International Development Fund: non-communicable disease programme
This report responds to a commission by the Scottish Government to design a new international development health programme providing support to the governments of Malawi, Rwanda and Zambia with a focus on non-communicable diseases (NCDs).
Appraisal Case - Part 1
What impact and outcome do we hope to achieve through SG investment in NCDs in the three partner countries?
45. The SG plan to continue to invest in health in Malawi, Rwanda and Zambia, with a specific focus on the prevention and treatment of NCDs. The expected impact of the three-year programme will be increased financial and political engagement and commitment on the prevention, diagnosis of NCDs and increased access to locally led NCD quality care in Malawi, Rwanda and Zambia.
46. The outcomes of the programme will be;
a. Raised profile of NCDs as part of the UHC agenda.
b. Increased access to NCD care at district level.
c. Increased evidence on how NCDs can be integrated into existing UHC funding mechanisms.
d. Increased evidence on affordable, scalable options for NCD management in LICs.
e. Increased proportion of health care workers (HCW) able to diagnose and manage NCDs at district level.
f. Improved access to quality community based palliative care.
47. Specific programme targets will be agreed with partners on agreement and approval of the approach.
What are the feasible options that address the need set out in the Strategic Case?
48. For the purpose of this report three options have been considered.
Option 1: Do nothing. Stop health sector support to the three countries.
Option 2: Continue existing programming.
Option 3: Provide comprehensive support for NCDs at global, regional and national level, and form and participate in peer-to-peer collaborations between Scotland and the three partner countries.
Description of the options
Option 1: No SG support to the health sector in the three countries
49. This option assumes that SG will end direct support for the health sector in Malawi, Rwanda, and Zambia. This assumes that the longstanding relationships built between SG and the three partner countries will come to an end. SG development assistance is in addition to that given by the UK Government and forms an important part of SGs strategy on foreign policy and international affairs. It is likely if SG were to stop investing in health this would have broader implications for Scotland’s development objectives. In terms of NCDs, given there is currently limited support to NCDs in the three countries this will not have implications for the broader NCD agenda however Scotland’s relationship with the three countries, and in particular Malawi will likely be affected. Such an approach has a risk of significant reputational damage for Scotland with potential implications on how Scotland is viewed internationally. Given the risks of this approach it is not considered further.
Option 2: Continue with the existing SG programme and halt plans for more strategic engagement on NCDs
50. This assumes that SG continues the existing programme and ceases design efforts. SG have expressed a desire for a more strategic approach to development health spend that shares Scotland’s expertise with partner countries focusing on a narrower range of programmes, partners and topic areas. At present SG manages over 50 development contracts (7 in health, and 16 indirectly supporting health) ranging from support of a dental school, to individual support to NGOs to deliver school meals, community ear and hearing care and programmes to improve maternal and child health.[85] SG has specific interests in decolonisation and gender mainstreaming of investments, which will be much harder to achieve if the portfolio continues in its current exact form.[86] In addition, SG’s current portfolio of investments in health are wide ranging in focus and approach and are often external to government or national budgetary processes. Whilst all add value, potential impact is likely to be limited and are unable to leverage impacts potentially available through partnership and collaborative working.[87] Given the commission specifically asked for a new strategic approach to investing in health in the three countries and the limitations of the current approach in terms of impact, leverage and management this option has been discounted from further analysis.
Option 3: Set of support around NCDs with the aim of stimulating action at global, regional and national level
51. This uses SG’s political influence and position as a leader in NCDs to increase momentum towards the UN SDG goals on UHC by building partnerships at global level, both political and technical, supporting regional initiatives and targeting support at national level to scale up and roll out WHOs Regional strategy for NCDs or PEN Plus. The individual components of this approach would be:
(a) Forge political alliances with like-minded countries to raise global awareness of NCDs linking to the UHC agenda. Given the paucity of international donor investment and engagement in NCDs, there is an opportunity to work with other like-minded governments and donors to raise the profile of NCDs globally and particularly within LMICs. Potential partners to consider include those who have expressed interest in NCDs. A partnership around NCDs would raise the profile of NCDs politically including Scotland’s role in development but also have the potential to leverage additional financial resources. Potential inputs might include:
i. Work with key partners to identify opportunities to help foster dialogue around the Global NCD agenda. This might include advocacy to raise awareness of the importance of NCDs; high level dialogue or an MoU for collaboration between Scotland and like-minded partners; support for high level panels to disseminate and interrogate best practice and integration of NCDs into the UHC agenda.
ii. Joint financing of global initiatives such as the Multi-partner Trust Fund (MPTF) led by WHO.
iii. Work with partners to identify opportunities to disseminate learning on NCDs in LMICs. This may include supporting high level panels, or the organisation of conferences on NCDs as part of the roadmap towards the UN High level meeting on NCDs.
iv. Support to regional partners including potentially WHO Afro or Africa CDC as is relevant.
(b) Support the scale up of PEN PLUS in Malawi and Zambia. PEN Plus is an integrated care delivery strategy that focuses on improving access of the poorest to quality chronic care services in rural areas of LMICs. PEN Plus was adopted by Member States of the WHO African Region as the regional strategy for improving access to decentralised care for NCDs in particular Type 1 Diabetes Mellitus, Sickle Cell Disease and Rheumatic Heart Failure.[88] Treatment for these conditions is traditionally only available in tertiary level hospitals, however the barriers to accessing care by the poorest are well documented. By scaling up access to diagnosis and treatment of these relatively complex diseases that would inevitably lead to premature death and disability life expectancy for some of the poorest people will inevitably increase.[89] PEN Plus bridges the gap between training, mentoring and referral for NCDs. PEN PLUS complements the WHO PEN which aims to address less severe NCDs in health centre level, by building up capacity of nurses in district hospitals to mentor and train health centre staff providing the longer term follow up and care of NCD patients with a range of conditions.[90] Inputs include:
i. Funding the set-up of two additional PEN Plus training centres in Zambia and support to increase NCD capacity at the MoH. At present partners are working with the MoH to set up two training centres, one in Lusaka and one in the rural outskirts of the city. Two additional training centres would allow a substantial scale up in the number of HCWs trained in delivering PEN Plus, thus improving access for the poorest to services. It would accelerate ambitions in terms of dissemination of capacities to rural and harder to reach areas. In addition, support for a secondment to the Zambian MoH NCD department would build capacity of the MoH to prioritise NCD care and PEN Plus, helping to accelerate progress as per the Zambian National Health Strategic Plan 2017 They could also provide a link and feedback to the SG.
ii. Funding the delivery of PEN Plus in Malawi through support for the HSJF. The fund was established by the UK as a managed joint fund able to provide parallel financing for the Government of Malawi priorities without using their systems. Partners channel funding through it to support the Health Sector Strategic Plan of the MoH. It is the main vehicle for coordinating donor investments in the health sector in Malawi and current expenditure is around US$16m per year. The largest donor has been Norway (55%) to date followed by the UK (35%), and KFW (Germany) (7.5%). Funds are channelled through commercial bank accounts co-signed by an international Fiscal Agent with payments made directly to vendors and suppliers. Payment is in arrears on delivery of services. Procurement is via the Government of Malawi’s procurement systems but are co-approved by a contracted International Procurement Oversight Agent representing the donor partners. Overheads are shared amongst partners equally however discussions are ongoing to adjust this to reflect proportionality of investment. Governance and management arrangements are rotated amongst the partners however these are flexible and informally agreed by each of the partners. This would allow concession to be given to Scotland given its lack of country presence. At present the primary focus is on health systems and maternal and child health but discussion with donor colleagues participating in the HSJF suggest interest and willing to allow SG to use the mechanism to support finance for NCDs. By leveraging the platform, a small amount of funding has the potential to enable much wider reach than setting up a separate funding mechanism specifically to enable access to NCD services. It is also the specific request of the MoH that donors provide support through this mechanism to reduce fragmentation and to benefit from capital gains.
(c) Development of a quality community palliative care model pilot in Rwanda. Rwanda is further advanced in its implementation of PEN and PEN Plus. The MoH have asked for support for palliative care specifically. One area discussed was home based palliative care. This option would look at ways of integrating home based palliative care into the Pen and PEN Plus model as a potential pilot, building the evidence base on this approach to delivery of palliative care for those living with cancer, but also with chronic diseases that are not amenable to treatment, for example, advanced chronic kidney disease, or advanced chronic heart failure. If this model of delivery is shown to work well, research findings could potentially be used to share learning across the region on integration of community or home based palliative care into PEN and PEN Plus.
(d) Peer-to-Peer collaboration. Workshops and individual discussions with SG colleagues has flagged the interest in peer-to-peer learning and shared collaboration. This component provides two specific options for peer-to-peer learning that would operate in complement to already agreed plans around support for peer to peer learning.
i. International Association for National Public Health Institutes (IANPHI): IANPHI links and strengthens government agencies responsible for public health by leveraging the experience and expertise of its member institutes to build and improve national public health systems. At present it has 115 members in 98 countries. Public Health Scotland could join the network[91]. Examples of support that have been given by countries include use of specialist registrars to support Africa CDC with development of their strategy for NCDs. Additional support could be given to national public health institutes in the three countries potentially working in partner with other national public health institutes with a specific interest in NCDs.
ii. Support development of a regional/ national palliative care curriculum and cadre of palliative care professionals. This would involve working with colleagues from Makerere University in Uganda, Hospice Africa and linked organisations in Scotland including the University of Edinburgh etc. There are ongoing discussions about developing a programme in Rwanda, potentially with support from the Economic and Social Council (ECOSOC) of the UN through collaboration with the International Association for Hospice and Palliative Care. This might offer the opportunity to work in palliative care across the three countries, potentially linking to the development and pilot of a home-based palliative care model as above in Rwanda. It may also be possible to leverage the capacities of the NHS.
52. The proposed option benefits from the global evidence base, in particular learning through implementation of the WHO Best Buys, PEN, PEN Plus and the proposed integrated care model from the non-communicable diseases and injuries (NCDI) Poverty Commission. Figures 11-13 compare the interventions proposed in WHO Best Buys as part of the GAP with those proposed by the NCDI Poverty Commission as part of an integrated care model against the different components of the SG programme. The proposed option takes an approach more aligned to that of the NCDI Poverty Commission, supporting strengthening of the health system at district level, with a focus on diagnosis and treatment of more complex NCDs that have a disproportionate impact on the poorest. The figure also shows assumed indirect effects from the SG programme particularly by strengthening training and mentorship arrangements between district hospitals and health centres and the communities they serve. In addition, the proposed programme includes a component of increasing access to palliative care at district and community level in Rwanda.
53. The proposed option has also been audited against principles developed by the World Bank in their overview of the challenge of NCDs for SSA. Three additional principles (peer-to-peer, decolonisation and gender mainstreaming) were added from analysis of KIIs and workshops with SG colleagues.
54. Table 5 (see p.46 onwards) shows that the proposed option maps well against the audited principles. The areas where gaps emerge are specifically around comprehensive prevention given the focus on PEN PLUS however it is assumed that efforts to build capacity at district hospital level in terms of diagnosis and management of complex NCDs will build capacity for long term management of stable patients with NCDs in the medium term. The other areas where there are potential gaps are around multisectoral responses to NCDs such as working on nutrition, healthy cities, or air pollution etc. Some of these areas are already covered in national plans and strategies, or through work by WHO, so indirectly SG support for these institutions will support this. In addition, other SG work is ongoing that may well contribute to the social determinants that impact upon risk of NCDs.

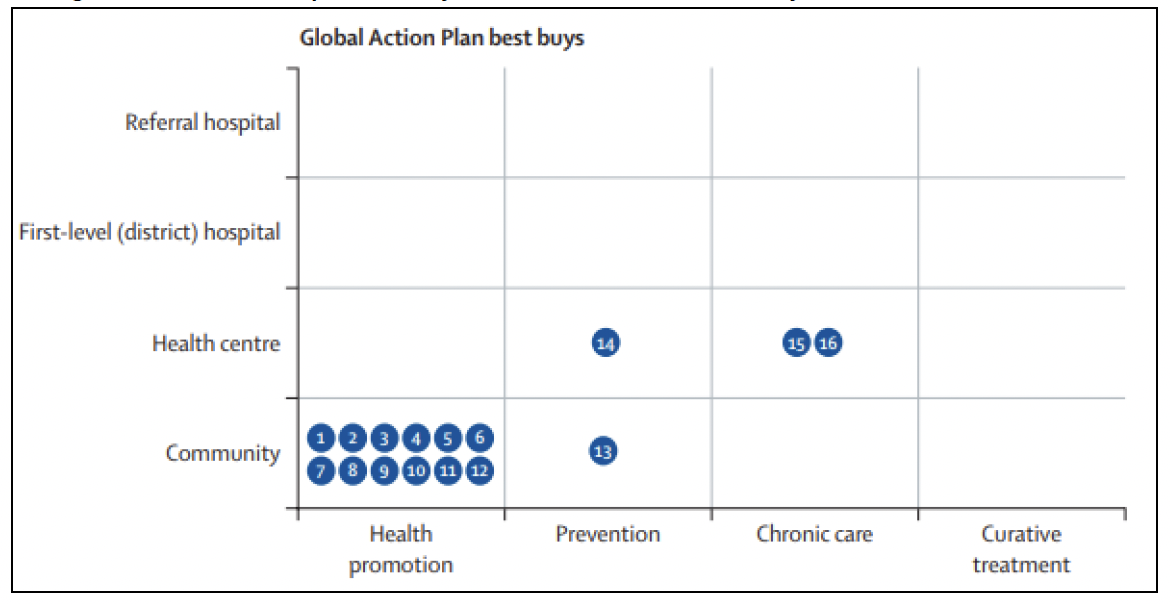
Source for Figures 11 and 12: Bukhman G. et al (2020) Lancet NCDI Poverty Commission Study Group. The Lancet NCDI Poverty Commission: bridging a gap in universal health coverage for the poorest billion. Lancet. 3;396(10256):991-1044. Permission to reproduce content secured via RightsLink.
Referral hospital |
Health promotion |
Prevention |
Chronic care |
Curative treatment |
|---|---|---|---|---|
First level (district) hospital |
32 (Malawi direct impact) 32 (Zambia direct impact) |
32 (Malawi direct impact) 32 (Zambia direct impact) |
||
Health centre |
32 (Malawi indirect impact) 32 (Zambia indirect impact) |
32 (Malawi indirect impact) 32 (Zambia indirect impact) |
32 (Malawi indirect impact) 32 (Zambia indirect impact) 34 (Rwanda direct impact) |
32 (Malawi indirect impact) 32 (Zambia indirect impact) |
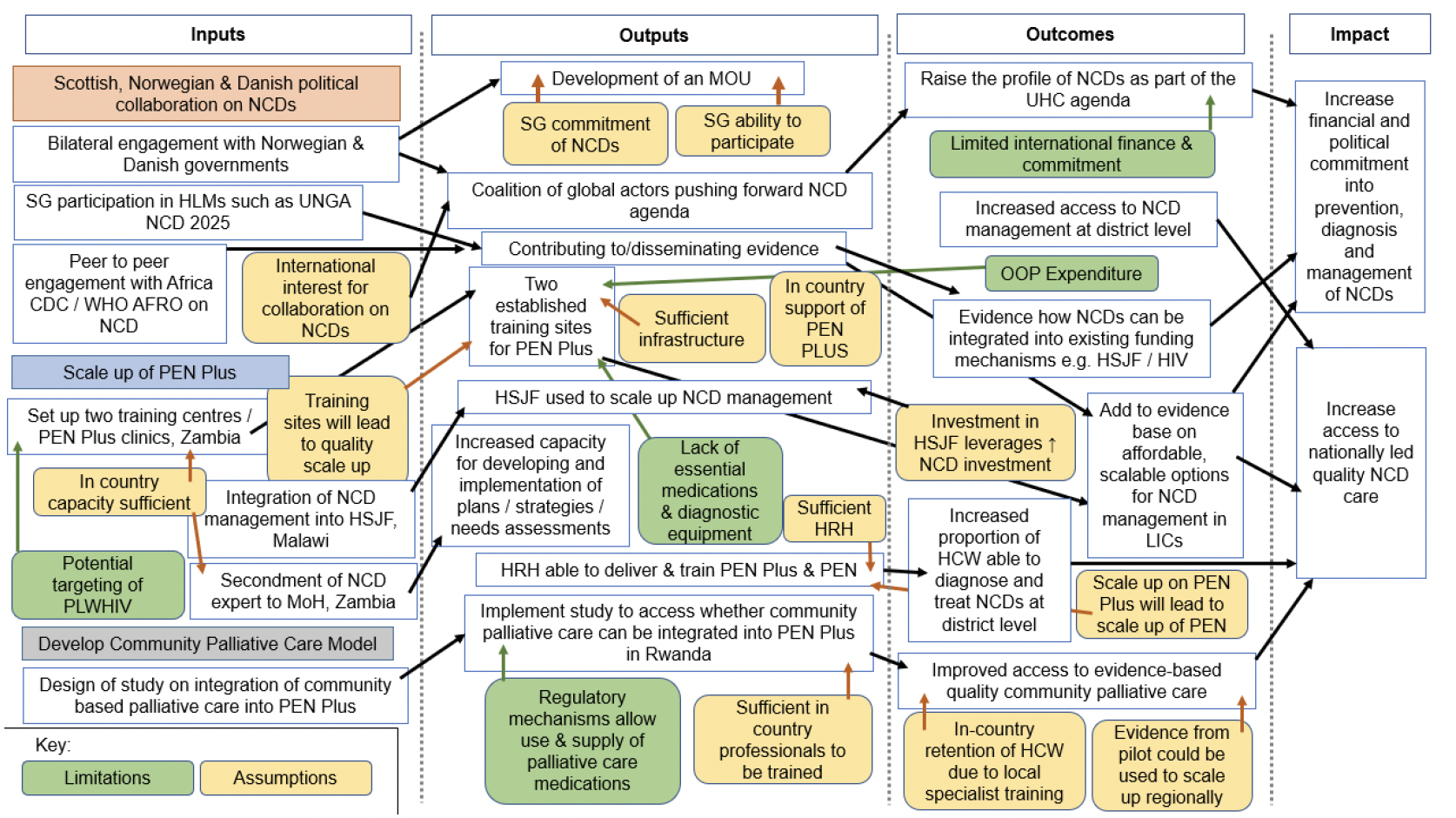
Community |
32 (Malawi indirect impact) 32 (Zambia indirect impact) |
32 (Malawi indirect impact) 32 (Zambia indirect impact) |
33 (Rwanda direct impact) 33 (Malawi indirect impact) Zambia (indirect impact) 34 (Rwanda direct impact) |
Source: Adapted from Bukhman G. et al (2020) Lancet NCDI Poverty Commission Study Group. The Lancet NCDI Poverty Commission: bridging a gap in universal health coverage for the poorest billion. Lancet. 3;396(10256):991-1044. and WHO (2017) Tackling NCDs: 'best buys' and other recommended interventions for the prevention and control of noncommunicable diseases
Table 2: Key for Figure 11[92]
Number 1
Intervention: Mass media messages concerning healthy eating or physical activity
Number 2
Intervention: Mass media messages concerning use of tobacco and alcohol
Number 3
Intervention: Mass media for awareness on handwashing and household air pollution health effects
Number 4
Intervention: Education campaigns for the prevention of gender-based violence
Number 5
Intervention: School-based HPV vaccination for girls
Number 6
Intervention: Opportunistic screening for cervical cancer using visual inspection or HPV DNA testing and treatment of precancerous lesions with cryotherapy
Number 7
Intervention: Treatment of acute pharyngitis in children to prevent rheumatic fever
Number 8
Intervention: Low-dose inhaled corticosteroids and bronchodilators for asthma and for selected patients with COPD
Number 9
Intervention: Screening and management of diabetes among adults at risk, including glycaemic control, management of blood pressure and lipids, and consistent foot care
Number 10
Intervention: Prevention of long-term complications of diabetes through blood pressure, lipid, and glucose management as well as consistent foot care
Number 11
Intervention: Screening and management of diabetes in pregnancy (gestational diabetes or pre-existing type 2 diabetes)
Number 12
Intervention: Basic palliative care
Number 13
Intervention: Long-term management of ischaemic heart disease, stroke, and peripheral vascular disease with aspirin, beta blockers, ACEi, and statins (as indicated) to reduce risk of further events
Number 14
Intervention: Opportunistic screening for hypertension for all adults and initiation of treatment among individuals with severe hypertension or multiple risk factors
Number 15
Intervention: Screening and management of hypertensive disorders in pregnancy
Number 16
Intervention: Management of depression and anxiety disorders with psychological and generic antidepressant therapy
Number 17
Intervention: Management of epilepsy, including acute stabilisation and long-term management with generic anti-epileptics
Number 18
Intervention: Management of acute exacerbations of asthma and COPD using systemic steroids, inhaled beta-agonists, and, if indicated, oral antibiotics and oxygen therapy
Number 19
Intervention: Basic palliative care
Number 20
Intervention: Secondary prophylaxis with penicillin for rheumatic fever or established rheumatic heart disease
Number 21
Intervention: Medical management of acute heart failure
Number 22
Intervention: Medical management of heart failure with diuretics, beta blockers, ACEi, and mineralocorticoid antagonists
Number 23
Intervention: Provision of aspirin for all cases of suspected myocardial infarction
Number 24
Intervention: Management of schizophrenia using generic anti-psychotic medications and psychosocial treatment
Number 25
Intervention: In settings where sickle cell disease is a public health concern, universal newborn screening followed by standard prophylaxis against bacterial infections and malaria
Number 26
Intervention: Detect early-stage breast cancer using clinical examination and refer for treatment
Number 27
Intervention: Early detection and treatment of early-stage cervical cancer
Number 28
Intervention: Basic first-level hospital surgical services
Number 29
Intervention: Treat early-stage breast cancer with appropriate multimodal approaches, including generic chemotherapy, with curative intent, for cases that are referred from health centres and first-level hospitals following detection using clinical examination
Number 30
Intervention: Treat selected early-stage childhood cancers with curative intent in paediatric cancer units or hospitals
Number 31
Intervention: Specialised surgical services
Table 3: Key for Figure 12[93]
Number 1
Intervention: Increase excise taxes and prices on tobacco products
Number 2
Intervention: Enact and enforce comprehensive bans on tobacco advertising, promotion, and sponsorship
Number 3
Intervention: Implement plain or standard packaging and large graphic health warnings on all tobacco packages
Number 4
Intervention: Eliminate exposure to second-hand smoke
Number 5
Intervention: Implement effective mass media campaigns that educate the public about the harms of smoking or tobacco use and second hand smoke
Number 6
Intervention: Increase excise taxes on alcoholic beverages
Number 7
Intervention: Enact and enforce bans or comprehensive restrictions on exposure to alcohol advertising
Number 8
Intervention: Enact and enforce restrictions on the physical availability of retailed alcohol
Number 9
Intervention: Reduce salt intake through reformulation of food products to contain less salt
Number 10
Intervention: Reduce salt intake through establishment of a supportive environment in public institutions
Number 11
Intervention: Reduce salt intake through behaviour change communication and mass media campaign
Number 12
Intervention: Reduce salt intake through implementation of front-of-pack labelling
Number 13
Intervention: Implement community-wide public education and awareness campaign for physical activity
Number 14
Intervention: Vaccination against HPV
Number 15
Intervention: Prevention of cervical cancer through screening and treatment
Number 16
Intervention: Drug therapy and counselling to individuals who have had a heart attack or stroke or who are at high risk of a fatal or non-fatal cardiovascular event in the next 10 years
Table 4: Key for Figure 13
Number 32
Intervention: Support the scale up of PEN-Plus in Malawi and Zambia
Number 33
Intervention: Development of quality community palliative care model pilot in Rwanda
Number 34
Intervention: Peer-to-peer collaboration
Principle |
Principle definition |
Forge political alliances linking NCDs to UHC |
Support the scale up of PEN PLUS in Malawi |
Support the scale up of PEN PLUS in Zambia |
Pilot community palliative care, Rwanda |
P2P IANPHI |
P2P palliative care training |
|---|---|---|---|---|---|---|---|
Multisectoral response |
Mobilize a multisectoral response to build support and capacity |
X |
X |
X |
|||
Partnership and Ownership |
Establish effective partnerships and promote civil society engagement, broad participation, and ownership |
X |
X |
X |
X |
X |
X |
Evidence based |
Select cost-effective and evidence-based approaches, and use and build an evidence base, with investment in research |
X |
X |
||||
Stepwise and prioritise |
Implement priority interventions according to potential for health gains, local considerations, and need |
X |
X |
X |
X |
X |
|
Integration |
Take account of common risk factors, determinants, and care models across diseases, and promote integration where it adds value and/or saves costs |
X |
X |
X |
X |
||
Comprehensive prevention |
Balance a combination of population-level primary prevention and individual health care strategies |
X |
X |
||||
Life Course |
Promote prevention throughout life, beginning in early life and continuing with interventions for adults and the elderly |
X |
X |
X |
X |
X |
X |
Health system strengthening |
Reorient and strengthen health systems, in particular primary health care, striving for universal coverage and fairness in resource allocation |
X |
X |
X |
X |
||
Enabling and empowering |
Enable and empower people with NCD and their families to manage their conditions better |
X |
X |
X |
|||
Equity |
Promote equity, taking account of social and environmental determinants |
X |
X |
X |
X |
X |
X |
Evaluation and accountability |
Strengthen surveillance, monitoring, evaluation, and information-sharing to increase accountability and target effort and resources more effectively |
X |
X |
X |
|||
Development |
Integrate with national programs for sustainable development, and ensure consistency with national health policy and existing programs |
X |
X |
X |
X |
X |
X |
Peer to Peer |
Mutual learning and training strategy that involves participants of the same level engaging in collaborative learning. |
X |
X |
X |
X |
||
Decolonisation |
Take a decolonised/BLM lens on investments, supporting shift power South |
X |
X |
X |
X |
||
Gender Mainstreaming |
Putting the rights and empowerment of women and girls and other marginalised groups at its heart, in a manner that has a practical impact. |
X |
X |
X |
X |
Assessing the strength of the evidence base for each feasible option
55. The evidence base on investing in NCDs is LMICs is small but growing. Table 7 outlines the main assumptions explored as part of the report and the source and quality of evidence found that supports these areas. This section does not provide a detailed overview of the evidence, as this has been incorporated into the formation of the report. The definition of quality of evidence is explained in Table 6.
Certainty |
What it means |
|---|---|
Very low |
The true effect is probably markedly different from the estimated effect |
Low |
The true effect might be markedly different from the estimated effect |
Moderate |
The authors believe that the true effect is probably close to the estimated effect |
High |
The authors have a lot of confidence that the true effect is similar to the estimated effect |
Theory of change
56. The programme seeks to increase global, and national attention to NCDs by working with partners to leverage finance and capacities in support of the NCD agenda at country level. The focus will be on engaging international partners and raising awareness in advance of the UN High Level meeting on NCDs. In addition, it will support the scale up of PEN Plus in Malawi and Zambia by focusing on training of health workers or making available services using existing platforms to build upon thus maximising scope and scale of the interventions. In Rwanda, priority will be given to exploring opportunities to integrate community palliative care on the backbone of an existing PEN Plus network and on creating training programmes for palliative care for the country and region under the leadership of the MoH. Peer-to-peer support will form a major component of the work, whether public health capacity and links or using specific NCD related clinical capacities and linkages via the Royal Colleges as appropriate. The programme builds upon lessons learned through existing policies and programmes such as the GAP, and programmes run by MoH and partners in the three countries. This can be seen in Table 7.
57. The Theory of Change (ToC) has several implicit assumptions built in (see Figure 14):
a. That UHC will not be achieved without increased action on NCDs. Given the existing and future burden of NCDs, it is unlikely that targets on UHC will be met without accelerated focus on NCDs.
b. That countries are keen to partner with Scotland on this important agenda and that the global system will be able to absorb the agenda into current health security focused frameworks. COVID-19 showed the importance of tackling NCDs, given the heightened risk of COVID-19 for those suffering from an NCD but also increased risk of developing an NCD following infection. In addition, services for those with NCDs collapsed as a consequence of the focus given to COVID during the pandemic.
c. That SG has the capacity to engage with global partners on the issue of NCDs.
d. That SG has the capacity to engage with country partners in the design and implementation of the programme despite an absence of country presence (this might include discussions around budget support in Rwanda).
e. That SG stakeholders will be comfortable with a shift in approach away from a programme explicitly designed around women and children, to one that is more heterogenous in the population it supports but that includes children and the poorest more broadly.
f. That partners at country level including those involved in the HSJF are willing for its remit to be expanded to include a focus on NCDs and that this leads to expanded access to services for NCDs.
g. There are sufficient health workers, infrastructure and commodities to allow training on PEN Plus to be rolled out in Zambia.
h. There are sufficient health workers, infrastructure and commodities to allow roll out of PEN Plus as part of the HSJF in Malawi.
i. That the MoH and partners can design and roll out a pilot on palliative care as part of PEN Plus.
j. That Scottish partners can provide capacity to enable robust peer-to-peer networks to be formed and tailored in a way appropriate to the country contexts.
k. That scale up of PEN Plus will lead to scale up of PEN.
Table 7: Strength of evidence for strategies / interventions
Statement: NCDs should be invested in at global level
Strength: High
Sources:
WHO observatory data
Global Burden of Disease studies
Lancet NCDI poverty commission: Bridging a gap in Universal Health Coverage for the poorest billion
Summary: There is strong evidence articulating the burden of disease from NCDs globally.
Statement: There are evidence-based interventions for the prevention and management of NCDs
Strength: High
Sources:
WHO Best buys
Summary: This forms the evidence-based framework for investing in NCDs. This is a global level strategy, so some recommendations may be less relevant for specific countries however it is the framework used to inform progress towards the SDGs.
Statement: There is a link between poverty and NCDs
Strength: High
Sources:
Lancet NCDI poverty commission: Bridging a gap in Universal Health Coverage for the poorest billion
Summary: There is clear evidence on the link between poverty and NCDs, including the policy gap between global recommendations and interventions and the NCD needs of those living in the poorest billion.
Statement: Supporting NCDs will support the poorest
Strength: Low
Sources:
Lancet NCDI poverty commission: Bridging a gap in Universal Health Coverage for the poorest billion
Summary: Although there is no direct evidence, extrapolating from Ethiopia and Rwanda, support of decentralised models of primary health care can reach the poorest if designed appropriately (evidence for maternal and child health).
Statement: NCDs should be invested in in Malawi, Rwanda & Zambia
Strength: Medium
Sources:
WHO observatory data
Global Burden of Disease studies
MoH Strategic Plans from Malawi, Rwanda and Zambia
MoH NCD Plans from Malawi and Rwanda
STEPS survey from Malawi, Rwanda and Zambia (all outdated)
Summary: National data is available based on modelled estimates from the Global Burden of Disease. In country data from surveys is available but support is needed to refresh it. In addition, support and advocacy is needed to integrate NCD indicators into the DHIS and HMIS.
Statement: Political partnerships will leverage support in NCDs
Strength: Medium
Sources:
Mid-point evaluation of the implementation of the WHO global action plan for the prevention and control of noncommunicable diseases 2013–2020
Summary: The mid-point evaluation of the GAP for NCDs shows it has raised the profile of NCDs and improvement in some indicators, however, outcomes and impact not yet assessed.
Whilst not directly related, experience from HIV, TB, Malaria, family planning, maternal and child health and from global policies such as the MDGs and SDGs shows the potential impact political and other alliances can have in raising awareness of a set of disease conditions. By working in partnership, the potential for impact is maximised.
Statement: Pooled funds should be utilised for NCD investment
Strength: Medium
Sources:
Annual reviews and Project Completion reports on impact from development assistance for health and pooled funds.
Anecdotal reports on benefits for Governments and MoH.
Summary: SWAp and Pooled Funds have been used in the health sector in many regions successfully, reducing overheads for participants.
Statement: Direct investment in PEN improves NCD care
Strength: Low to Medium
Sources:
Global Strategy on WHO PEN
Summary: PEN is a global strategy that sets out recommendations on scale up of interventions for NCDs at health centre and community level. Whilst this is gold standard guidance, evidence on implementation is more limited, as is evidence on effectiveness of interventions on the health of the poorest.
There is a severe lack of data on roll out of PEN in the three countries of focus for SG or indeed LLMICs more broadly.
Anecdotal evidence from interviews suggests that the focus on the health centre level has slowed down implementation due to the sheer numbers of health workers needed to be trained and due to lack of access to basic diagnostics and treatments.
Statement: Direct investment in PEN PLUS improves NCD care
Strength: Medium
Sources:
PEN-Plus – A regional strategy to address severe NCDs at first-level referral health facilities.
Lancet NCDI poverty commission: Bridging a gap in Universal Health Coverage for the poorest billion
Summary: PEN Plus is the regional strategy adopted by MS in the WHO Africa region to improve NCD care in SSA. This is supported in the Lancet NCDI poverty commission on bridging the gap for the poorest billion, where they present evidence on integrated models of care. In addition, there were detailed discussions on this in a recent conference on PEN Plus and NCDs in Rwanda, where Rwanda and Malawi shared their experience of scaling up PEN Plus.
Statement: Investment in PEN Plus will lead to spill over benefits for scale up of PEN at health centre level
Strength: Low
Summary: Little to no evidence that spill over from PEN Plus to PEN will take place. Evidence on this needs to be collected.
Statement: Community based palliative care will integrate well into PEN Plus
Strength: Low
Summary: Community based palliative care used to be an important component of HIV management prior to scale up of ARVs. There is no evidence on how this model might be used for NCDs as part of PEN Plus, but the Rwandan government is keen to explore community based models of care. Work with partners including those at Harvard and Partners in Health could help pilot this approach and disseminate learning.
Statement: Peer-to-Peer support for NCDs will support partner countries to develop palliative care training programmes and models of care
Strength: Medium
Summary: Evidence on use of peer-to-peer approaches to build capacity and scale up NCD care is low and mainly anecdotal e.g., role of the Department of Health and social care in providing capacity to Africa CDC to support development of their regional strategy on NCDs via IANPHI or on links between Royal Colleges and country medical training systems to allow use of accreditation systems and processes. However, learning can be taken from other disease areas, and the use, approach, and impact of peer-to-peer programmes such as THET, VSO, and other collaborations.
Contact
Email: socialresearch@gov.scot
There is a problem
Thanks for your feedback