Realistic Medicine - Taking Care: Chief Medical Officer for Scotland annual report 2023 to 2024
This is the Chief Medical Officer Professor Sir Gregor Smith's fourth annual report, and the eighth report on Realistic Medicine. The overarching aim of Realistic Medicine is to deliver better value care for patients, and for our health and care system.
Chapter 3: Taking Care of Progress
“It’s the 50th anniversary of the Chief Scientist Office, so let’s talk about innovation – and why we need to grasp the innovation revolution now.
The most satisfying thing for me is taking discoveries, new things, from bench to bedside for the benefit of the people we care for – this is my passion. I want it to be your passion too – innovation, science and technology applied to your clinical arena.”
Professor Dame Anna Dominiczak
Scotland’s Chief Scientist for Health
Regius Professor of Medicine at the University of Glasgow
Introduction
Research and innovation are essential to support sustainable healthcare. They help refine and validate new technologies, techniques and treatments and foster collaboration between healthcare professionals, scientists and patients to drive improvements in care and outcomes.
Scotland has been at the forefront of medical developments, and our NHS is seen as a world-leader in healthcare quality and research. We continue to build on our successes to meet the changing needs of the people of Scotland.
In this chapter I celebrate the 50th anniversary of the Chief Scientist Office (CSO), research and innovation in Scotland and how they continue to help the way we care, and the people we care for, to flourish.
Looking back at the past decade of CSO achievements
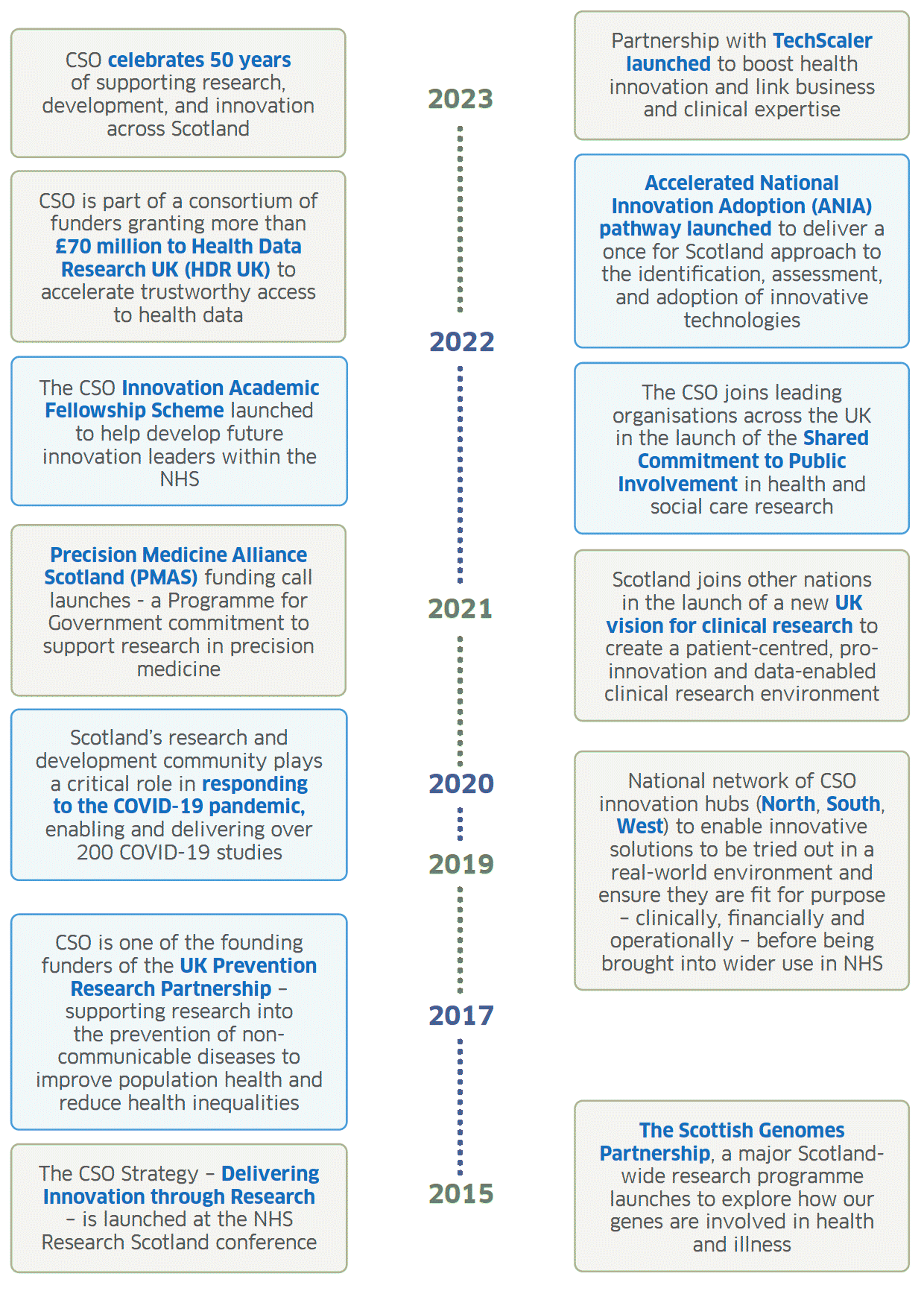
Graphic text below:
Partnership with TechScaler launched to boost health innovation and link business and clinical expertise
CSO celebrates 50 years of supporting research, development, and innovation across Scotland
2023
Accelerated National Innovation Adoption (ANIA) pathway launched to deliver a once for Scotland approach to the identification, assessment, and adoption of innovative technologies
CSO is part of a consortium of funders granting more than £70 million to Health Data Research UK (HDR UK) to accelerate trustworthy access to health data
2022
The CSO Innovation Academic Fellowship Scheme launched to help develop future innovation leaders within the NHS
The CSO joins leading organisations across the UK in the launch of the Shared Commitment to Public Involvement in health and social care research
Precision Medicine Alliance Scotland (PMAS) funding call launches - a Programme for Government commitment to support research in precision medicine
Scotland joins other nations in the launch of a new UK vision for clinical research to create a patient-centred, pro-innovation and data-enabled clinical research environment
2021
Scotland’s research and development community plays a critical role in responding to the COVID-19 pandemic, enabling and delivering over 200 COVID-19 studies
2020
National network of CSO innovation hubs (North, South, West) to enable innovative solutions to be tried out in a real-world environment and ensure they are fit for purpose – clinically, financially and operationally – before being brought into wider use in NHS
2019
CSO is one of the founding funders of the UK Prevention Research Partnership – supporting research into the prevention of non-communicable diseases to improve population health and reduce health inequalities
2017
The Scottish Genomes Partnership, a major Scotland-wide research programme launches to explore how our genes are involved in health and illness
The CSO Strategy – Delivering Innovation through Research – is launched at the NHS Research Scotland conference
2015
We can all be innovators and improvers by taking the best of science, technology and new techniques and transforming them into care and outcomes that matter. Improving and innovating must be central to the way we care. It sits at the core of Realistic Medicine. We must embrace innovation if we are to deliver Value Based Health and Care.
Scotland values research and innovation
For centuries, we have been innovators – educators and philosophers, technicians and scientists, nurses and doctors and the whole spectrum of colleagues who carry, promote and advance health and care in Scotland.
Our National Innovation Strategy pitches innovation as our forward-thinking and outward-looking obsession and I could not agree more. It is powering our Economic Transformation into a wealthier, fairer and greener Wellbeing Economy. And we know that it can change and save lives. I was not surprised to hear that nearly two thirds (64%) of our colleagues consider themselves innovators – and, importantly, feel they have the ideas we’re looking for to safeguard and improve our NHS. I am extremely encouraged by this.
Research is vital in delivering care that matters. It sits at the heart of evidence -informed practice. Indeed, the General Medical Council now advises that we should all consider opportunities for research and let people know we can support them if they themselves want to participate in research. In doing so we can collaborate with the people we care for and make a real and positive difference to the health and wellbeing of Scotland. And we know that society wants to make a difference because over 300,000 people have registered for SHARE – The Scottish Health Research Register and Biobank. I was delighted to hear that we have such an enthusiastic movement of people supporting medical science across the country – and know that they will welcome even more volunteers.
We have no end of home-grown powered-by-people initiatives, like Generation Scotland. This collection of studies, looking at the health and wellbeing of over 7,000 families in Scotland, is a true collaboration between the Chief Scientist Office, NHS Scotland, researchers in four of our great universities (Aberdeen, Dundee, Edinburgh and Glasgow) and the communities they serve. Family studies like this are foundational to managing risk by helping us understand how heritability shapes us and influences our health.
Generation Scotland
4.9 million people across the UK live with diabetes – 90% of whom have Type 2 diabetes. In recent years, there has been a rapid rise in under-40s in the UK diagnosed with Type 2 diabetes. This has a huge impact on these individuals, their families and the health and care systems supporting them.
Analysing changes to DNA in the blood can help us predict who these people are going to be – and this can tell us who needs the most support to avert the onset of diabetes before problems develop. This is the groundbreaking finding of Generation Scotland’s recent study.
Scientists looked at the influence of these changes – known as DNA methylation – alongside other risk factors in nearly 15,000 volunteers to predict the likelihood of developing the condition years in advance of any symptoms developing.
The findings could help us identify those most likely to develop Type 2 diabetes – and put the targeted support in place to nurture a healthier lifestyle. This is how we can use innovation to manage risk and reduce the huge impact of the issues that are linked to Type 2 diabetes – including heart disease, kidney disease and dementia.
This proof-of-concept means similar approaches could be taken for other common health conditions – generating broad health predictors from a single blood or saliva sample. But Generation Scotland needs you to help — the more people that join these studies, the more precisely we can identify these signals and help delay or prevent the onset of diseases as we age. The Next Generation is recruiting families now!
I often talk about the need to work in partnership with the people we care for and research should be no different. Empowering people to play an active role in our vibrant research community, whoever and wherever they are in Scotland, means meaningful inclusion. This is the understanding that their individual history, both biology and biography, will lead to better research and, down the line, better outcomes.
Our research and innovation landscape must also represent and reflect the diversity of our society if we are to achieve outcomes that matter.
The more we understand about the biology and biography of the people of Scotland, the greater scope we have to tailor healthcare to the individual. Scotland is the home of Precision Medicine – the opposite of a one-size-fits-all approach to healthcare.
This is a careful approach to care - powering earlier diagnoses, targeted treatments and prompt interventions. The right plan, and the right treatment at the right time, will increase our chances of delivering careful and kind care, as well as the outcomes that matter.
Here are just a few examples of the cutting-edge Precision Medicine innovations in Scotland:
- Precision MS Integrating precision metrics of brain health into early treatment of multiple sclerosis.
- iDiabetes Tailoring diabetes treatments through enhanced testing and sophisticated analysis of health data.
- PRaCTicAL Accelerating the translation of precision cell therapies for the liver, from the lab bench through to adoption in NHS Scotland.
- TRAITS Enabling time-critical decisions in critically ill patients presenting to emergency departments and Intensive Care Units throughout Scotland.
Triple Helix and the Discovery – Translation – Adoption continuum
A crucial piece of the puzzle is the unified ecosystem that innovation needs to flourish. We have a vibrant life sciences sector in Scotland, contributing significantly to the economy. We have created a continuum between discovery, translation and adoption to capitalise on this, ensuring healthy lives and a sustainable system. I am pleased to share with you our unified efforts to develop a whole-system approach across Scotland, a bench-to-bedside pathway for research, development and innovation. This is already helping to deliver transformative changes to our ways of working.
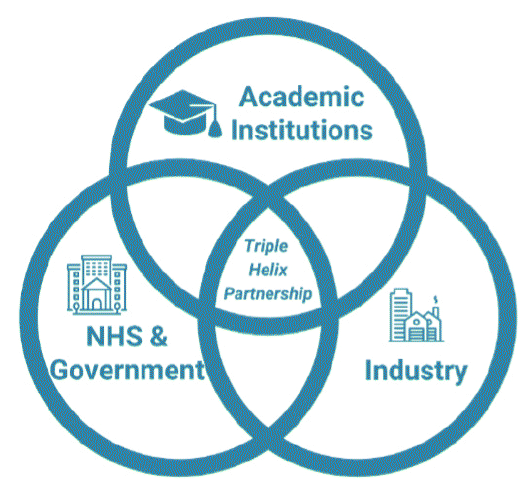
Triple Helix Model
Central to the success of this ecosystem is our forward-thinking and collaborative approach – academia, the NHS and industry working together, driving change and sustaining success for the benefit of the people we care for.
Discovery
Our academic pedigree, of which we are rightly proud, is led by our higher education sector. The Research Excellence Framework, the UK’s peer-review process for assessing quality of research in higher education providers, reported that each of Scotland’s 18 universities is involved in “world-leading” research – and 86% of their research output is internationally excellent. Our great universities, ancient and modern, are fuelling our revolution in health and care. Long-term thinking places discovery science, the earliest explorations of what might be, at the core of future success.
Discovery, by its nature, is outward-looking and open. We should actively seek inspiration beyond the traditional sources, which will give us the best chance of achieving outcomes that matter. We all have networks – professionals, peers, friends – and we can tap into these human connections to find out what works elsewhere and drive local innovation.
Translation
Translation, or taking scientific discovery to the bedside for patient benefit, is the next step. I am proud of our national network of CSO-funded Regional Test Beds which are translating discovery science into reality and improving the lives of those we care for. Our three hubs – North, South East and West, bringing universities and NHS Boards across each region together and fostering practical connections with the life sciences industry.
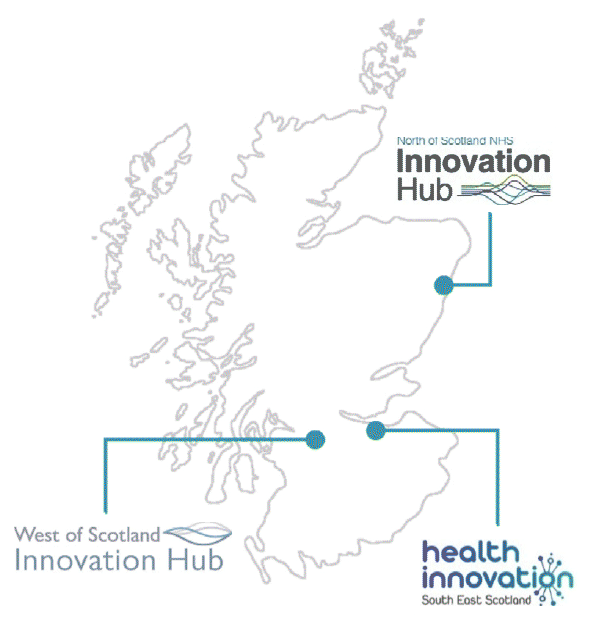
(Above) Map of Scotland with locations of innovation hubs
I’d like to share an example of game-changing innovation from the hubs which is already making a positive difference to the lives of people in the North of Scotland:
Grampian’s Radiology Assist Chest XR Evaluation (GRACE)
This artificial intelligence-driven decision support tool has been a collaborative endeavour involving the Centre for Sustainable Delivery, the Scottish Health Technologies Group, NHS Grampian and Annalise.ai. The tool uses sophisticated pattern recognition to identify possible issues on Chest X-Rays (CXR).
Harnessing this technology, NHS Grampian launched their Rapid Lung Cancer Diagnostic Pathway – with all CXRs across the NHS Board rapidly analysed and flagged if suspicious for lung cancer. The 12-month trial found a reduction between the CXR to CT report time of 22 down to 10.1 days, and the proportion of people with lung cancer meeting the 62-day treatment target increased from 52% to 100%.
This means more people with lung cancer will get an early diagnosis – and treatment can be started earlier when it has a better chance of curing the disease.
It’s tools like this – pushing time-consuming processes to the background of care – that will help clinicians work at the top of their game rather than working at the top of their capacity. There are more initiatives like this in the pipeline, and I hope these will support my colleagues to provide the high-quality care that only their expertise can deliver. However, across the broad spectrum of cancer disease, we must also continually appraise the effectiveness of these new technologies, to ensure that their introduction does not simply result in the overdiagnosis of indolent lesions that otherwise would not have impacted on health outcomes. Developing these insights are important as well for a harm-free, sustainable healthcare future.
Adoption
The NHS was founded on the principle of universalising the best healthcare, but more than 75 years later, we struggle with this concept. Widespread adoption of innovative practice has long been a stumbling block. In response to competing needs, philosophies and priorities, the different parts of our system can sometimes default to siloed thinking and the successes we see up-and-down the country, delivering better quality and better value care, are often confined to the departments or NHS Boards that pioneered them. This approach needs to change and this is why the Accelerated National Innovation Adoption (ANIA) pathway exists.
ANIA is a critical component of our end-to-end innovation pathway – the part that makes the best ideas, the highest impact products, and the most evidence-informed interventions a reality for all the people we care for across the country. Through ANIA, we can ensure the quick and safe rollout of tech innovations – minimising waiting and maximising outcomes that matter.
Rapid adoption of proven innovations is most welcome and much needed.
Digital Dermatology
Digital Dermatology will introduce a standard and straightforward way of capturing a series of triage-quality skin images at the point of referral. These images are then securely transferred, as part of a person’s referral to Dermatology services.
The use of digital images as part of the referral enables, where clinically appropriate, senior dermatology decision-makers to triage, diagnose and assess skin conditions without the patient being physically present. This can improve productivity whilst still providing the same level of access to high quality care, clinical outcomes and patient satisfaction.
This is an innovation that values people’s most precious resource, their time, and could be transformational in the early diagnosis of skin cancers like melanoma. Streamlining a process like this will benefit patients by reducing waiting times and benefit the planet by reducing the need for carbon-intensive travel. And we mustn’t forget that an advantage of these innovations is to free up our time too – so that we can concentrate on the business of caring.
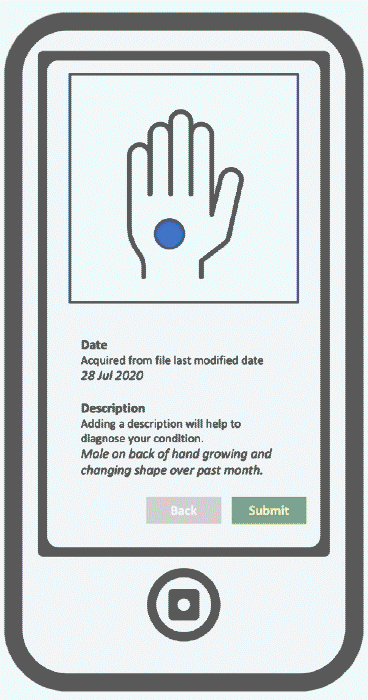
Adapted depiction of the Digital Dermatology App
Crucial to the success of this project, and anything large-scale and forward-thinking that we hope to do, is a more joined-up data environment.
Joined-up thinking
While the COVID-19 pandemic tested the limits of our systems of care, it also presented an opportunity to show the world the value of a connected and enabled National Health Service in a time of crisis.
Scotland’s research community was among the first in the world to produce comprehensive whole-country COVID-19 infection mortality data and followed this with near real-time data on vaccine effectiveness. This was possible because of our unique position – a relatively small population, with world class healthcare infrastructure and academia.
This enhanced surveillance study, led by researchers at the University of Edinburgh, was a global leader in tracking the impact of the COVID-19 pandemic and provided the first real-world data on vaccine effectiveness. The research team managed this in near real-time across Scotland using a rich dataset of all 5.4 million people registered with a GP – around 98% of the Scottish population.
The impact of EAVE II has been profound. EAVE II has directly influenced the decision-making of the Scottish and UK Governments, including when to ease social distancing restrictions.
Several countries around the world – including France, Canada and Germany – altered their policy positions following publication of EAVE II findings, such as making the Oxford-AstraZeneca vaccine available to older people. This shows the outsize impact we can have on people’s lives, not just in the UK, but around the world. This research tells us who would be more or less likely to benefit from a vaccine – helping us, as clinicians, manage risk and provide more personalised care.
EAVE II has shown, unequivocally, just how effective and safe COVID-19 vaccines are – while demonstrating how Scotland can rapidly perform critical whole-population cohort studies in a crisis.
My colleagues in academia have told me that the landscape feels very different as compared to the height of the pandemic, and we may have lost some of the urgency and agency we once had with large-scale studies like this. The biggest barriers to realising this ambition seem to be related to data and information governance and often in the interpretation of this.
We must maintain this world-leading capability if we want to deliver outcomes that matter. The pandemic has shown that Scotland has the potential to be a world-leader in using health data to inform public policymaking, at home and abroad, with huge opportunity in using this to inform a precision approach to population health.
Here’s to the next 50!
We are all aware of the pressure on our health and care system and we know some of the big challenges coming our way. There are lots of difficult calls to make, but we cannot afford to move away from our pursuit of research excellence and, especially, our need to innovate. This is how we ensure that we improve and deliver careful, kind, more sustainable care.
Innovation is everyone’s business – and we know that the greatest innovations spring from a place of passion and expertise. That’s why I am pleased to be supporting a suite of fellowship opportunities, including CSO Innovation Academic Fellowships. Fostering the talents of our health and care professionals through these fellowships will help strengthen our innovation culture, teach how to solve real problems through service transformation and, ultimately, improve the quality, efficiency and sustainability of health and care delivery in Scotland.
Digital technology and artificial intelligence are not replacements for human care – they are merely tools to support us in our role providing the careful and kind care that matters. Artificial intelligence, machine-learning and technology-enabled care have a role to relieve the friction in our system and help us make time for the human connections at the core of our practice.
I am proud of the research that Scotland has given the world – the lives it has improved as well as the lives it has saved.
I am certain that CSO will remain firmly in the vanguard of a collaborative, dynamic and caring health and care system, embracing the future on behalf of Scotland’s people, and it is imperative that it continues to receive the support to do so.
Contact
Email: realisticmedicine@gov.scot
There is a problem
Thanks for your feedback