Realistic Medicine - Taking Care: Chief Medical Officer for Scotland annual report 2023 to 2024
This is the Chief Medical Officer Professor Sir Gregor Smith's fourth annual report, and the eighth report on Realistic Medicine. The overarching aim of Realistic Medicine is to deliver better value care for patients, and for our health and care system.
Chapter 2: Taking Care of Our Planet
“I believe we can create a healthy society that protects the planet and safeguards future generations. And although the climate emergency is a global issue, we need a local response in every community.
What drives my passion for greener practice is that this local response is one that can transform our communities so that they are healthy and fulfilling places to live.”
Dr Deepa Shah
GP at Levenwick Medical Practice in Shetland
Chair of North East Scotland Greener Practice Group
The planetary crisis
We are in a worsening planetary crisis – facing the triple realities of climate change, pollution and loss of biodiversity. Last summer saw Scotland’s hottest June since records began, last winter was one of the UK’s wettest and global sea levels are rising twice as fast as they were in the 1990s. Around the world, lives are being disrupted, food and water insecurity is worsening, and even as existing inequalities deepen, this crisis is leading to new forms of inequity.
What we choose to do now matters. Many of the anticipated health impacts of climate change in the UK are still avoidable. We must safeguard our natural environment for future generations whilst we still have agency to act. Not only do we need to reduce greenhouse gas emissions to mitigate the warming that our planet will experience, but we urgently need to adapt to the current and future effects of climate change.
We must choose to be responsible global citizens: our wellbeing, our health and the lives of this and future generations depend on this.
Last year, I shared my thoughts on our three priorities for action:
1. The impact of healthcare on the planetary crisis
2. The impact of the planetary crisis on health and care
3. Mitigation and adaptation
I must emphasise the urgency of addressing this planetary crisis and the public health crisis that is unfolding consequently. This year, I would like to put these thoughts into further context. I would like to share real-life examples of action in our systems and beyond. And I would like to inject some realism into the conversation: mitigating and adapting to the planetary crisis must be our number one concern as we work towards our climate-resilient, low-carbon, equitable and sustainable health and care system of the future. We must act quickly, collectively and decisively.
The impact of climate on our health
A quarter of a million additional deaths will occur globally every year between 2030 and 2050 as a result of humanity-driven changes to the climate. This is because climate change affects most of the basic building blocks of health by influencing the day-to-day weather conditions that we experience. How severely this impacts us depends on how much warming occurs.
The United Nations Framework Convention on Climate Change established an upper limit of 2° Celsius warming above pre-industrial level. Beyond this, we are likely to experience rapidly escalating, irreversible and unacceptable effects – on everything from water security to healthcare. But even today, as we approach 1.5° Celsius of warming, the changing climate is already affecting our health in Scotland.
Winter saw Storm Babet sweep across the country, with half the average monthly rainfall for October falling in days and tragically leading to loss of life and hardship. Unpredictable storms and flooding will continue to become more common. By 2050 winter rainfall is expected to increase by 8-12% and sea levels in Edinburgh are expected to rise by 12-18cm. More flooding will compound existing inequalities and the greatest health burden associated with flooding is likely to be the long-term mental health impacts.
While flooding is expected to get worse during Winters, our Spring and Summer temperatures are likely to rise – in tandem with an increase in heat waves. Water scarcity in the summer will add to the burden of winter floods and increase our risk of food insecurity. Nearly half of the UK’s food is imported from abroad and the proportion of food coming from climate-vulnerable countries is increasing. This leaves our food chain vulnerable to climate shocks both at home and abroad. This might affect what we have access to and what we can afford – with the hardest hit likely to be those already struggling with the cost-of-living and existing barriers to accessing healthy, nutritious food.
We must carefully consider how the long-term health impacts of food insecurity could affect the pressures on our system and think of other climate-related risks on the horizon.
Our changing weather and climate also mean a changing pattern of vector-borne diseases. These are illnesses caused by bacteria, parasites and viruses and transmitted by carriers such as fleas, mosquitoes and ticks. Scotland has a disproportionate share of the UK burden of Lyme disease and cases have been increasing over the past five years.
Looking further ahead, climate modelling suggests that invasive mosquito species, which transmit serious diseases like dengue, chikungunya and Zika, may become endemic in England by the 2040s and parts of Scotland by the 2060s – due to a hotter and more humid climate. This is one of the most significant risks that climate change poses to public health in our country and we need to be prepared to respond through contingency planning, habitat management plans and targeted human, animal and vector surveillance.
Being realistic in our response to the planetary crisis means having a sense of what to expect. The Local Climate Adaptation Tool tells us how the climate will change where we live, who will be the most vulnerable and what the health impacts will be. These impacts are major, multifaceted, co-occurring and inequitable and affect us directly, as individuals, and collectively through disruption of the fundamental building blocks of a healthy and fairer society.
Our health and care system must adapt and enact plans to address the immediate and worsening impact on health of flooding, overheating, high winds and storms and water scarcity. NHS National Services Scotland has a critical role here which will underpin our success: to increase resilience of our systems and minimise the impact of climate change, to assure other NHS Boards’ progress towards adaptation and preparedness for worsening natural events and to support the mapping of vulnerabilities across the system, including risks to hospital sites and disruption to the ways staff and patients reach them.
The impact of healthcare on climate
NHS Scotland is making progress towards working in a sustainable way. However the impact of health and care on the climate is significant. Healthcare remains the fifth biggest emitter of carbon dioxide (CO2) – a major greenhouse gas – in the world. This year, three quarters of the Thirteenth Citizens’ Panel, which aims to capture and reflect the views of the Scottish public, agreed that NHS Scotland has a responsibility to reduce its impact on climate change. However, we are not seeing the reductions in emissions required to achieve our goals on Net Zero: the time when we are no longer adding to the total amount of greenhouse gases in the atmosphere.
It was no accident that this year’s Realistic Medicine conference fell on Earth Day. As people around the world gathered and demonstrated in support of our natural environment, it was my great pleasure to hear from the inspirational Maria Gaden, who heads the Centre for Sustainable Hospitals in Denmark. Like us, Denmark is at the start of a sustainability journey. Maria and I know it’s hard for people to change the world from just one country – but I’m optimistic that there is an international community within which we can collaborate, find solutions and drive change at home and further afield through deep global connections.
Maria shared her experience of three approaches to reducing climate impact:
1. Reduce – Not using something saves 100% of the possible carbon impact
2. Reuse – Reusing products recouped 60% of the lifetime carbon impact of the product
3. Recycle – Recycling consistently could recoup 3-4% of the carbon impact of the product
To help address the climate emergency, the number one thing we can do as professionals is to create less waste when we deliver healthcare.
Carbon accounting will feel intuitive one day. We’re not quite there yet, so we need to apply some common sense and use a currency that we all understand. For example, if we can’t calculate the carbon cost of what we’re using, we can simply weigh the amount of waste we generate and work to reduce that weight.
Reducing waste in surgery
In the Central Denmark region, the consumption of single-use surgical products in hip replacement surgery ranged from 7.1 kg to 12.5 kg per procedure, depending on the surgeon, with similar outcomes. In some cases, products were not used during the surgery but disposed of anyway. Variation was mainly a result of surgeon preference, culture, assumptions and local habits – not clinical need.
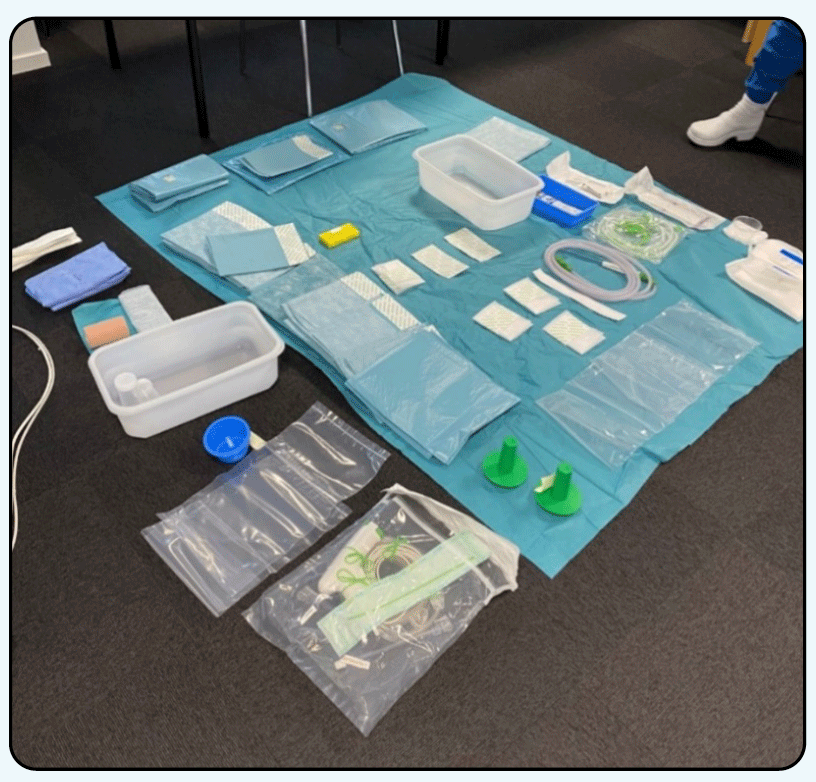
A surgical drape and surgical equipment.
Everything not on the blue drape above is being phased out: saving resource, plastic and CO2. We should follow suit and consider what we can safely stop using.
Maria also questions the purchasing of single-use equipment. She has studied the carbon footprint of multiple-use versus single-use suturing sets (i.e., scissors, tweezers and needle holder). Multiple-use sets had 90% lower CO2 emissions than single-use sets, with the same lifetime costs. There was no evidence that single-use sets improved safety and clinicians preferred multiple-use sets because of the quality of the products.
While there are many examples of good practice in Scotland, single-use has become the standard in many places. Switching will take initial investment, changes in procurement, remanufacturing services and building sterilisation capacity. However, this is an investment that should pay for itself over the lifetime of the equipment.
Maria’s lessons – reduce, reuse, recycle – are easy to follow. They are about how getting the basics right can benefit people, planet and pound.
The changes our society needs to make cannot be accomplished by health and care professionals alone, but we can start the conversations and leverage our trusted positions to role-model best practice.
Culture of stewardship
While addressing CO2 emissions from health and care is fundamental to planetary health, I’d also highlight that the most harmful care for our planet is the wasted and futile care that makes no difference to the lives of the people we care for. The Organisation for Economic Co-operation and Development estimates that 20% of healthcare spend does not meaningfully improve our health.
This consumption of resource without benefit is also more likely to prevent those who are disadvantaged from receiving the care that they need. It is also a drain on our natural resources and increases harmful emissions – wasteful care is poor care for the people we care for and our environment and increases the potential for harm to them both.
To fully tackle the climate emergency, effective collaborative working across the healthcare system will be vital. Health and care professionals must be supported as we develop a culture of stewardship, where resources – everything from the gloves we wear to how our time is used – are safeguarded and used responsibly.
Your impact
Interested in your impact? You can use this tool to calculate the non-clinical carbon footprint of your GP surgery. This accounts for about 40% of primary care emissions. Then connect with your local Greener Practice team to find out how other GPs are reducing their impact!
Transitioning towards sustainability can be complicated by hygiene, costs, work environment, cooperation, efficiency, culture and behavioural considerations. While it is easy to feel overwhelmed, we must question established practices and we must take action to reduce consumption in a safe and responsible way.
And through careful and kind care, we can also focus on delivering the outcomes that matter. We can reduce waste and potential harm, deliver better value care, reduce our environmental impact and help to create a more sustainable health and care system. Tackling this crisis is challenging – but we know that many of the changes we need to make that are good for the planet will also be good for our health.
Zero emissions fleet
My colleagues in Health Infrastructure and Sustainability have been gathering data related to our emissions across NHS Scotland. Between 2016 and 2023, NHS Scotland’s total heat and power emissions have reduced by 32%. This is great – and mostly driven by decarbonisation of the electricity grid.
NHS Scotland is aiming to fully decarbonise its fleet of vehicles by 2032. This is a critical step on our journey to a Net Zero service, as we know that domestic transport is the sector which produces the most greenhouse gas emissions in Scotland (29% of the total for 2019) and that car travel makes up the most carbon-intensive mode of transport.
Between October 2022 and March 2023, the proportion of Zero Emissions Vehicles (ZEV) in our fleet increased from 19 to 33% — with NHS Ayrshire & Arran moving from only 5% to nearly half their fleet.
I’ll talk later in this chapter about our role as anchors in our communities – taking the lead on ZEVs will improve our local air quality, reduce our carbon footprint and serve as a beacon for our direction of travel.
Some of the tools we need to reduce emissions are already here. In my report A Fair And Sustainable Future in 2022, I highlighted Near Me, a video-based virtual consultation service which saw huge expansion at the height of the COVID-19 pandemic as we sought to minimise transmission risk. Near Me is now embedded across health and care in Scotland– a business-as-usual service providing nearly 400,000 consultations last year. The average journey saved per consultation was 43 miles – a potential saving of millions of miles per month. Kind to people and kind to our planet.
NHS Highland has embedded a pathway for kidney replacement therapy which is underpinned by a philosophy of careful and kind care. This pathway aims to minimise the impact of healthcare on people’s lives and the planet and strikes the right balance between the science and the art of care – placing biometric and biographical care in equilibrium while caring for the environment. It’s a great example of locally-led climate-first innovation from NHS Highland’s specialist renal team.
Incremental dialysis
Nearly 2,000 people in Scotland currently benefit from haemodialysis, a form of kidney replacement therapy. Haemodialysis is a life-saving intervention in chronic kidney failure, but one that comes at a high cost to the people we care for, our system and the environment. A single dialysis session uses 400 litres of water (2/3 of which is wasted) and it has been calculated that 7.1 tonnes of CO2 are emitted per year for each dialysis patient.
Taking an evidence-informed approach, the specialist renal team in NHS Highland has transformed the service that they deliver – establishing an incremental dialysis pathway. Incremental dialysis means providing the minimum effective amount of kidney replacement therapy, rather than taking a one-size-fits-all approach.
In just one year, the specialist renal team saved:
- 648,000 litres of water
- 53,090 miles of travel
- 74 tonnes of CO2 from being emitted
- 3.6 tonnes of non-recyclable waste
- £84,072 in taxis
- £27,850 in consumables
- £2,722 in medication
Most importantly, patients appreciated this realistic approach to their care – as “It made starting dialysis a bit less scary,” meant they could “spend more time with family,” and it ensured that dialysis wasn’t “affecting my ability to work”.
This team have viewed national guidelines through the lens of local clinical expertise to achieve outcomes that matter, and this willingness to approach old problems in new and dynamic ways is at the heart of Value Based Health and Care.
Pollution and our health
Worldwide, pollution is responsible for 16% of all deaths and for economic losses totalling 6.2% of global economic output.
In Scotland, outdoor air pollution is implicated in approximately 1,800 to 2,700 deaths every year, making it the largest environmental risk to public health. Air pollution is caused by fine particulate matter released from a variety of sources. We have some of the most stringent air pollution regulations in the world – but these fall short of WHO recommendations and, in countries with similar ambient levels of air pollution to Scotland, there is compelling evidence of harm.
Environmental Standards Scotland reported this year that we need to consider where the most vulnerable people in society live and take targeted action.
Children are disproportionately affected by air pollution because they spend more time outdoors than adults and because their developing lungs are more sensitive.
Air pollution drives paediatric admissions
Researchers at the University of Dundee recently looked into 35,000 admissions to Ninewells Hospital and matched these admissions to trends in local air pollution. They found the number of children admitted into hospital rose when markers of air pollution were high and that children seemed markedly more vulnerable to rising levels of air pollutants than adults. They concluded that two out of every five children admitted to hospital with breathing concerns in Dundee could avoid admission in the future if air pollutant levels could be kept within safe recommended limits.
The healthcare we provide is also a major source of pollution. The most common therapeutic intervention in our system is the prescription of medicines. We are all aware of the harm medicines can sometimes do – but we don’t often think of them harming the environment.
The recent Citizens’ Panel found that 7 in 10 people would support considering the environmental impact of their treatment options as part of deciding their treatment with their health professional, and nearly 8 in 10 would support choosing one medicine over another because it has less impact on the environment.
iSIMPATHY – Stimulating Innovation in the Management of Polypharmacy and Adherence Through the Years – is a European Union-funded collaboration between Scotland, Northern Ireland and the Republic of Ireland. This project aimed to tackle the health, climate and financial harms associated with the use of multiple medicines through innovate collaborative pharmacist-led medicines reviews.
Key findings from the evaluation include:
- 82% of interventions were clinically significant, while 4% of interventions potentially prevented major organ failure or significant adverse drug reactions
- the appropriateness of medicines improved in 92% of reviews, with an average reduction of one medicine (from 12 to 11)
- economic benefits to the wider healthcare system were identified, with direct medicines cost savings of £13,100 and a potential total of £168,800 savings from avoided healthcare resource usage per 100 reviews
- patients reported better understanding of their medicines, improved adherence and experienced less harm
- an average of 7.4 Quality-Adjusted Life Years (QALY) were gained per 100 patients
iSIMPATHY has set a blueprint for undertaking reviews for people taking multiple medicines and will have implications for practice and environmental sustainability across NHS Scotland - find out how to do these on Turas. There is work already underway to embed the successful models used by the project in medicines reviews and Patient Reported Outcome Measures which gather views of people using services.
Our food
Climate has a profound impact on our food supply. Changes in temperature and precipitation patterns can affect crop yields and livestock productivity both here in Scotland and abroad. Extreme weather events like droughts, floods and storms can damage crops and infrastructure, disrupting food productions and distribution. All of this can increase the costs of production and the price people pay for food. Increasing food prices impact most on our communities who are already struggling to make ends meet. An inability to buy healthy food has an adverse impact on our health and wellbeing.
The biodiversity of our natural world is one of Scotland’s greatest assets. We must look at ways in which we can better understand the impact of climate on our food and the importance of our connection with nature.
I am adding my voice to the need for a fundamental shift in our society’s relationship with food. Our diet needs to move towards healthy food habits that consider water, emissions and land usage. Good nutrition is the cornerstone of good health – but agriculture takes up half of the planet’s habitable land and worldwide food systems are responsible for a quarter of the planet’s greenhouse gas emissions. Of that quarter, the majority is down to the production of meat and dairy products.
On any given day, 86% of adults in Scotland consume some kind of meat and almost everyone consumes dairy in one form or another. Food Standards Scotland modelled the impact of reductions in meat and dairy consumption. It’s a complicated picture – diets in Scotland are just not healthy and varied enough to say we can do away with the crucial micronutrients that meat and dairy contain. What we can do is aim for our intake to be less than 70g per day of red and red processed meat. If we can manage this as a society, there will be an estimated reduction of around 10,000 cases of Type 2 diabetes over a ten-year period, and a reduction in the rate of colorectal cancer.
We can take a leaf out of Keep Scotland Beautiful’s Pocket Garden book and inspire a positive relationship with food in the next generation. This project connects children with their food and with nature: a Pocket Garden is a miniature garden that uses edible plants, plants that attract wildlife and that reuses something which would otherwise have been thrown away.
Pocket Gardens
Staff and pupils at Firpark Primary School in Motherwell produced a “Fairy Herb Garden,” last year, celebrating the hard work of NHS staff. All the plants in the garden are edible and are being used to make healthy meals.

Firpark Primary School’s Fairy Herb Garden – A Celebration of Our NHS
The benefits of children and young people eating well cannot be overstated. In every culture, food is a vehicle for connection, and Community Food Initiatives North East (CFINE) takes this idea to heart. This is a truly inspiring third sector organisation working in the North of Scotland that uses affordable locally sourced fruit and veg as an opportunity to have human conversations. Making it easy to access healthy food allows their staff and volunteers to ask: “What else is going on that brought you to us? And can we help?”
This local team “knows what’s out there” to help disadvantaged, vulnerable and low-income families and communities to live the lives they want to live by supporting access to education and work. This approach, which starts with finding out what matters, then working together to find solutions, is something that I feel we need to see more of.
Our role as anchors in our communities
We must achieve a culture of stewardship within NHS Scotland, where resources are safeguarded and responsibly used to provide environmentally sustainable healthcare. Care and caring are fundamental to what we do. We should be thinking about the triple focus of improving outcomes for the people we care for while reducing environmental impact and ensuring the sustainability of our services – people, planet and pound.
The communities which we serve, and are often a part of, can help us tackle the planetary crisis. NHS Scotland’s anchor institutions are driving positive change across our society. Our healthcare service is made up of large organisations which have significant presence in local communities. This presence – anchored in place – gives them significant power to distribute wealth and assets within our communities through deliberate decisions to recruit and procure locally, and to ensure land and assets are used to the benefit of the local community.
Our systems are built on a model of continuous consumption and this leaves us vulnerable. By deliberately choosing environmentally friendly options while supporting our local communities, decision-makers in our anchor institutions can work towards a wellbeing economy in concert with people, equity and the planet.
Places for people and planet
With 278 hospital sites and buildings alone in Scotland, NHS Scotland owns a significant amount of land and buildings. Land and assets can be made available and used in ways which benefit local communities. This is a key way for the NHS to boost local social, environmental and economic wellbeing.
GP surgeries are time-tested assets in every community and will be pivotal in our move towards a greener and more sustainable health and care system. Greener Practices is a network of GPs leveraging their passion for the environment through practical, local action on sustainability in Primary Care and the community. Colleagues in Dundee have shared their story of greening with their local community:
Greener Practices in Dundee
Douglas Medical Centre in Dundee teamed with local government, NatureScot, academia, the arts, the third sector and a local school to create, nurture and enjoy a Wee Forest – a tennis court-sized, densely-planted and fast-growing, native species-rich woodland in urban Scotland, nurturing citizen science and volunteering.
Dundee City Council provided seven raised beds to get going and Scottish Water provided water butts to harvest rainwater from the surgery for watering the garden areas.

Greenery flourishing in Douglas Medical Centre’s Wee Forest
They are putting the space to good use — collaborating with RockSolid Youth Project to develop a community gardening group, growing vegetables for the Community Larder, sharing ideas with Claypotts Primary School for the adjacent plot, working with the local Men’s Shed to create an outside seating area and, last summer, Art at the Start came along once a week to run outdoor art classes for preschoolers.
The power of community and the privileged role health and care professionals hold in this community have created a special place for wellbeing and connection – an asset to people and an asset to the planet.
Strengthening local communities
Providing good quality and stable employment can address health inequalities and the social determinants of health. This includes supporting people who are furthest from the labour market into employment, ensuring staff have opportunities to grow and progress throughout their career.
NHS Scotland is Scotland’s biggest employer – a community of more than 180,000 people that make up 7% of all people in work in Scotland. We have huge power as a community and can leverage our connections for local benefit. The NHS Scotland Community Benefits Gateway is helping to deliver community benefit support to local Ayrshire charities, including equipment, repairs to buildings, assistance to build community facilities, training support or advice and much more.
Community Benefits Gateway in action
Last year, 25 Ayrshire community need requests were registered on the gateway and NHS Scotland and NHS Ayrshire & Arran suppliers have supported the delivery of a number of community benefits.
The Ayr Housing Aid Centre asked for assistance to replace and upgrade their headquarters’ ageing IT equipment. NHS supplier Hewlett Packard supported their request by reviewing the centre’s IT equipment and providing advice on upgrading the equipment. They put the charity in touch with the Edinburgh Remakery, an environmental social enterprise which champions the circular economy refurbishing unwanted electronic devices and passing them on to be used again. Edinburgh Remakery donated modern specification refurbished IT equipment to Ayr Housing Aid Centre. The new modern up-to-date refurbished computer equipment has greatly improved the centre’s computing capacity and efficiency at a vastly reduced cost.
This is a great example of organisations working together to support the wellbeing of local communities.
Supporting local businesses
NHS Scotland purchases £2.5billion worth of goods and services each year from around 8,000 suppliers. By sourcing and procuring locally, with organisations that work ethically and sustainably, NHS boards can help bring wealth back into the community.
NHS Ayrshire & Arran has taken this message to heart — working with 214 local suppliers and increasing local procurement spending by 36% in just a year to more than £13million. This focus on local procurement is supporting local suppliers and generating wealth in the local community. NHS Ayrshire and Arran are also supporting small and medium enterprises by increasing spend from £53million in 2022 to £69million in 2023.
Wellbeing Economy Governments partnership
In the face of increasing pressure on public services and funds, traditional approaches to economic growth are deepening inequalities in our society, while limiting our ability to respond to the climate crisis. A new approach, where the economy serves people and planet first, is needed.
As a founding member of the Wellbeing Economy Governments partnership, Scotland has ambitious plans to reshape our economy into something fairer and greener. To effect this change the aspirations of all sectors including health and care must align. Our communities are at the core of sustainable change. Further radical action by our anchor institutions and local and global communities is needed.
We are making excellent progress with the development of our anchor institutions to enable the people in our communities to flourish. Our anchor institutions are already modelling success – like investing in community polytunnels for fresh vegetables by NHS Orkney. We must continue to find ways to maximise our impact on local health and wellbeing, and meaningfully deploy our significant power, including by providing more employment opportunities for local people and buying more often from local suppliers.
Imperial College Healthcare NHS Trust in London is using their Health & Equity Framework to help to join the dots between initiatives already underway and, importantly, to spot and address key gaps. They are attempting to get the right balance between actions to improve equity of access, experience and outcomes for the people they care for – not only in their core activities (clinical care, research and education), but also those that contribute to wider efforts to improve health and to reduce inequalities due to social determinants of health (such as employment, housing, literacy levels and structural racism).
Developing a sense of connection to the local community can be difficult when starting a new job. Dr Dominique Allwood, CMO at UCLPartners, recently shared a project she is leading where new NHS staff members are invited to a walking tour around the community they serve, and encouraged to spend time in local cafes and businesses to get an understanding of the lives of the people living there. This is an innovative and very human idea. Perhaps we might think about taking a similar approach in Scotland?
A future where we flourish
The planetary crisis is the single biggest threat facing our collective wellbeing across the world. As health and care professionals, we have a duty to practise sustainably, to use resources wisely. We must leverage our expertise, insight and humanity to help set the natural world on the road to recovery.
But progress can be slow, and action is not keeping pace with aspiration or with need. We must accelerate our efforts towards a more sustainable system that will benefit the people we care for, our population and our planet.
We must stop using resources when we don’t need to, especially single-use equipment, and we must remake what we can and recycle the rest. We must identify and halt wasteful and futile care that makes no difference to the lives of the people we care for. The continuing consumption of resource without benefit and that results in planetary harm will affect those who are from our disadvantaged communities the most, and only increase inequity.
To fully tackle the planetary crisis, we must continue to collaborate and strengthen our links with industry and the third sector whilst developing our pivotal role as anchors within the communities we serve. By understanding their needs in their place, we can provide care and outcomes that matter to them – ensuring our communities and our planetary health prosper.
Contact
Email: realisticmedicine@gov.scot
There is a problem
Thanks for your feedback