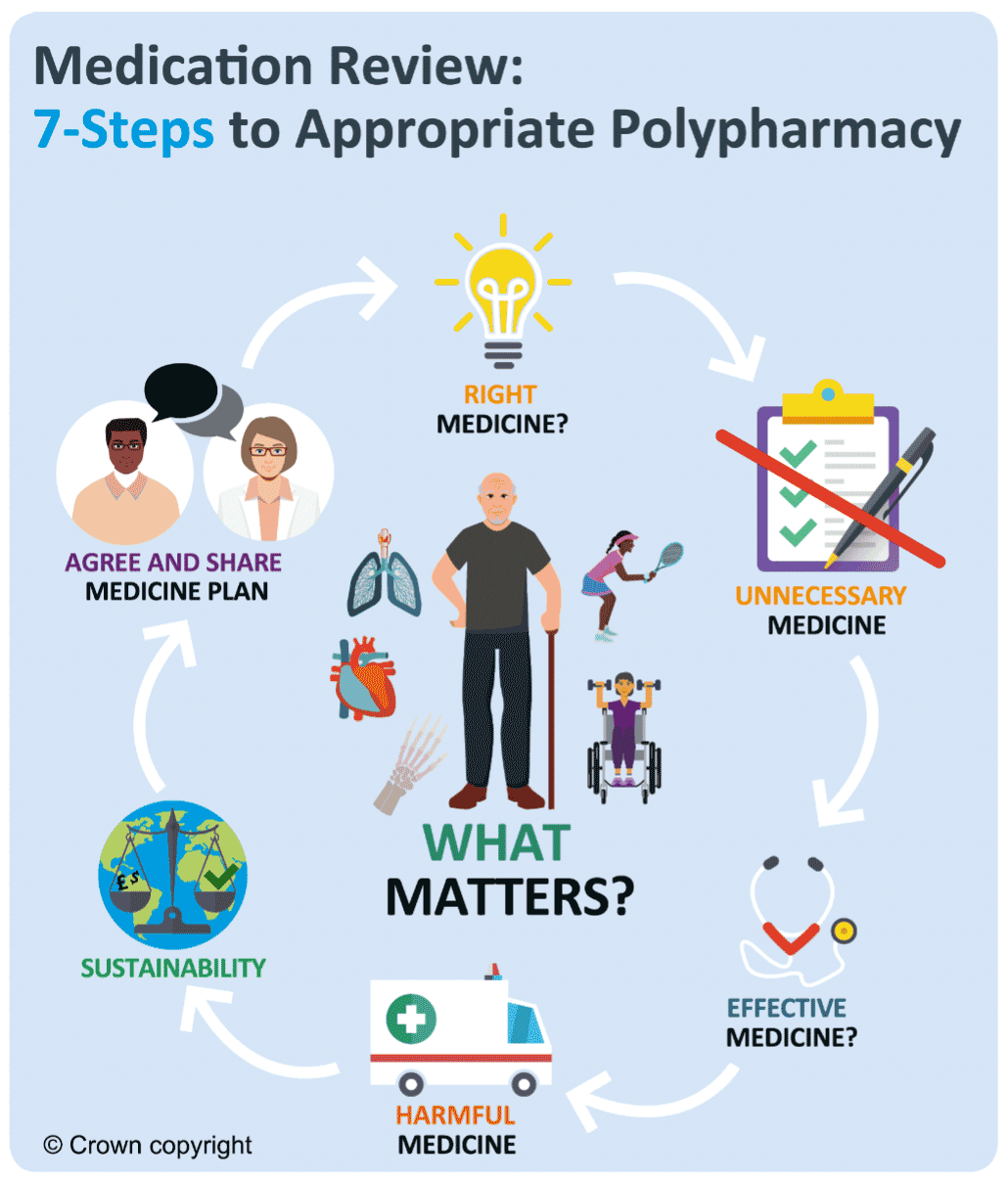
This guidance promotes Realistic Medicine using the holistic 7-Steps polypharmacy approach to medicine reviews that includes shared decision-making, a personalised approach to care, reducing harm and waste and addressing unwarranted variation and ineffective prescribing practice.[4], [5]
This guide will build on what already works well in respiratory prescribing and encourage further quality improvement within NHS Scotland. It highlights key respiratory prescribing indicators, and it is hoped that clinicians will reflect on their current practice in prioritised areas. This guidance should be read in conjunction with clinical guidance such as SIGN[6] or NICE[7] - it is not intended to replace them. The guidance has four main sections on asthma, COPD, bronchiectasis and Interstitial Lung Disease (ILD), focusing on Idiopathic Pulmonary Fibrosis (IPF).
Environmental considerations for respiratory prescribing will be introduced and explored. NHS Scotland has committed to be a net zero greenhouse gas emissions organisation by 2040[8] with more individuals interested in their own carbon footprint.
We sometimes refer to ‘patients’ throughout the document and recognise that different terminology is often used in official documentation. We recognise that patients are people who are managing different medical conditions, including respiratory disease.
Who is the guide for?
It is for all healthcare professionals involved in respiratory care and prescribing decisions in both primary and secondary care including doctors, nurses, pharmacists, pharmacy technicians, physiotherapists and occupational therapists.
The guide will be available on the Polypharmacy: Manage Medicines app for ease of access and as an additional support for patients and clinicians.[9] If clinicians can reflect on their own prescribing practice, it will help reduce unwanted variation of prescribing across Scotland.[10]
Why is the guide important?
What are the benefits of guidance to patients?
This guide focuses on quality prescribing and should result in improvements in patient care and treatment of respiratory conditions. The 7-Steps medication review process promotes a shared decision-making approach to medicine reviews and places the individual at the centre of their care to ensure prescribing is effective and appropriate for them. People will be encouraged to self-manage their condition where appropriate and be asked ‘what matters to you?’[11] to support a holistic approach to care in line with the Scottish Government’s polypharmacy guidance.[5]
What are the benefits to Health Boards?
Optimising therapy through shared decision-making will lead to improved person-centred care. Appropriate and effective use of pharmacological therapy for respiratory conditions will facilitate better outcomes for individuals with respiratory conditions and should reduce healthcare utilisation and hospital admissions due to respiratory disease.
There is an increase in the volume of prescriptions dispensed and the cost of medicines year on year. Appropriate review of respiratory prescribing should improve medication safety and ensure cost effective and sustainable prescribing.
Figure 2 below highlights the spend of respiratory prescribing in primary care in 2022/23 by inhaler type. The total annual spend in 2022/23 was approximately £117.02 million. This represents 9.5% of the Scottish primary care prescribing spend and is £7.81 million less than the total prescribed in 2016/17. Prescribing costs of short-acting Beta2 Agonist inhalers (SABA) have reduced by 3.7% in the same time period. At the same time, there has been an increase in use of long-acting combination bronchodilator inhalers (LABA/LAMA) and triple combination inhalers (ICS/LABA/LAMA) as they are now more widely available and are more cost effective compared to single ingredient inhaler use.
| BNF Chapter | Total Spend | ||
|---|---|---|---|
| Drugs used in respiratory conditions | £117,018,822 | ||
| BNF Section | Section Spend | Class of Respiratory Medicine | Spend |
| Bronchodilators | £32,460,779 | Combination LABA & LAMA | £8,929,750 |
| Combination SABA & SAMA | £55,304 | ||
| LABA | £959,393 | ||
| LAMA | £12,951,530 | ||
| Other | £260,674 | ||
| SABA | £8,949,933 | ||
| SAMA | £124,764 | ||
| Theophylline | £229,429 | ||
| Corticosteroids (respiratory) | £80,369,161 | Combination ICS & LABA | £50,183,468 |
| Combination ICS, LABA & LAMA | £22,508,569 | ||
| ICS | £7,677,125 | ||
| Cromoglycate & LRA | £1,063,467 | LRA | £802,793 |
| Miscellaneous | £260,674 | ||
| Mucolytics | £3,125,414 | Mucolytics for CF | £1,839,063 |
| Mucolytics for COPD | £1,286,350 | ||
Contact
Email: EPandT@gov.scot
There is a problem
Thanks for your feedback