Setting the Table Guidance
Nutritional Standards and Practical Guidance for Early Learning and Childcare Providers in Scotland. Childcare services providing food and/or drinks to children 0-5 years, and are registered with Care Inspectorate, will be responsible for the implementation of this guidance.
2 Guidance from birth to 1 year
2.1 Feeding babies in the first year of life
Babies from birth to 1 year of age have different nutrition and feeding requirements to children over 1 year. It is important to talk to parents and carers regularly about the feeding needs and preferences of their baby, including any allergies they may have. It is also important to recognise cultural differences and discuss any specific requirements with parents and carers in a sensitive way. Section 4 provides information on meeting the needs of all children.
Feeding patterns and needs
In the first year of life, babies follow individual feeding and sleeping patterns that can regularly change. Childcare settings should ask parents and carers about their baby’s current pattern.
These patterns should be kept consistent and should be part of the baby’s care plan each day, wherever possible. A baby feeding checklist is a useful tool to support these discussions.
Discussing feeding patterns and specific requirements, such as allergies, with parents and carers is important. Look at the baby feeding checklist to help you.
Equipment and facilities
When providing care for babies, it is important to consider the environment and equipment you will need for feeding. It is especially important to provide a supportive environment to encourage and enable mothers to continue breastfeeding.
The equipment you will need will depend on the needs of the babies in your care and whether they are breast-fed or formula-fed.
Some important points to consider include:
- If a mother wants to breastfeed, do you have a quiet space with a comfortable chair? A comfortable chair for practitioners when bottle feeding is important too.
- If parents are providing expressed breast milk, do you have a fridge which is maintained at 0-4°C to store the breast milk and labels to write the baby’s name?
- Do you have a fridge thermometer to regularly check the fridge is operating at the correct temperature?
- If you are making up formula feeds in a bottle, do you have all the sterilising equipment you need?
- If parents provide solid foods, do you have appropriate storage facilities and labels to write the baby’s name?
- When introducing solid foods, do you have a suitable highchair with secure straps, and a foot rest to ensure the baby is sitting safely in an upright position to allow them to swallow properly?
- Do you have suitable equipment such as small bowls and free flow cups (without a valve)? Remember soft spoons are gentler on gums.
! Always use a highchair with a securely fitted harness, and a foot rest to ensure the baby is sitting safely in an upright position to allow them to swallow properly. Never leave babies unattended on raised surfaces or when feeding.
Introducing a baby to solid foods sometimes called complementary feeding or weaning, should start when a baby is around 6 months old.
Providing feedback to parents and carers
Feedback is important to make sure parents and carers know what food and drink their baby has had whilst in your care, and to support a variety of foods being offered both at home and in the childcare setting.
A daily feeding diary is a useful way to keep a record of feeding patterns and can be shared with parents and carers. It is also important for parents and carers to be made aware of any changes in feeding patterns you observe.
At the end of the day the daily feeding diary could be shared with parents and carers.
Feeding expressed breast milk and infant formula milk
Practitioners should be aware of the signs (feeding cues) a baby will show when they are hungry and feed them responsively according to their needs. You should look for feeding cues such as their mouth opening, puckering, smacking their lips, or turning their head towards the bottle. The Parent Club website provides further information on feeding cues.
Having a big feed does not mean a baby will go longer between feeds, so try not to encourage them to take on a bit more than they want for this reason. This can lead to them overeating.
Babies may take more milk during one feed than they do at another. As solid food is introduced, and babies adapt to larger quantities of solid food, they will gradually take less milk.
Babies who are bottle-fed with expressed breast milk or infant formula milk, or fed breast milk from a cup, should be held close in a semi upright position. If being bottle-fed, encourage them to draw the teat into their mouth. You should give babies eye contact and speak soothingly to them throughout feeds. Whenever possible, a baby should be fed by the same person at each feed, as this supports their emotional needs.
! Babies should never be left alone with a bottle and neither the baby nor the bottle should be propped up. Propping up the bottle is dangerous, as babies may choke, and it does not support their emotional needs.
! Always test the temperature of the milk on the inside of your wrist before feeding, it should feel slightly cool.
Babies normally feed in bursts of sucking, with short pauses to rest before starting to suck again. Never force a baby to finish a feed if they seem to be full. Signs to look out for that they may have had enough include: milk spilling out of their mouth; closing their mouth or their head turning away; splayed fingers and toes; and pushing the bottle away in an older baby.
Overfeeding could upset their tummy, make them vomit or gain weight too quickly. Responsive or paced feeding means feeding whenever a baby shows signs that they are hungry, feeding at their own pace and using the cues that they are full.
! Always discard any unused expressed breast milk or infant formula milk that is left in the bottle after feeding. The combination of milk and baby’s saliva can cause bacteria to grow. The milk in unused bottles should be discarded if it has been kept at room temperature for over two hours.
Only expressed breast milk or infant formula milk should be provided in a baby’s bottle. Adding solid food, such as cereal or sugar, to bottles is not recommended because they may not be developmentally ready for solid food. There is also the potential to overfeed, and it has a negative impact on oral health.
Further useful information can be found in Public Health Scotland’s Off to a good start: all you need to know about breastfeeding and Formula feeding: How to feed your baby safely publications as well as the Parent Club website.
Daily feeding diary example
The following diary example is a useful tool to inform parents and carers of key points about their baby’s feeding each day. It can be adapted to meet the needs of the provider and babies.
| Baby’s name | |
| Date | |
| Your baby had milk today (If baby is mixed fed you may want to specify whether breast milk or infant formula milk was provided) | at_____________ o’clock and took __________________ ml Add in additional lines as required |
| Your baby had food today | at_____________ o’clock and ate __________________ Add in additional lines as required |
| Your baby has been | Record any relevant information in relation to feeding e.g., did baby seem satisfied/settled with feeds, were they sick/ windy? |
Additional information (e.g. water provided to formula fed babies) |
Baby feeding checklist example
The following checklist example is a useful tool to support discussions with parents and carers around their baby’s feeding patterns. It can also form part of any care plan that you develop for the baby and should be updated regularly. It can be adapted to meet the needs of the provider and babies.
| What to check on | Yes | No | Notes |
|---|---|---|---|
Breastfeeding
|
|||
Formula feeding
|
|||
Solid foods
|
|||
Food allergies/ intolerances
|
|||
Are any foods avoided/ preferred? e.g. vegetarian/ cultural |
|||
| Is water given? |
2.2 Breastfeeding
Encouraging breastfeeding is a national priority in Scotland, and breast milk is the ideal food for babies. The World Health Organization’s recommendation is for babies to be exclusively breastfed for the first 6 months of life and the Scottish Government has adopted this recommendation.
Breast milk provides all the energy and nutrients a baby needs during this time. It also helps to protect against infection and supports the development of a close and loving relationship with the mother. However, all babies receiving breastmilk should have an additional vitamin D supplement. Babies consuming more than 500ml of infant formula milk do not need a vitamin D supplement.
Breastfeeding should continue beyond the age of 6 months, alongside the introduction of appropriate types and amounts of solid foods, for up to 2 years of age or for as long as mother and baby wish. Public Health Scotland provides further information on the health benefits of breastfeeding for both mother and baby. The Parent Club website provides advice and information to help mothers navigate any challenges around breastfeeding.
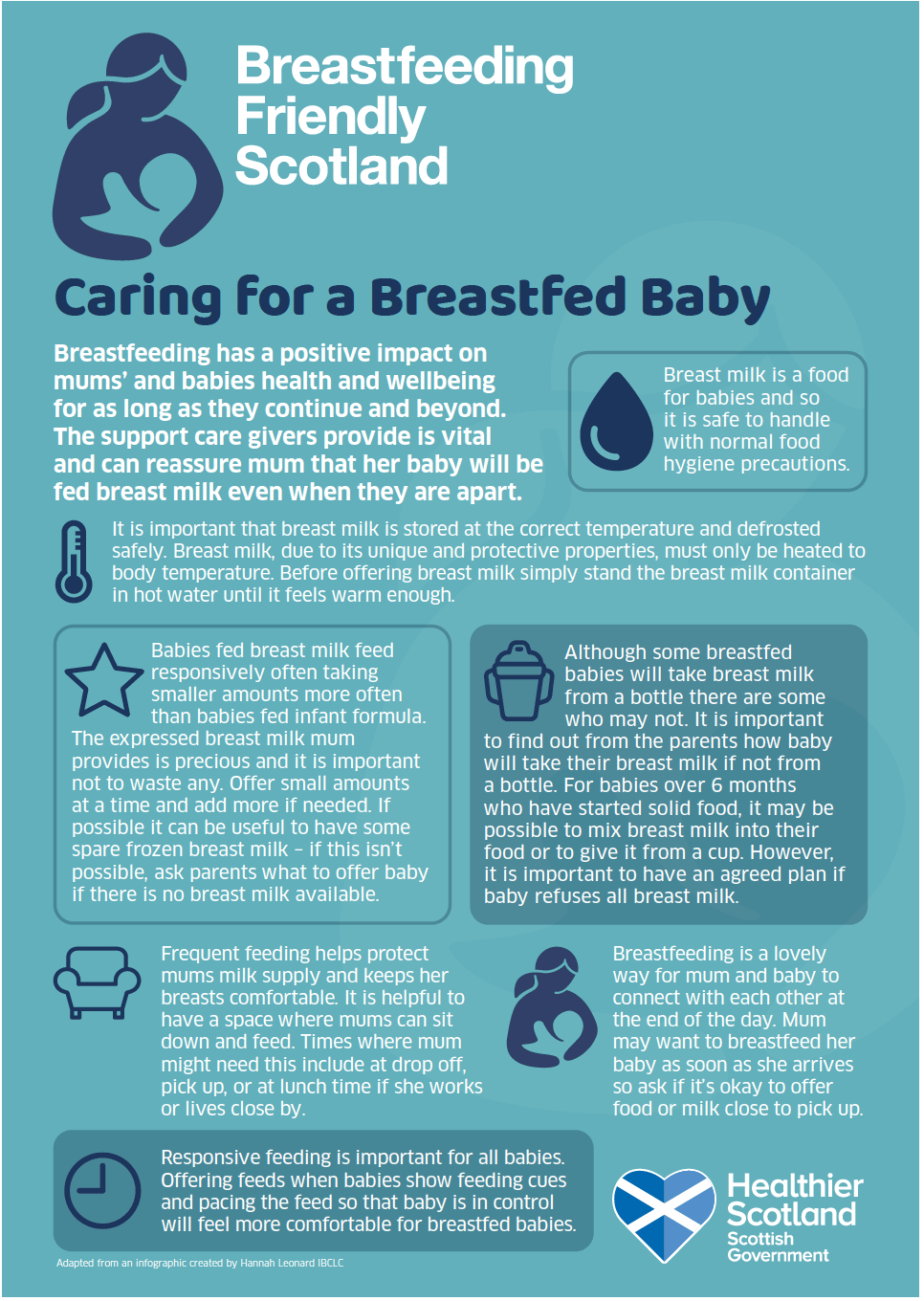
Graphic text below:
Caring for a Breastfed Baby
Breastfeeding has a positive impact on mums’ and babies health and wellbeing for as long as they continue and beyond. The support care givers provide is vital and can reassure mum that her baby will be fed breast milk even when they are apart.
Breast milk is a food for babies and so it is safe to handle with normal food hygiene precautions.
It is important that breast milk is stored at the correct temperature and defrosted safely. Breast milk, due to its unique and protective properties, must only be heated to body temperature. Before offering breast milk simply stand the breast milk container in hot water until it feels warm enough.
Babies fed breast milk feed responsively often taking smaller amounts more often than babies fed infant formula. The expressed breast milk mum provides is precious and it is important not to waste any. Offer small amounts at a time and add more if needed. If possible it can be useful to have some spare frozen breast milk – if this isn’t possible, ask parents what to offer baby if there is no breast milk available.
Although some breastfed babies will take breast milk from a bottle there are some who may not. It is important to find out from the parents how baby will take their breast milk if not from a bottle. For babies over 6 months who have started solid food, it may be possible to mix breast milk into their food or to give it from a cup. However, it is important to have an agreed plan if baby refuses all breast milk.
Frequent feeding helps protect mums milk supply and keeps her breasts comfortable. It is helpful to have a space where mums can sit down and feed. Times where mum might need this include at drop off, pick up, or at lunch time if she works or lives close by.
Breastfeeding is a lovely way for mum and baby to connect with each other at the end of the day. Mum may want to breastfeed her baby as soon as she arrives so ask if it’s okay to offer food or milk close to pick up.
Responsive feeding is important for all babies. Offering feeds when babies show feeding cues and pacing the feed so that baby is in control will feel more comfortable for breastfed babies.
Adapted from an infographic created by Hannah Leonard IBCLC
Many mothers using childcare may wish to continue providing breast milk for their babies. Some mothers may have already returned to work and will provide you with expressed breast milk for their baby during the day. Mothers who work nearby may plan to come to the setting to breastfeed their baby during their breaks, and this should be encouraged.
Your knowledge of the importance of continued breastfeeding, and how to store, prepare and feed expressed breast milk, will reassure mothers and will be welcomed. You can help by offering comfortable, warm and appropriate facilities for breastfeeding mothers and by encouraging them to continue providing expressed breast milk. Further information on providing a supportive environment to encourage breastfeeding is provided later in this section.
If a mother provides expressed breast milk for her baby while in your care, it is important to be aware of current guidance on how to store and heat the milk.
Transportation and storage of expressed breast milk
Expressed breast milk should be:
- Transported to the setting in a cool bag or with ice packs.
- Stored in the main part of the refrigerator (0-4°C) not in the door, for up to eight days from the date it was expressed.
- Clearly labelled with the baby’s name to ensure it is only used for that baby.
- Clearly dated when the milk was expressed.
Also note:
- If the milk smells overly sour, it may be spoiled. Be aware that defrosted breastmilk can have a more sour smell.
- When milk is stored, the milk may separate. It isn’t spoiled, just mix it gently before use (it may be spoiled if it doesn’t easily mix).
! Use a fridge thermometer to regularly check your fridge is operating to the correct temperature (0-4°C).
Heating
When preparing breast milk for a feed:
- The milk should be heated straight from the fridge. If it is not provided in a bottle transfer to a very clean bottle or cup. There’s no need to sterilise. Clean everything thoroughly in hot, soapy water and completely air dry, checking there is no dried in milk or soap left behind.
- Place the bottle in a bowl of warm water, ensure the cap covers the teat so that the teat is not contaminated with tap water.
- Check the temperature by putting a few drops on the inside of your wrist, it should feel slightly cool.
- Dry the outside of the container with a clean, dry cloth or kitchen roll before use.
- Shake the bottle before feeding.
- Follow the manufacturer’s instructions if you are using a warming device and ensure that the cap covers the teat.
If frozen breast milk is provided:
- It should be thawed in the refrigerator (0-4°C). Use breast milk on the same day it has been taken out of the freezer, throw away any unused milk.
- If needed, quickly stand in a container of lukewarm water, making sure only ¾ of the bottle is sitting in the water to avoid water leaking into the milk.
- Make sure that the cap covers the teat so that the teat is not contaminated with tap water.
- Gently shake to mix the milk.
! Thawed milk should not be refrozen.
! Microwaves should never be used to heat or defrost breast milk as they may overheat or heat the milk unevenly, which can scald the baby.
Exclusive breastfeeding is defined as no other food or drink, except breast milk. Under the age of 6 months, breast-fed babies do not need any additional fluids. This includes water, even in summer. Babies should be given more breastfeeds in summer to keep them hydrated. It is important to be guided by parents and carers if they have been advised otherwise by a health professional.
Around the age of 6 months, babies will begin to have solid foods, but breast milk will continue to provide most of the energy and nutrients that the baby needs and continue to help protect them from infections.
Mothers who are continuing to breastfeed may not want their baby to be given a bottle as the shape of the teat can disrupt their sucking patterns. They may prefer breast milk to be fed using a cup or spoon or ask you to mix expressed breast milk with food in a bowl. It is important to discuss any preferences and seek guidance from parents and carers. Practitioners should only provide specific services, requested by parents and carers, if they feel confident and are trained to safely do so.
For more information about breastfeeding refer to Off to a good start: all you need to know about breastfeeding, Breastfeeding: Ready Steady Baby! and the Parent Club website.
Providing a supportive environment to encourage breastfeeding
Childcare providers have a key role to play in ensuring that mothers are supported to return to work and continue breastfeeding.
The Breastfeeding etc. (Scotland) Act 2005 and the Equality Act 2010 make it an offence to prevent anyone feeding milk to a baby or a child under 2 years of age in a public place (excluding licensed premises). This means that mothers have the right to feed their baby milk in public at any time, whether breastfeeding or bottle feeding.
The importance of childcare settings in supporting mothers to breastfeed is highlighted in guidance provided by UNICEF, including guidance for children’s centres.
Some childcare settings are involved in developing activities to promote breastfeeding as a positive choice; for example, NHS Scotland’s Breastfeeding Friendly Scotland Early Learning Scheme is aimed at promoting breastfeeding so as many families as possible can benefit. Activities can include increasing staff knowledge and awareness, reviewing resources used within childcare settings, and providing a welcoming atmosphere to breastfeeding mothers.
Some areas in Scotland offer breastfeeding friendly nursery initiative. If this is of interest to you, visit the breastfeeding and your business section of the Scottish Government website for further details.
Relevant HSCS:
11.19 My care and support meets my needs and is right for me.
5.18 My environment is relaxed, welcoming, peaceful and free from avoidable and intrusive noise and smells.
5.17 My environment is secure and safe.
2.3 Formula feeding
The only recommended alternative to breast milk in the first 12 months is a ‘first infant formula’, or ‘first milk’, which is usually based on cows’ milk. All first infant formula milks contain the same ingredients and must comply with regulations, therefore there is no significant difference between the brands available.
Goats’ milk formula is also available and produced to the same nutritional standards as cows’ milk formula.
It is vital that practitioners know how to make up and store formula feeds (including how to prepare ready-made liquid formula) as safely as possible.
Equipment
- Bottle with a teat and a cap.
- Bottle brush and teat brush.
- Sterilising equipment such as a cold-water steriliser or steam steriliser (microwave or electric).
- A kettle.
Key safety points
- Formula powder is not sterile and provides an ideal environment for bacteria to grow. Using freshly boiled water (do not use water that has been boiled before) of at least 70°C to make up the feed will kill any harmful bacteria and reduce the risk of babies becoming unwell.
- Feeds should be made up in a suitable area where you can wash and dry your hands thoroughly before making up a feed.
- Equipment should be washed and sterilised. It is important to clean and disinfect all surfaces before using sterilised equipment.
- Multiple feeds should not be made up in advance. This is because the risk of bacteria growing in formula increases with storage time, even in a fridge. It is best to make up each feed as you need it.
- To reduce the risk of injury, make sure babies are not near the hot water when you are making up a feed. Take care not to scald yourself.
- Water should always be carefully poured into the bottle first and the correct amount of powder added afterwards. Always make sure you follow the manufacturer’s instructions on the packaging. The NHS website provides information on using a baby formula prep machine.
- Cool the formula before feeding the baby by holding the bottle under cold, running water and rotate to ensure even cooling. Make sure the cap covers the teat to avoid contamination with water.
- Check the temperature by putting a few drops on the inside of your wrist, it should feel slightly cool.
- Discard any infant formula milk that is left in the bottle after feeding as the combination of formula and a baby’s saliva can cause bacteria to grow.
- The milk in unused bottles of formula should be discarded if it has been kept at room temperature for over two hours.
- Ready-made liquid formula should be prepared and stored according to the manufacturer’s instructions on the packaging. Always check the use-by date and discard if it is out-of-date. All equipment should be washed and sterilised.
- Any unused ready-made liquid formula should be stored in the fridge, with the cut corner turned down/lid screwed back on or sealed in a sterile container. It should be discarded after 24 hours to minimise the risk of infection.
! Microwaves should never be used to heat up infant formula milk. There is a danger of overheating or heating the milk unevenly, which can scald the baby’s mouth.
! Adding too much or too little formula powder to the measured amount of water can cause babies to become ill. If you add too much powder, they can become dehydrated, if you add too little powder, they won’t get enough nutrients.
Types of infant formula milk and other milks
- All first infant formula milks are of a similar composition. The main difference between brands is cost. If families are struggling with the cost of purchasing infant formula milk for their baby, encourage them to contact their health visitor or family nurse for support.
- It is not necessary to switch to a follow-on formula milk. Although marketed to babies over 6 months, they have no advantage over ‘first milk’ infant formula and are not necessary.
- In hot weather babies under 6 months who are formula-fed may be given small amounts/sips of cooled, boiled tap water (with nothing added) between feeds.
Further information can be found in Public Health Scotland’s Formula feeding: How to feed your baby safely resource and the formula feeding pages of the Parent Club website.
A funded portion of infant formula milk is available to children under 12 months as part of the Scottish Milk and Healthy Snack Scheme (SMHSS). The scheme offers a daily portion of first infant formula (or specified alternative) for pre-school children spending two hours or more in the care of a regulated day care provider and/or childminder that is participating in the Scheme.
Babies under 12 months should only be drinking breast milk or infant formula milk. A wide variety of other types of infant formula milk are available in addition to first stage infant formula, such as anti-reflux and hungry baby milks. These often state they are suitable for use from birth; however, they should only be used on advice from a qualified health professional. If a parent or carer mentions their baby drinks any of the following milks, you should have a discussion with them about the milk not being suitable unless advised by a health professional.
Further information on infant milks can be found at First Steps Nutrition Trust.
| Type of Milk | Rationale |
|---|---|
| Cows’, goats’ and sheep’s milk | You should not give babies cows’, goats’ or sheep’s milk as a drink before they are 12 months old because they do not have the right mix of nutrients for this age. However, you can use them in cooking and with breakfast cereals from around 6 months as long as they are pasteurised full-fat milks. After 12 months, you can give children pasteurised full-fat or semi-skimmed milk as a drink as part of a healthy diet. |
| Goats’ milk infant formula | Goats’ milk infant formula is now permitted for sale in the UK and is made to the same nutritional standards as cows’ milk formula. However, it is not suitable for babies with a cows’ milk protein allergy, as the proteins are very similar to cows’ milk. |
| Soya-based infant formula milk | Soya-based infant formula is occasionally used for babies with a cows’ milk allergy but should only be used on advice from a health professional. It is only suitable from 6 months. |
| Unsweetened calcium fortified alternatives (e.g. soya, nut, oat, hemp, coconut-based milk alternatives) | These should not be given as the main drink before 12 months. However, you can use them in cooking and with breakfast cereals from around 6 months. |
| Rice milk and drinks | Rice drinks should not be given to children under 5 years because they may contain arsenic. Arsenic is found naturally in the environment and can find its way into food and water at varying levels. There are strict maximum levels set for rice milk and rice products available to buy, however a baby’s main milk drink should not be rice milk. If a baby in your care has had a rice drink, there is no immediate risk to them, but you should advise parents and carers to consult a health professional about a suitable alternative. |
| Lactose-free formula milk | Lactose-free formula milk is suitable for babies who are lactose intolerant. Lactose intolerance is rare in babies and this type of formula should only be used following advice from a health professional. |
Section 2.6 provides further information on unsuitable drinks for babies. Public Health Scotland’s Fun first foods: An easy guide to introducing solid foods and Formula feeding: How to feed your baby safely are useful resources to support you.
2.4 Introduction of solid foods
This section provides you with the most up-to-date advice given to parents and carers about the introduction of solid foods. For more information see Fun first foods: An easy guide to introducing solid foods, a resource given to parents and carers across Scotland, and the weaning and first foods pages of the Parent Club website.
Taking the lead from parents and carers
Babies should start eating solid foods at around 6 months. Parents and carers should inform childcare settings when they begin or plan to begin introducing solid foods to their baby.
The scientific evidence supports that babies should not be given solid foods before 4 months (17 weeks), because they are not developmentally ready to actively accept foods, and their kidneys and digestive system are still developing. There also may be an increased risk of infection and allergies if solid foods are introduced too early. Section 2.5 provides further information on allergies.
If a baby is being introduced to solid foods before 4 months, speak to parents and carers and recommend they seek advice from a qualified health professional.
The introduction of solid foods is a good opportunity to discuss feeding patterns and specific requirements such as allergies with parents and carers again. The baby feeding checklist can be used to do this.
! Introducing solid foods to babies is recommended at around 6 months.
Relevant HSCS:
1.35 I can enjoy unhurried snack and meal times in as relaxed an atmosphere as possible.
3.15 My needs are met by the right number of people.
Why introduce solid foods at around 6 months?
Breast milk or infant formula milk provide all the energy and nutrients babies need until around six months (except for vitamin D in breastfed babies who are recommended to be given a supplement). After this time the need for nutrients, particularly iron, cannot be met by breast or formula milk alone and a baby’s digestive system and kidneys are now ready to cope with solid foods. They will also be better at moving food around their mouth, chewing and swallowing different foods.
Breast milk and/or infant formula milk will continue to provide most of the energy and nutrients that babies need at this time. First foods provide first tastes, and allow babies to develop and practise the skills required for eating solid foods. It is important to look for signs that a baby is ready for solid foods.
Introducing solid foods is often an exciting but anxious time for parents and carers; it is a key life stage for babies. It is important to have regular conversations with parents and carers about how their baby is progressing and managing different textures and flavours.
Signs that a baby is ready for solid foods
It is important to focus on the developmental signs of readiness, rather than using a specific age or weight to determine whether a baby is ready for solid foods. Some of the signs that will occur around 6 months and suggest a baby is ready to accept solid foods are:
- The baby can stay in a sitting position and hold their head steady.
- The baby can reach out and grab things accurately, e.g. look at food, pick it up and put it in their mouth by themselves.
- Tongue reflex has developed to enable the baby move food around their mouth with their tongue instead of pushing food out.
If the baby is around 6 months and these signs are there, and in consultation with parents and carers, a small spoonful of soft food could be offered to see how they respond. Babies who are not ready will consistently push food back out with their tongue. Try offering again in a day or two and wait until they show signs of swallowing rather than always pushing the food out with their tongue.
Relevant HSCS:
1.19 My care and support meets my needs and is right for me.
1.35 I can enjoy unhurried snack and meal times in as relaxed an atmosphere as possible.
The following behaviours can be mistaken as signs that a baby is ready for solid foods:
- Chewing their fists.
- Waking up in the night (more than usual).
- Wanting extra milk feeds.
What to expect
Many babies are slow to eat in the beginning; be patient and let them take it at their own pace. First foods are just about babies exploring new tastes and learning how to move solid foods around their mouths and how to swallow them. Try not to worry too much about mess. It is important for babies to learn about food by touching, squishing or smelling, as well as tasting it.
At around 6 months most babies prefer to use their fingers while they are learning to use a spoon. They may need some assistance until they are more confident using a spoon, and in the beginning only small amounts of food may be eaten. It is important to let babies explore the food on their plate and feed themselves whenever possible, but always under close supervision.
! Never leave a baby unattended while feeding. Refer to Section 2.8 for information on how to prevent babies from choking.
Some babies take to solid foods quickly, but others take longer. New foods may need to be offered several times before they are accepted (as many as 10 times or more). It is important for practitioners to have enough time to feed babies in a relaxed atmosphere so they can eat at their own pace.
Respond to a baby’s hunger and fullness cues. They may be ready for more food when they lean towards the food with an open mouth or pull food towards their mouth. When a baby is full, they may close their mouth or turn their head away.
It is normal for a baby’s appetite to change from day to day and you shouldn’t worry if they eat more on some days than others. Don’t force them to take the food, if they don’t seem to want it, try again later.
First foods at around 6 months
At around 6 months, soft finger foods and mashed foods can be given. Babies take different amounts of time to get used to more textured, lumpy food. Babies that have started solid foods before 6 months are likely to need their food puréed and may need more support with feeding. Section 2.9 provides guidance when solid foods have been introduced before 6 months.
A variety of solid foods and textures should be gradually introduced alongside a baby’s usual milk feeds (expressed breast milk or infant formula milk). Offer babies solid foods when they are relaxed, happy and not overly hungry. At first, offer small amounts before their usual milk feed. It is best to be guided by parents and carers to ensure that what you do fits with their baby’s normal routine.
Try the following suggestions for first foods:
- Use unprocessed foods where possible and do not add any sugar or salt.
- Mashed cooked vegetables such as broccoli, cauliflower, carrot, parsnip or turnip.
- Mashed fruit such as banana, stewed apple or pear.
- Fist-sized/long pieces or batons of soft fruit or cooked vegetables, such as melon or carrot.
- Strips of toast, bread, pitta bread or chapatti (about the length of your finger).
- Pasteurised cheese (sliced or grated), scrambled or hard-boiled egg quarters or pieces of cooked fish that they can hold in their fist (be careful to remove all bones from cooked fish).
- Plain breakfast cereal mixed with their usual milk feed (expressed breast milk or infant formula milk), always in a bowl, never in their bottle. If baby is 6 months or over, pasteurised, full-fat milk can be used to mix with breakfast cereal or used in cooking.
Section 2.6 provides information on suitable drinks for babies from six months.
It is important to remember there are several foods and drinks that should be avoided in the first year of life and these can be found in Section 2.7.
! Some foods are not recommended until babies are around 6 months old. If parents or carers have decided to introduce solid foods before 6 months Section 2.9 provides further information.
Moving on
Once a baby is used to eating a few foods, you can offer a wider variety of foods and textures. The need for iron and other important nutrients increases as they grow, and this change needs to be met with an increased variety of foods.
Offering a wide range of foods, textures and flavours can help increase the variety of accepted foods and encourage healthier eating habits later in childhood. Continue to offer foods, including fruit and vegetables and those with bitter flavours, even if they have been rejected. It can take multiple times (as many as 10 times or more) for a new food or texture to be accepted, particularly as children get older.
Aim to include a variety of the following:
- Fruits and vegetables, including savoury and bitter vegetables, such as broccoli, cauliflower, spinach, cabbage or courgette.
- Potatoes, rice, pasta, breads, oats, low sugar breakfast cereals, such as wheat biscuits or plain porridge, and other starchy foods.
- Beans, pulses, eggs, fish including oily fish, such as mackerel or salmon, and pieces of well-cooked meat.
- Full-fat pasteurised dairy products, such as cheese and plain yoghurt.
! Always remove bones from cooked meat and fish.
A baby’s appetite will vary from day to day, and they are normally very good at regulating their own food intake. Look out for signs of fullness such as the baby closing their mouth, turning their head away from the food or pushing the food away. Avoid pushing the baby to eat more than they want to.
It is important to discuss a baby’s normal eating pattern with parents and carers to make sure you are providing a consistent approach. A daily feeding diary is a useful communication tool.
More meals and more textures
Gradually increase the number of times you offer food each day. Begin with one meal a day, then two, then three in addition to their usual milk feeds. As a baby eats more solid food, they may take less milk at each feed or may even drop a feed altogether. Let the baby guide this process.
Continue to offer milk feeds on demand between meals and speak to parents and carers regularly about changes to the feeding routine at home. A cup of still, plain water, in a free flow cup (without a valve), can be offered with meals from around 6 months.
Babies should be gradually introduced to more textured foods as soon as they are ready, so that by the age of 10 months they are used to eating lumpy and finger food regularly. Some babies will be happy with mashed, lumpy or finger foods from the start, but others may prefer smooth or blended food on a spoon and will take longer to get used to new textures. Mixing a new food with a familiar one, such as adding cooked lentils to mashed carrot or parsnips, may make this progression easier.
Use a spoon and encourage finger foods and self-feeding, however messy it is. Some babies may enjoy feeding themselves as it gives them the independence to control their own food intake.
Any concerns around the feeding patterns of the babies in your care should initially be raised sensitively with parents and carers. The family health visitor may be able to support with advice and practical suggestions.
As babies approach their first birthday, they should be eating a wide range of different foods from a variety of food groups each day. From the age of 12 months you should be offering children three main meals plus two or three snacks each day. Section 3 provides guidance for children aged 1 to 5.
Public Health Scotland’s Fun first foods: An easy guide to introducing solid foods, the weaning and first foods pages of the Parent Club website and Eating well in the first year from First Steps Nutrition Trust are useful resources providing further information on introducing solid foods, portion sizes and meal ideas.
2.5 Meal planning
Whether you decide to prepare food on site, or use another food service provider, it is good practice to plan the meals you will provide for the babies in your care. Some parents and carers will only use ready-prepared manufactured foods, others will want their baby to have home-prepared foods, and some parents and carers will use a mixture of both.
It is important to involve parents and carers in any decisions around meal planning. It is also good practice to use your menus to support any discussions with them.
If parents and carers would like to bring in food from home while their baby is introduced to solid foods, it is important to let them know what can be stored and heated appropriately within your setting. It is a good idea to include food brought in from home as part of a food and nutrition policy. Section 5 provides more information on Food from home and Developing a food and nutrition policy.
Sample menus that have been provided for children aged 1 to 5 can be used as a guide for menu planning for babies. In consultation with parents and carers, and food service providers, these menus can be adapted to suit the age and stage of each baby.
An example menu, which has been adapted from the meals provided in sample menu week 1, has been provided in the next page as a guide. The stages shown in Section 2.4 should be used to help further adapt the menus to suit the needs of each baby from when they are introduced to solid foods, at around 6 months, to eating the range of meals and snacks as shown in the sample menus from the age of 1 year.
Around 6 months-1 year sample menu
| Monday | Tuesday | Wednesday | Thursday | Friday | |
|---|---|---|---|---|---|
| Breakfast | Toast fingers with spread, plain yoghurt and pineapple slices | Malted wheat cereal with milk and chopped plum (skin removed) | Toast fingers with spread, scrambled egg and tomatoes (mashed or cherry tomatoes quartered) | Wheat biscuits with milk and banana (sliced) | Porridge and blueberries (mashed or quartered) |
| Lunch | Roast chicken (chopped) with gravy, mashed potatoes and a vegetable medley Baked apple with custard |
Tofu and vegetable noodles (chopped) Plain fromage frais with pear slices |
Beef casserole (chopped) Cheese batons with sliced grapes |
Salmon fish cake with peas and sweetcorn (mashed) Plain yoghurt with mixed berries (mashed or quartered) |
Pasta (well-cooked smaller shapes) with tomato and lentil sauce Fruit selection |
| Tea | Carrot and butter bean (mashed) soup with a wholemeal roll (strips) Peaches in juice (drained) |
Tuna and cucumber wrap (deconstructed where required- cucumber sticks and wrap strips) Fruit platter |
Cous cous with chickpeas (mashed) and tomatoes (mashed or cherry tomatoes quartered) Fruit selection |
Vegetable sticks (hard vegetables cooked until soft or grated) Muffin pizza faces (sliced into strips) |
Baked potato (skin removed) with baked beans (mashed) Fruit salad with plain yoghurt or fruit selection |
A baby’s usual milk or water can be provided at all meal and snack occasions in consultation with parents and carers. However large volumes of milk after 1 year are discouraged (i.e. more than 600ml) as it may reduce appetite for other foods. Fruit should be available as a choice for children as an alternative to the dessert/pudding each day. Food should be prepared for the age and stage of the child to avoid choking risk. Please refer to Sections 2.4, 2.5 and 5.6 of the guidance for further information. |
|||||
In consultation with parents and carers, and food service providers, these menus can be adapted to suit the age and stage of each baby to avoid a choking risk. This will be different for each baby, but consideration should be given to the texture and size of the food, for example: cooking harder fruits and vegetables until soft, removing the skin and offering safe sizes and shapes of the food.
Section 2.4 provides further information on introducing solid foods. Refer to the Care Inspectorate’s Good practice guidance on prevention and management of choking episodes in babies and children, Section 2.8 and Section 5.6 for further information on choking.
It is important that you check labels on any ready prepared foods as they may have high levels of salt and sugar that make them unsuitable for babies. The Eatwell Guide Booklet provides more information on how to interpret food labels.
| Sugar | Salt |
|---|---|
Added sugar is not necessary for babies. It provides little nutritional value and causes tooth decay. Giving sweeter foods with added sugar to babies may encourage a preference for sweeter tastes, which in turn may negatively impact the acceptance of less sweet foods, such as vegetables and pulses. Avoid adding sugar to food and limit sweet tasting foods. Any foods provided in childcare settings containing non-sugar sweeteners should be carefully considered to ensure that sugary products aren’t simply replaced with sweetened products. See Section 3.3 for more information. Only plain varieties of yoghurts should be provided. Foods such as flavoured yoghurts, fromage frais, and tinned and packet milk puddings often have a lot of added sugar. Milk and water are the best drinks for babies and young children. Fruit juices should not be provided. Although fruit juices are a good source of vitamin C, they are acidic and contain lots of natural sugar, which can be harmful to teeth. |
Do not add salt to a baby’s milk or food (including during the cooking process). Babies under 1 year old need less than one gram (a sixth of a level teaspoon) of salt per day, as their kidneys can’t cope with more. If a baby is breastfed, they will get the right amount of salt from breast milk, and infant formula milk contains a similar amount. Salt is added to a lot of foods, for example smoked and processed foods, tinned tuna in brine, soy sauce, stock cubes and some breakfast cereals. Look for lower salt varieties and avoid high-salt foods. |
Things to consider if you use shop bought baby foods
- Shop-bought baby foods must follow strict guidelines about what can and can’t be included in the food. These do not however ensure that food is health promoting or appropriate for babies. Choose foods without any added sugar or salt and even if they taste bland to you, you shouldn’t add any sugar or salt to baby foods yourself.
- Check the ingredients list to see the breakdown of ingredients within the food. The name of the food is not always a true reflection of the content. A product called broccoli, peas and pear, for example, may only contain a very small percentage of broccoli, the bitter tasting food, and contain larger amounts of the sweeter-tasting peas and pear.
- Some baby foods may say ‘suitable from 4 months’ on the label but health experts agree that around 6 months is the safest age to start to introduce solid foods. Some may contain gluten or dairy products which are not recommended before 6 months. Make sure you check the label for suitable foods if you are providing them for babies in your care. Section 2.9 provides further information on the introduction of solid foods before 6 months.
- Make sure foods are within their use-by date and that the seal has not been broken before use.
- It is best to decant the food from the jar or pouch into a bowl and then feed a baby from the bowl with a spoon. This supports better feeding development and avoids bacteria and other infectious agents transferring between a baby’s mouth and the jar or pouch. Around a third of commercial baby foods and drinks are packaged in pouches, many of which have nozzles. Sucking from these pouches is harmful for developing teeth.
- Babies won’t necessarily finish the whole jar or pouch. You should serve a small amount in a bowl and top up as required. Any remaining food can be sealed and kept in the fridge for up to 24 hours. Any uneaten food from the bowl should be thrown away.
- Shop-bought baby foods often have the same texture, making it harder for babies to adapt to more varied textures and to move to family foods as they get older. They are often made up of more than one food which doesn’t help babies get used to individual flavours and textures. Home-made foods can be easier to adapt to suit the developmental stage of each baby, they can offer more variety in texture and are likely to encourage better acceptance of lumps and more solid foods.
- Making your own food tends to be cheaper than buying shop-bought baby foods.
It is important to discuss with parents and carers if you are concerned about any food they have provided.
Food Allergies
It is important that you introduce the foods that most commonly trigger allergic reactions one at a time and in very small amounts, to spot any reaction. In consultation with parents and carers, these foods can be introduced from around 6 months as part of a baby’s diet, just like any other foods:
- Cows’ milk (in cooking or mixed with food but not as a main drink).
- Eggs.
- Foods that contain gluten, including wheat, barley and rye.
- Peanuts and tree nuts.
- Seeds (served crushed or ground).
- Soya.
- Shellfish.
- Fish.
Once introduced, and if tolerated, you can continue to offer these foods as part of a baby’s usual diet in consultation with parents and carers.
Childcare settings should watch out for symptoms of an allergic reaction.
This can be one or more of the following:
- Diarrhoea or vomiting.
- A cough.
- Wheezing or shortness of breath.
- Itchy skin or throat.
- A rash.
- Swollen lips and throat.
- Runny or blocked nose.
- Sore, red and itchy eyes.
It is important to discuss any allergies with parents and carers to ensure you can provide food safely. The baby feeding checklist can support this discussion.
Once a food from the list above is introduced and tolerated, it should be included in the baby’s diet regularly. Regular inclusion of a food in the child’s diet will continue to prevent an allergy developing later in life. Deliberate exclusion of any food beyond 12 months should be avoided unless there is good reason, as this may increase, rather than decrease, the risk of future allergy.
Section 4 provides information on meeting the needs of all children and how to take appropriate action if a child has an allergic reaction.
2.6 Suitable drinks for babies from around 6 months
What a baby drinks is just as important as what they eat. The only drinks that should be provided in the first year are:
- Breast milk.
- Infant formula milk.
- Still, plain water.
Water hydrates without providing extra sugar, so it doesn’t damage children’s first teeth. Breast milk or infant formula milk should continue to provide a substantial amount of fluid and nutrients for babies in their first year of life. Breastfed babies don’t need water for the first 6 months. Formula fed babies under 6 months may need some extra water (cooled boiled tap water) in hot weather. Section 2.2 Breastfeeding and Section 2.3 Formula feeding provide further information.
Follow-on formula and ‘Growing up’ milks are not suitable under 6 months, and not necessary for babies older than 6 months.
Babies need to learn to sip, not suck, and therefore free flow cups (without a valve) are recommended. Non-spill cups (with a valve) encourage babies to suck rather than sip and should be avoided.
Public Health Scotland’s Fun first foods: An easy guide to introducing solid foods and Eating well in the first year from First Steps Nutrition Trust provide further information on drinks and the reasons why many are unsuitable at this age.
2.7 Foods to avoid in the first 12 months
There are several foods that should be avoided. This is for a variety of reasons such as food safety and choking risk, and for the negative impact some foods could have on a child’s long-term health and development.
They are as follows:
| Foods to avoid from around 6 months to 1 year | |
|---|---|
| Honey | Honey can contain bacteria that can harm a baby’s intestines, leading to botulism, which can be very serious. Therefore, giving young babies honey in the first 12 months should be avoided. |
| Added sugar | Consuming too much sugar increases the risk of future tooth decay and can cause a high energy intake. |
| Added salt | A baby’s kidneys are not mature enough to cope with added salt or foods with salt added during processing. |
| Unpasteurised dairy products and some cheeses | Unpasteurised dairy products can contain bacteria and there is an increased risk of food poisoning, so it’s better to avoid them. Babies should also avoid mould-ripened soft cheeses such as brie, camembert and Roquefort, as there is a higher risk that they may contain a bacteria called listeria. |
| Shark, marlin and swordfish | Should be avoided until 16 years old due to mercury levels, which affects a growing nervous system, . |
| Shellfish (raw) | Raw shellfish can increase a baby’s risk of food poisoning. Other fish and cooked shellfish are suitable from around 6 months. |
! Babies and children can eat raw or lightly cooked UK hen eggs or foods containing them, provided that the eggs are produced under the Lion Code with a British Lion mark, or under the Laid in Britain egg assurance scheme. If the eggs are not Lion Code or Laid in Britain, or if in doubt, then they should be fully cooked.
2.8 How to prevent babies from choking
During the first year of life, babies are still learning to enjoy food and developing the skills and muscle coordination needed to eat a much wider variety of foods. It is, however, important to ensure that babies are kept safe and that they do not choke on food.
Babies should not be given solid foods before they are 4 months (17 weeks), as this will increase the risk of choking. Wait until around 6 months before introducing solid foods. Section 2.4 provides more information on the introduction of solid foods.
! To avoid choking, babies must always be supervised when eating.
There is a difference between choking and gagging. Gagging is a normal reflex and is commonly experienced by babies as they learn to chew and swallow solid foods. Gagging is usually noisier. Babies’ skin may also look red when they are gagging, but redness can be harder to see on dark skin. Choking is usually quiet.
The following key points are important to help you reduce the risk of babies choking:
- Always stay with a baby when they are eating.
- Cook hard or stringy fruits and vegetables until they are quite soft for use as finger foods, rather than offering them raw.
- Remove any stones, pips or tough skin from fruit and vegetables.
- Cut fruit and vegetables into slices rather than chunks or round shapes.
- Remove bones, skin or stringy bits from cooked meat and fish.
- Finely chop, crush or grind nuts, peanuts and seeds.
- Encourage a baby to chew by offering different textures.
- When eating, a baby should be sitting up, preferably in a highchair with a securely fitted harness and a foot rest (to stop them slipping down).
- Stop a baby from putting too much food in their mouth in one go.
- Give the baby time to swallow each mouthful.
- Make sure a baby’s mouth is empty before taking the next mouthful of food. It is important to go at the baby’s pace.
- Let the baby feed themselves so they have more control over what goes into their mouth.
- Remember to always supervise a baby closely when they are eating.
Relevant HSCS:
3.15 My needs are met by the right number of people.
4.11 I experience high quality care and support based on relevant evidence, guidance and best practice.
5.17 My environment is secure and safe.
It is also important for you to consider the needs of individual babies and take guidance from parents and carers.
Further information on choking can be found in Section 5.6. The British Red Cross website provides guidance on what to do when a baby is choking.
2.9 Introducing solid foods before 6 months
The World Health Organization and the Scientific Advisory Committee on Nutrition advise waiting until babies are around 6 months to introduce solid foods, and that this should never occur before 4 months. However, some parents do introduce solid foods before 6 months and the reasons are often complex.
Suitable foods before 6 months
If you are asked by a parent or carer to give a baby solid food before 6 months, the foods must be puréed to a smooth, thin consistency as the baby may not be developmentally ready to cope with lumpy or finger foods.
Some examples of suitable foods are:
- Puréed vegetables such as spinach, courgette, carrot or parsnip.
- Puréed fruit such as avocado, apple, pear or banana.
- Plain baby rice mixed with the baby’s usual milk and served in a bowl, not a bottle.
All equipment for spoon feeding must be sterilised until the baby is 6 months old. Offer small amounts to begin with and look out for signs they have had enough. The amount you give should be guided by the baby’s appetite and information from parents and carers.
Unsuitable foods before 6 months
In addition to the foods to avoid in the first year, provided in Section 2.7, there are certain foods that should not be given to babies less than 6 months of age (unless recommended by a health professional), and these include:
- Foods containing gluten like wheat, rye and barley. These can be found in pasta, rusks, bread, flour and breakfast cereals containing gluten.
- All fish and shellfish (e.g. tuna, cod, salmon, prawns).
- Any milk or milk product (e.g. cheese, yoghurt) apart from breast milk or their usual infant formula milk.
- Eggs.
- Honey.
- Nuts and seeds.
! Remember, foods that can trigger an allergy should be introduced in small amounts, and one at a time from around 6 months, unless advised otherwise by a health professional. Section 2.5 provides information on food allergies.
Contact
Email: elc@gov.scot
There is a problem
Thanks for your feedback