Ministerial Scottish Nursing and Midwifery Taskforce: report and recommended actions
The final report of the Scottish Ministerial led Nursing and Midwifery Taskforce which makes a number of recommended actions that aim to make Scotland the best place for nurses and midwives to work.
1. The Ministerial Nursing and Midwifery Taskforce
1.1 What is the Ministerial Nursing and Midwifery Taskforce?
In February 2023 the Scottish Government established a Ministerial Nursing and Midwifery Taskforce. The Taskforce originated following requests from the Royal College of Nursing (RCN) and Royal College of Midwives (RCM) as part of the 2023 pay negotiations to address challenges with attracting and retaining nurses and midwives in Scotland. It was agreed that the way forward was to bring stakeholders and experts together. The Taskforce included representatives from:
- NHSScotland
- Social Care
- Nursing and Midwifery Council (NMC)
- professional organisations, incl. representation from RCN and RCM
- trade unions, RCN, RCM, Unison and Unite
- third sector
- academic workforce experts
- Higher Education Institutions
- Council of Deans for Health Scotland
- NHS Education for Scotland
- Scottish Government
(see annex 1 for full membership)
The aim of the Taskforce was to work collaboratively, to listen to nursing and midwifery staff to identify what was important for them, and to develop a workplan of recommended actions to deliver short- and long-term sustainable change and build on efforts to make Scotland the best place for midwives and nurses to thrive at work.
Nurses and midwives work in a wide range of health, social care and education settings across Scotland, and they are the largest group of clinicians across the country. The recommended actions are relevant for nursing and midwifery staff (registered or not, or in training) in all sectors, including NHS Scotland, social care, and academia. In essence the Taskforce takes a whole system approach to creating the nursing and midwifery workforce of the future in line with the needs of Scotland’s population.
This report concludes Phase 1 of the Taskforce and includes the rationale for the Taskforce, the ambition, the approach to information gathering, and the recommended actions. Phase 2 will involve developing a detailed workplan for implementation which will include timescales, a financial framework and sequencing of the recommended actions, as well as agreeing oversight of implementation and monitoring impact. Phase 2 also involves linking up the workplan with existing and future programmes of work (e.g. the Nursing 2030 Vision and Midwifery 2020 programme) to avoid duplication; and aligning the workplan with existing policy documents and legislation (Health and Care Staffing Act, National Workforce Strategy).
Important to note
As agreed in the terms of reference, the scope of the work of the Taskforce does not include pay or terms and conditions.
Nurses and midwives working in the health and social care sector are part of a much wider system that affect the conditions and environments in which they work and many of these are beyond the scope of the Taskforce. For example, decisions made in other sectors, such as schools, the voluntary sector, food advertising, etc. will affect patients’ expectations, demand on health care, and patient flows within the health and social care system.
The Taskforce is part of a much broader programme of work that spans the implementation of the Health and Care Staffing Act, the National Workforce Strategy, the Agenda for Change Non-pay Review and other work programmes for the wider NHS Scotland workforce. Agreement was reached early on to avoid duplication with existing programmes of work.
1.2 Why we need a Ministerial Nursing and Midwifery Taskforce
Midwives and nurses are essential to the current and future population health of Scotland. Ensuring we have the nursing and midwifery workforce to meet current and future health and social care needs must be a priority. The projected increase in care must be met, in order to achieve a continued delivery of quality of care, and to avoid nursing and midwifery staff feeling demoralised and burned out. This in turn affects staff absence levels and retention rates of nurses and midwives. Adding to this, the decline in applicants for the nursing and midwifery pre-registration programmes further emphasises the urgency to convene the Ministerial Taskforce for Nursing and Midwifery, and to implement its recommended actions.
Population health
Scotland’s demographics are changing. People are living longer with an average life expectancy of 76.9 years for men and 80.9 years for women[1]. An ageing population comes with increasing chronic conditions (heart disease, diabetes, cancers, neurological diseases). Mental health conditions are increasing, and chronic conditions are affecting people earlier in life adding to the disease burden[2]. Further challenges are presented by continued inequalities in health outcomes and exposure to risk factors that are often beyond an individual’s control (e.g. economic or climatic factors or the availability of food in a person’s area)[3]. The Scottish Burden of Disease Study forecast the future burden of disease in Scotland to increase by 21% over the next 20 years, although a third may be preventable under the right circumstances[4]. These forecasts are important for workforce and care planning design and ensuring that the skills and capability are in place to meet the shifting demands.
Changing population demographics as well as women and families’ needs and expectations also affect maternity care. Although there is a reduction in birth rates in Scotland, there is an increase in the complexity of pregnancies, driven by pre-existing medical conditions, poverty, age and complex social needs. Also, data shows inequalities in outcomes and experiences for ethnic minority women and those from more deprived areas[5,6,7,8]. The preventative public health roles of midwives and nurses are key to improving the healthy life years lived by our population, with pregnancy and the early years providing the greatest return of investment in the life course[9].
Changing care needs impacts greatly on the number of nurses and midwives required, the knowledge and skills they need to obtain, maintain, and develop, and more generally the way services are configured[10,11]. This means that nursing and midwifery roles are changing with a growing need for enhanced skills, education and training, while at the same time the workload is increasing[6].
The registered nursing and midwifery workforce Staff in post
As of September 2024, there are 74,566 qualified nurses and midwives1* with a Scottish address on the Nursing and Midwifery Council (NMC) register. This is a 1.6% increase on the previous year[12]. Registration is a requirement of practice, though the registration numbers are not a direct reflection of those currently working in Scotland.
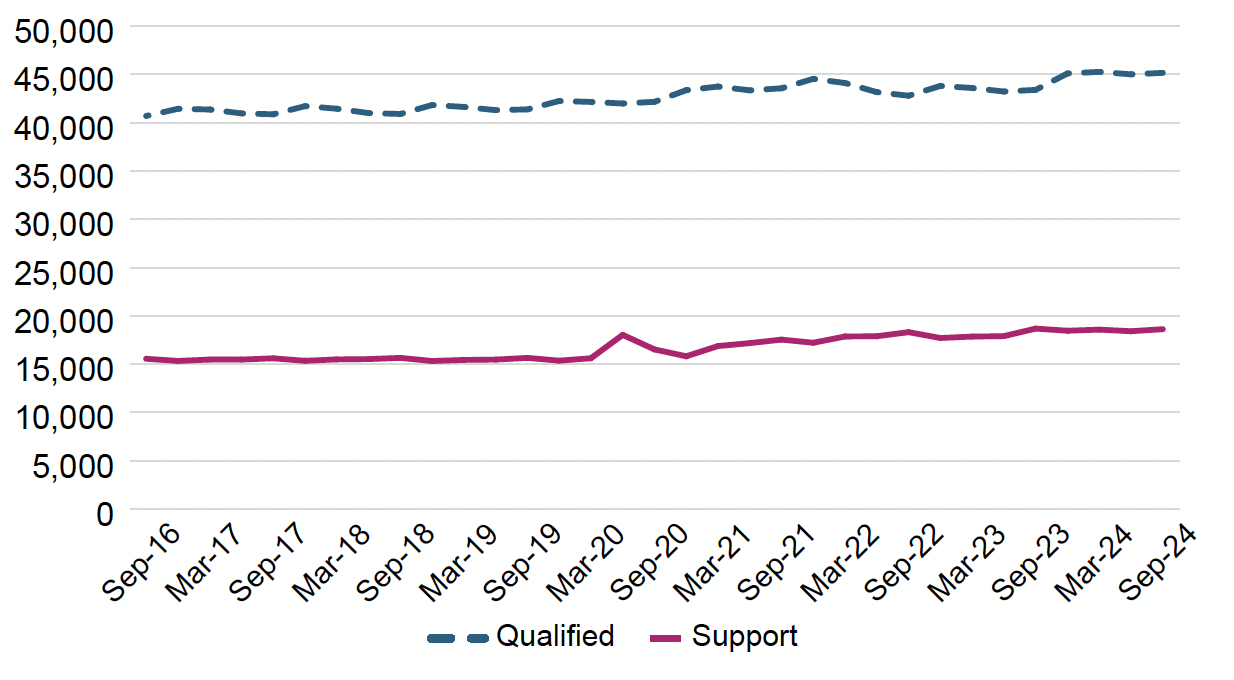
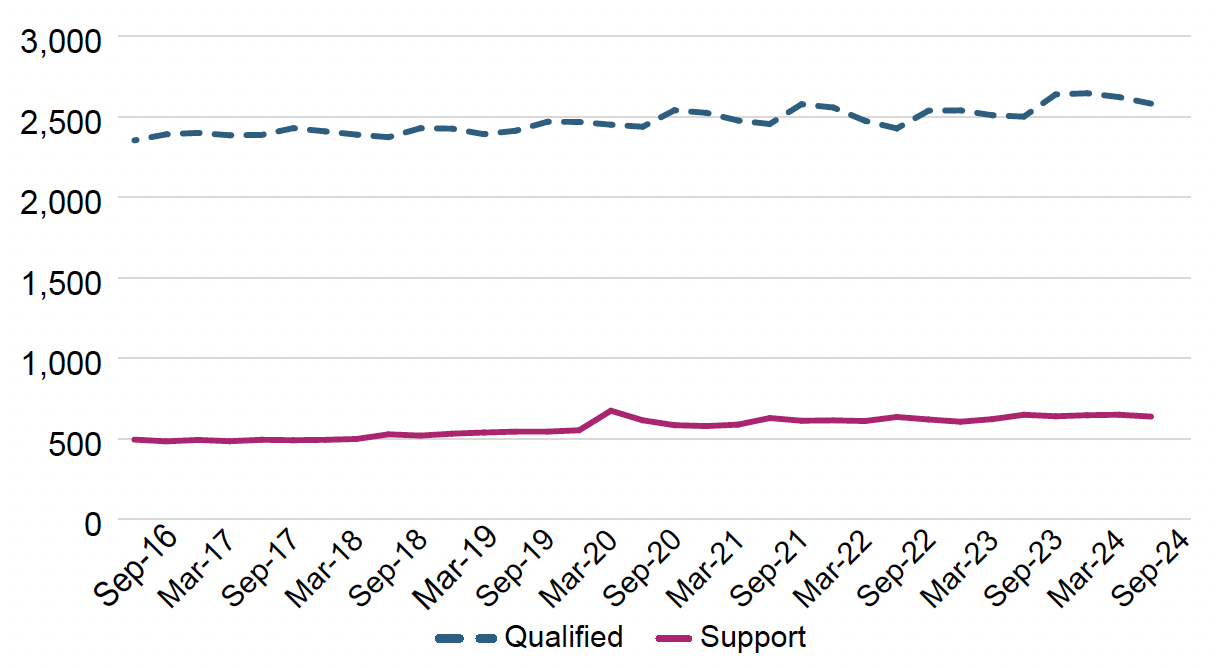
NHS Scotland is the biggest employer of these registered nurses and midwives with 51,572 (45,148.3 WTE2*) registered nurses and 3,173 (2,581.1 WTE) registered midwives as at September 2024. Over the last year this is an increase of 4.1% (1,760.1 WTE) and 3.2% (80.9 WTE) respectively. There are a further 21,939 (18,619.1 WTE) nursing support staff and 829 (637.6 WTE) midwifery support staff (see figures 1 and 2). Over the last year this is a decrease of 0.3% (-61.6 WTE) and 1.7%, (-11.3 WTE) respectively. Together nursing and midwifery staff make up 41.7% of the NHS workforce in Scotland. Of the nursing staff 88.4% are female and of the midwifery staff 99.7%[13].
1* 3,736 midwives, 70,507 nurses, 317 nurse & midwifes, 6 nursing associates.
2* WTE stands for Whole Time Equivalent. 1 WTE is equivalent to an individual working full-time.
Whilst the overall number of registrants has been steadily increasing, this increase has been uneven across professions and specialties, and across the country. For example, in table 1 it can be seen that district nursing and school nursing grew, partly due to Scottish Government commitments to support expansion of this part of the workforce, while the learning disabilities nursing workforce reduced.
Profession/nursing specialty |
Sept-16 WTE |
Sept-24 WTE |
% Change 2016-24 |
WTE change 2016- 24 |
|---|---|---|---|---|
Adult nursing |
23,702 |
24,954 |
5.3% |
1,252 |
District nursing |
2,866 |
3,290 |
14.8% |
424 |
Health visiting |
1,739 |
1,863 |
7.1% |
124 |
Learning disabilities nursing |
675 |
599 |
-11.3% |
-76 |
Mental health nursing |
6,500 |
7,087 |
9.0% |
586 |
Other |
2,873 |
4,384 |
52.6% |
1,511 |
Children and young people’s nursing / children’s nursing |
1,580 |
1,724 |
9.1% |
143 |
Public health nursing |
468 |
833 |
78.1% |
365 |
School nursing |
287 |
415 |
44.9% |
129 |
Midwifery |
2,353 |
2,581 |
9.7% |
228 |
Total |
43,043 |
47,730 |
10.9% |
4,686 |
Moreover, a growth in workforce does not mean that the distribution of staff to meet care needs is optimum.
Vacancy rates
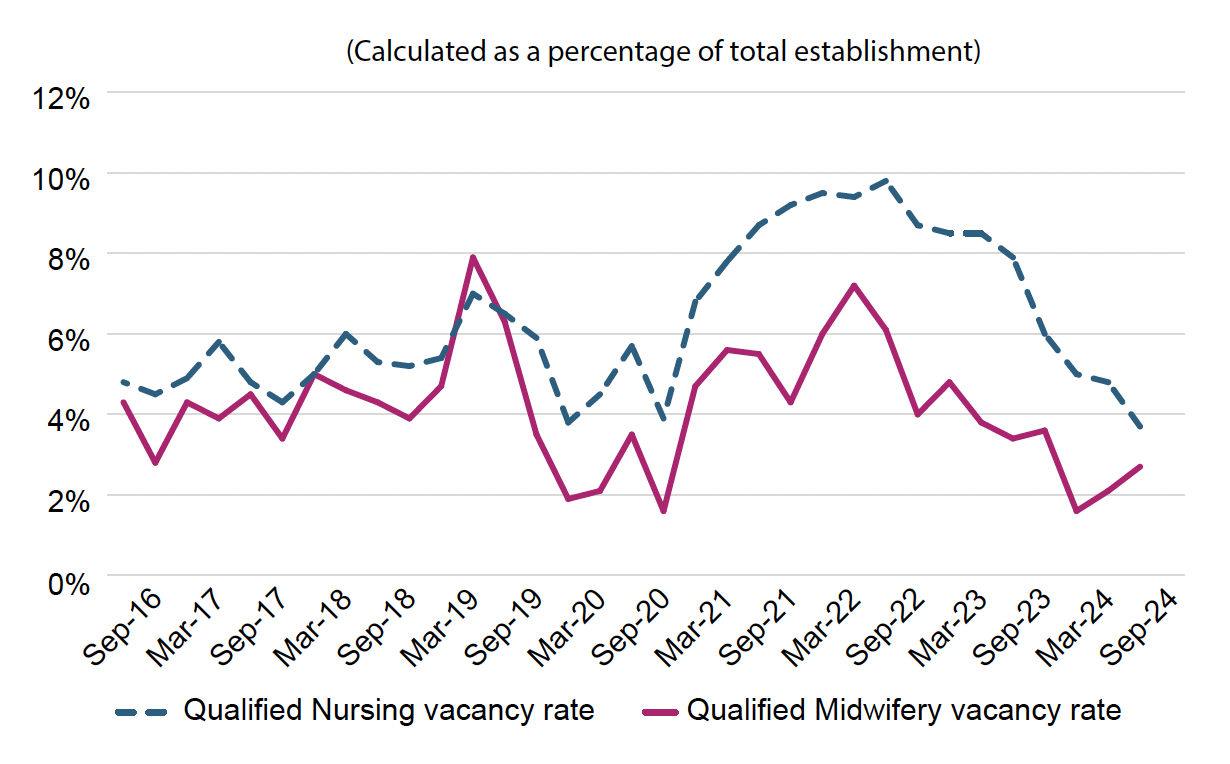
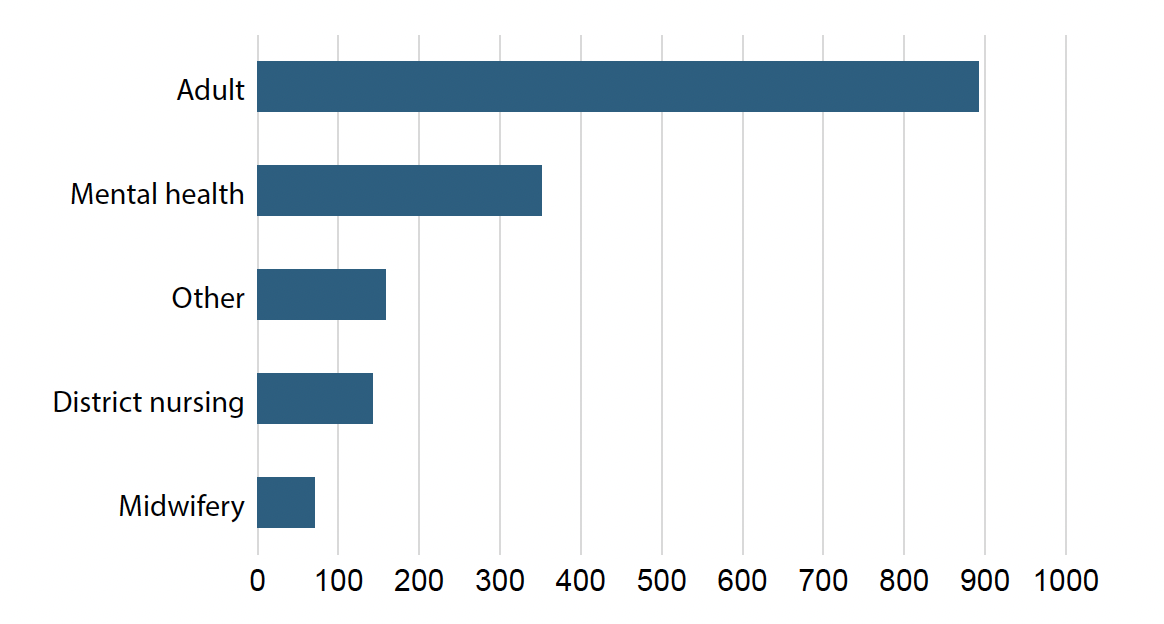
From September 2023 to September 2024 qualified nursing vacancies have decreased from 7.9% to 3.7% and qualified midwifery vacancies decreased from 3.4% to 2.7%. Adult nursing carries the most qualified vacancies (figure 4). As shown in figure 3 vacancy rates vary over time. They are affected by a combination of factors including a decreased turnover rate of nurses and midwives in the past year3*, the Covid-19 pandemic, which saw significantly increased recruitment rates, and current budgetary constraint. Implementation of the safe staffing legislation should, over time, help to identify the gaps between current establishments (that is staff in post plus vacancies) and identified workforce needed to provide safe person-centred care.
3* The turnover rate is the number of people who left divided by the total number of employees.
Leavers
While workforce data sets on nursing and midwifery are important, and especially for estimating safe and effective staffing to support improving population health, they do not contextualise the current landscape. Many workplace challenges faced by midwives and nurses are not captured by workforce data. From wider research[14,15,16,17] we know that an inadequate workplace environment can drive midwives and nurses to leave the professions. Experiencing traumatic events, poor workplace culture, inefficient IT systems and increasing expectations on the amount or variety of tasks were examples given that affect whether or not nurses and midwives feel supported and able to give the care they want to give.
For registered nursing and midwifery staff with the NMC, Scotland’s data shows that in the 12 months to March 2024, there was a 5.5% increase in the number who left the register in comparison to the previous year[12]. In addition, trends over time in the official health workforce data show that more nurses and midwives are leaving their careers at an earlier point than previously, highlighting potential gaps in the skill mix now and in the future.
Future nursing and midwifery workforce
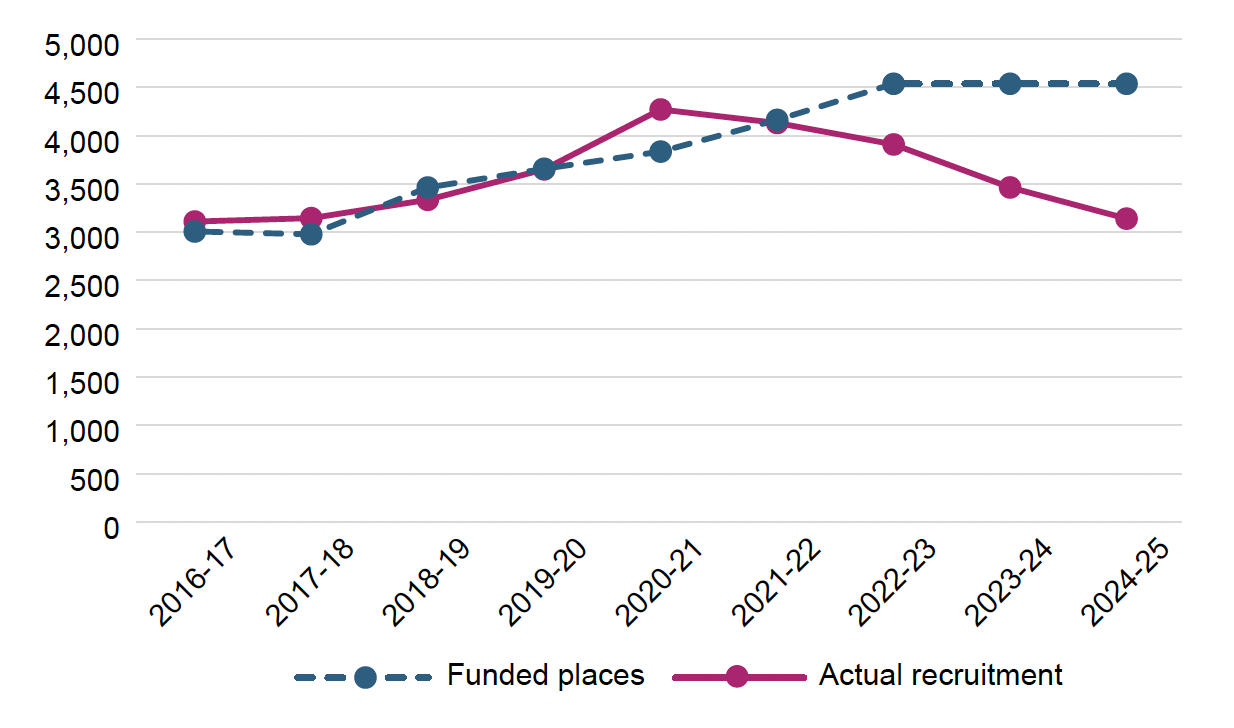
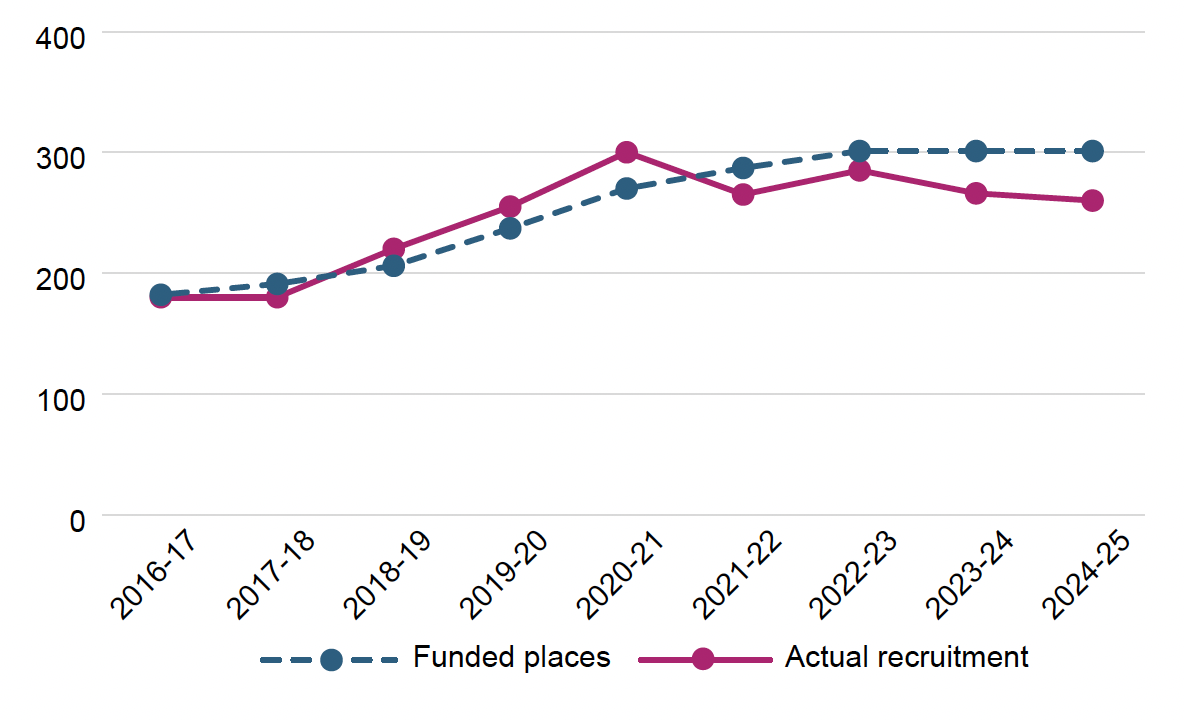
People begin a nursing or midwifery career primarily through undergraduate education programmes, with the number of training places determined by the Scottish Government after engagement with key stakeholders. Despite an increase in funded places on these programmes from 2016 until 2022, applications have declined in recent years and targets have not been met for funded places (figures 5 and 6)[18]. The decline in both nursing and midwifery applications has caused significant concern given that this is the main workforce pipeline.
The international context
When shifting from Scotland’s data to international data we see similar trends on recruitment and retention of midwives and nurses across high income countries, though most sources are based on pre-pandemic data[19,20,21]. Similarly, Scotland is not the only country seeing a drop in levels of interest to apply for undergraduate nursing post-Covid[22].
Scotland is part of a global labour market for nursing and midwifery skills. Many countries are now recruiting internationally and at a higher rate[21]. In Scotland, international recruitment has a role to play alongside domestic training routes to support safe staffing and workforce sustainability, and is bound by the Scottish Code of Practice[23] on the international recruitment of health and social care personnel, which also reflect key points from the World Health Organisation’s (WHO) Code of Practice on international recruitment[24] to protect the healthcare systems of low-income countries.
To safeguard workforce sustainability and ensure that nurses and midwives contribute to achieving universal health coverage in the best way possible, the World Health Organisation published the Global Strategic Directions for Nursing and Midwifery 2021-2025 (SDNM)[25]. The SDNM comprises policy priorities for countries in four areas: education, leadership, jobs, and service delivery, thereby highlighting that as well as addressing the clinical workforce, there is a need to focus on researchers and educators to maintain and drive forward standards of education and care. The Taskforce is drawing on the SDNM[25]and SDNM in the WHO European Region[26] to support Scotland’s ambitions of safeguarding and strengthening our nursing and midwifery workforce. Progress and implementation of the SDNM will be reported on at the World Health Assembly in 2025, emphasising the national, regional and global, importance of this work in achieving Universal Health Coverage (UHC) and population health.
1.3 The ambition of the Taskforce
The ambition of the Taskforce was agreed:
“to recognise and value the contribution of the nursing and midwifery professions in Scotland by building sustainable and skilled nursing and midwifery workforces, with attractive, varied career choices across the four pillars of practice (clinical practice, facilitation of learning, leadership, and service improvement), fair work and flexibility, where all are respected and empowered, and where staff actively choose to stay in Scotland’s Health and Social Care workforce their whole career.”
1.4 The approach of the Taskforce
To achieve the ambition identified by the Taskforce and to foster transparency, collaboration and collective leadership among the members, terms of reference were agreed. The WHO provided guidance in this initial stage and advised on the methodology, based on their experience of strengthening the global nursing and midwifery workforce[19,20]. This led to the Taskforce agreeing to develop recommended actions (to be actionable) rather than recommendations.
The Taskforce identified and agreed four key sub-themes as key areas for development:
- Attraction
- Education and Development
- Wellbeing
- Culture and Leadership
Information gathering
There were two distinct workstreams formed for the Taskforce to gather information to inform development of recommended actions. The first saw the development of four subgroups, following the sub-themes above with a further remit regarding retention. The second was a Listening Project that was designed to run concurrently with the work of the subgroups. Information from all sources has been brought together and used to develop recommended actions.
Information workstream 1: themed subgroups
The subgroups were established to examine and make recommended actions for each sub-theme. Those involved in the four subgroups were encouraged to consider retention because supporting nurses and midwives to stay in post is part of the underpinning aim of the Taskforce.
Each subgroup included representation from midwifery and nursing, see annex 1 for a list of the members and the remit of each subgroup. The subgroups met throughout the duration of the Taskforce and shared updates at the overall Taskforce meetings.
The objective for each subgroup was to consider consistent, whole system solutions required for nursing and midwifery professions now and for the future, identifying any gaps and/or areas for improvement and/or innovation.
Information workstream 2: the Listening Project
The Taskforce was committed to hearing from current nurses and midwives, students and academics from different settings and disciplines across Scotland to help shape the discussions on the recommended actions. A series of in-person and on-line engagement activities were organised under the banner of the Listening Project, which ran from August 2023 until June 2024. The Listening Project included over 80 in-person focus group discussions across Scotland and 20 online discussions. The focus of the sessions was on listening and giving space to participants to share both the positives and challenges relating to the broader working conditions which
were important to them. In addition, over 3,400 responses were received via two online surveys. Feedback was shared and discussed with the four subgroups and presented at overall Taskforce meetings. While participants raised many negative and frustrating issues, it shone through that those who took part in the Listening Project genuinely cared about the nursing and midwifery professions and the work they do. The overall Listening Project findings and key messages are published in a separate report[27].
Overview of the Listening Project engagement activities
Phase one Aug – Sep 2023
- Pulse Poll online survey (2,818 responses)
Phase two Nov 2023 – Jun 2024
- In-person focus groups across Scotland with staff (462 participants)
- National virtual focus groups with staff (122 participants)
- Free text online survey (607 responses)
Phase three Feb – May 2024
- Focus groups with students (27 participants)
- Focus groups with academics (30 participants)
1.5 Presentation of the output of the Taskforce
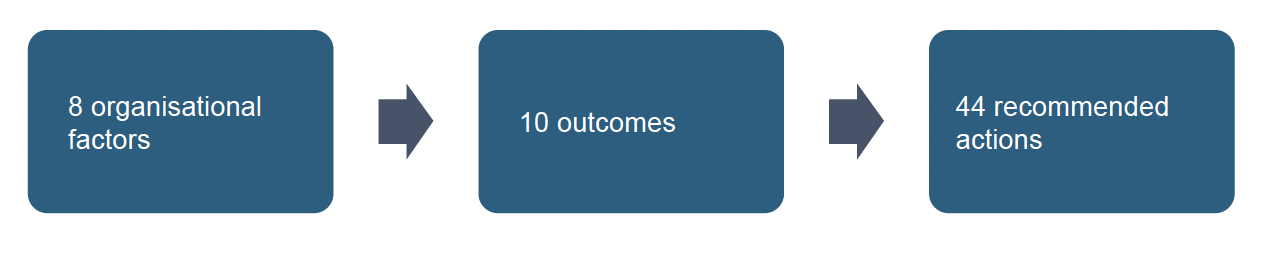
Having reviewed and analysed the supporting evidence, including the findings of the Listening Project, the four subgroups developed 44 recommended actions in support of ten key outcomes to deliver short and long-term sustainable change and build on efforts to make Scotland the best place for midwives and nurses to thrive at work.
The findings and recommended actions of the four subgroups overlapped considerably. Therefore, a framework was identified to more effectively present the 44 recommended actions and 10 outcomes. We chose to present the recommended actions by using Buchan and Catton’s review on key organisational factors for retention of nurses as a guide[21] and included Attraction as a separate factor. This means that under the following 8 organisational factors (see box) are 10 outcomes which will be delivered through the 44 recommended actions.
- Work environment and working conditions
- Flexible and work-life balance policies
- Career opportunities and access to education
- Manageable workload and safe staffing
- Productive working relationships
- Professional autonomy and participation in decision making
- Responsive management with supervision and mentoring
- Attraction
(adapted from Buchan and Catton[21])
Contact
Email: nmtlisteningproject@gov.scot
There is a problem
Thanks for your feedback