Setting the Table Guidance
Nutritional Standards and Practical Guidance for Early Learning and Childcare Providers in Scotland. Childcare services providing food and/or drinks to children 0-5 years, and are registered with Care Inspectorate, will be responsible for the implementation of this guidance.
3 Guidance for children aged 1 to 5
3.1 The importance of a healthy balanced diet
A healthy balanced diet for 1 to 5 year olds is important because it:
- Supports optimal growth and development.
- Supports children to eat well, and to have a healthy weight and good oral health.
- Can expose children to a variety of foods and builds the foundations for future health.
- Can shape food preferences and eating habits that children take with them into later childhood and beyond.
3.2 A healthy balanced diet for 1 to 5 year olds
Children aged from 1 to 5 years need the right amount of food and nutrients to develop and grow. A healthy diet is one that provides enough energy and the right balance of important nutrients (including vitamins, minerals and protein) and fibre, whilst limiting fat (especially saturated fat), sugar and salt intake.
Children’s diets should be varied and include a range of foods with different flavours and textures. Young children’s nutritional requirements are notably different to those of older children and adults. Children in the early years are growing rapidly and require more energy and nutrients in each mouthful of food compared to adults. Dietary recommendations as shown in the Eatwell Guide apply from around 2 years of age. Between age 1 and 2, children’s diets should continue to be diversified to include more foods, flavours and textures. How quickly this is done depends on the age and stage of the individual child.
From around 2 years onwards fibre can be slowly increased, whilst the full-fat products can start to be replaced with the lower fat products. Semi-skimmed milk can be given from 1 year as a main drink, unless otherwise advised by a parent/carer or health professional.
It is important that children aged from 1 to 5 years continue to be offered a wide range of foods that are good sources of iron. They do not require iron supplements unless advised by a health professional. Iron comes from a variety of both animal and plant sources including red meat, fish, poultry, beans, pulses, dried fruit, fortified breakfast cereals and dark leafy vegetables. In practice, achieving adequate iron intake is not easy and requires careful menu planning to ensure that iron-rich foods are included on a regular basis.
It is important that you take a flexible approach to allow for differences in children’s development and nutritional needs. This should be in discussion with parents and carers. It is important to remember that the quantities of food a child wishes to eat may vary greatly from child to child. Few children want to eat the same amount every day. Appetite can change according to how active the child is, if they are unwell, their mood and whether others are eating with them.
The Eatwell Guide shows the types and proportions of foods needed to make up a healthy balanced diet with plenty of fruit, vegetables and starchy carbohydrates plus some dairy and dairy alternatives, beans, pulses, fish, eggs, meat and other proteins.
The proportions shown are representative of the foods that should be consumed over a day or even a week, not necessarily at each meal.
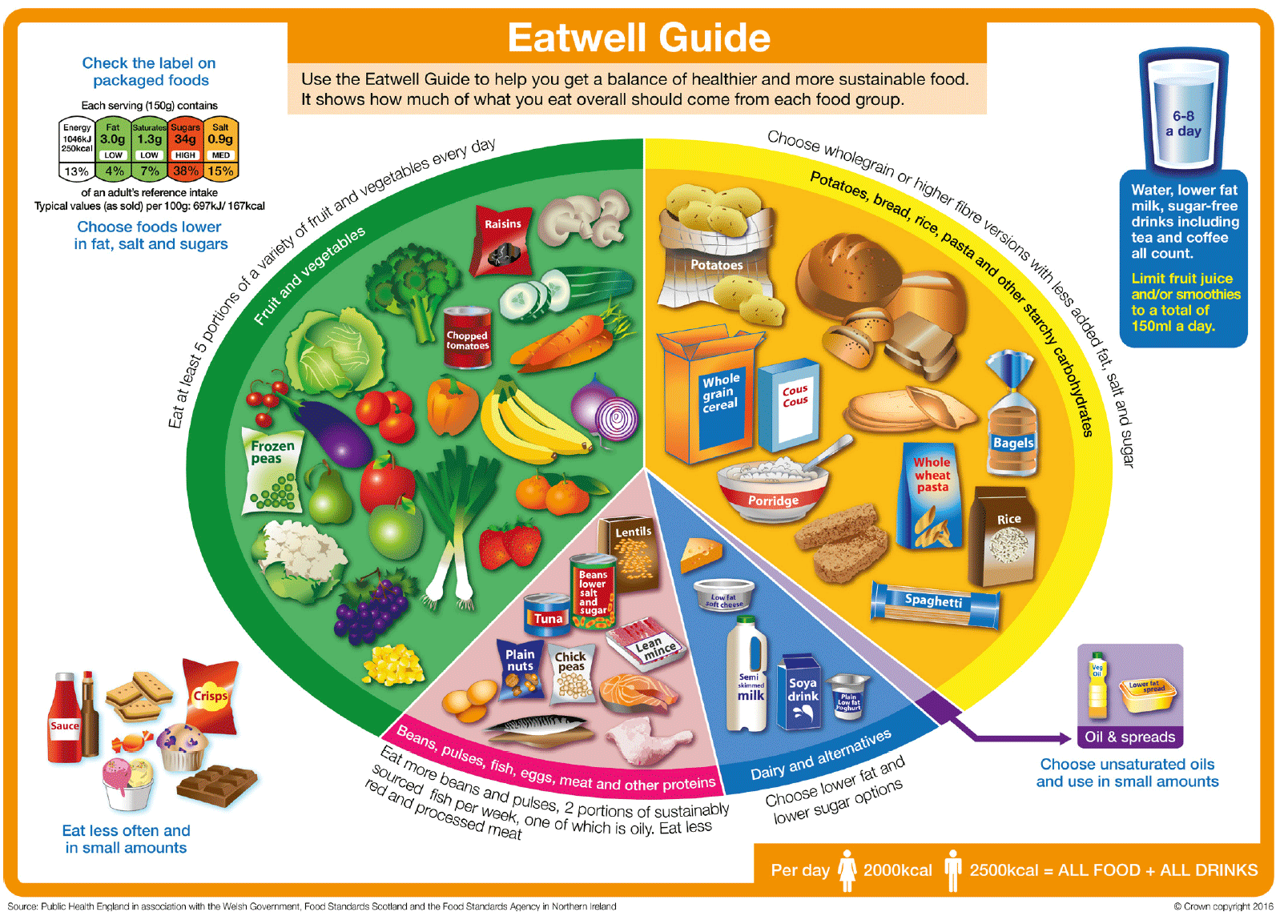
The Eatwell Guide applies to most people regardless of weight, dietary restrictions/preferences, or ethnic origin. However, it doesn’t apply to children under 2 years because they have different nutritional needs. From around age two children should gradually move to eating the same foods as others in the proportions shown in the Eatwell Guide, unless advised otherwise by a parent/carer or health professional.
The food and drink standards provided in this guidance have been developed to support the recommendations of the Eatwell Guide. Planning meals, snacks and drinks around these standards will help you to provide a variety of foods to meet the nutritional requirements of the children in your care. Sample menus have been developed to show how these standards can be met.
Parents and carers of children with special dietary requirements or medical needs may want to check with a registered dietitian on how to adapt the Eatwell Guide to meet their individual needs. Section 4 provides further information on meeting the needs of all children.
Health and sustainability
Health and sustainability go hand in hand. The Eatwell Guide has a lower environmental impact than the current UK diet. The food and drink standards in this guidance are aligned to the Eatwell Guide, so they are helping to support you to provide a more sustainable menu.
There are further actions you can take to improve the sustainability of the food you offer:
- Reduce the amount of food you waste by buying and preparing only the amount of food you need. Visit Zero Waste Scotland for more information.
- Buy products with minimal packaging or recyclable packaging.
- Avoid buying fish rated as ‘fish to avoid’ by the Marine Conservation Society and buy fish from sustainably managed stocks which is Marine Stewardship Council (MSC) certified.
- Choose food that is grown locally and that is in season where possible.
- Growing fruit, vegetables and herbs to use within menus.
Love food hate waste is a useful website providing further information.
Communicating with Parents and Carers
Talk to parents and carers about the food and drinks you provide across the day. This could include information on the routine for meals and snacks you provide and your weekly menus. It will support parents and carers to plan their child’s routine at home and with all the settings they attend, if more than one.
Breakfast is an important meal for young children. It is good practice to liaise with parents and carers to make sure that children always eat breakfast, whether at home or when they arrive at the setting.
Relevant HSCS:
1.36 If I wish, I can share snacks and meals alongside other people using and working in the service if appropriate.
3.3 Standards and menu planning
Food and drink standards have been developed to help childcare settings plan their menus for children in their care, whether they attend full-day care (approximately 10 hours/ day) in one setting or attend several settings throughout the week. There are 14 standards covering provision at meal and snack times, to ensure children get a balance of nutrient rich foods across the day.
The standards are evidence based and have been developed to reflect the current recommendations and the Eatwell Guide.
The following pages list each food standard and what is expected of childcare settings when complying with these. They also include information on why each standard is important and practical guidance points to assist in the implementation of them. Section 5 also provides information on putting the guidance into practice.
Energy requirements and menus
A full menu of a main meal, two light meals, two snacks and drinks should provide around 90% of the energy requirement for a child in full-time childcare (approximately 10 hours/day). The meals provided will be dependent on the opening hours of the childcare provider and the length of time the child is within the setting. The percentage energy intake for each meal or snack occasion, if provided, is listed below.
This is split across the following eating occasions:
- Light meal, e.g. breakfast, provides 20% of a child’s energy requirement.
- Snack, mid-morning, provides 10% of a child’s energy requirement.
- Main meal, e.g. lunch, provides 30% of a child’s energy requirement.
- Snack, afternoon, provides 10% of a child’s energy requirement.
- Light meal, e.g. tea, provides 20% of a child’s energy requirement.
Where these meals and snacks are provided within the setting, the remaining 10% of a child’s energy requirements will be provided at home.
The meals and snacks a child is provided dependent on how long their childcare session is each day and the setting’s approach to the provision of food, which may include home provided food. Under the National Standard for funded ELC, a free meal is provided and can be delivered as a light or main meal.
The food and drink standards provide a guide to how to meet the nutritional requirements of children aged from 1 to 5 years. The sample menu and the accompanying recipes have been analysed to ensure they meet these requirements. The nutrient standards are provided in Appendix 1 for information. There is no expectation that childcare settings will nutritionally analyse their menus, however, some may choose to do so.
The sample menus, accompanying recipes and menu planning information can all be used to help plan menus within your setting. The menus can be adapted to meet the needs of cultural and religious beliefs. Further information on meeting the needs of all children can be found in Section 4.
Menu Planning
Planning your menus, including snacks and drinks, is an important step in achieving a well-balanced and healthy diet for the children in your care. The sample menus can be used as a guide.
Consideration should be given to the existing eating habits of children in your care. Any change to these through new menu planning and the application of the food and drink standards should be carefully managed, and a staged and flexible approach taken if required.
The standards and guidance provided should be used to help produce a written menu covering all the food you provide, i.e. meals, snacks and drinks. They can also be used to develop a specification for food service providers when they provide meals for your setting.
You can use your developed menus as part of the evidence to show that you are meeting the standards set out in this guidance. Use the menu checklist to help you do this.
The Eatwell Guide can also be used to help menu planning to ensure the following:
- All meals should provide at least one serving from the starchy food group (potatoes, bread, rice, pasta and other starchy carbohydrates).
- A light meal should provide at least one serving of food from the fruit and vegetables group.
- A main meal should provide a minimum of two servings of vegetables.
- All meals (excluding breakfast) should provide one serving from the beans, pulses, fish, eggs, meat and other proteins group. However, these foods can also be served at breakfast.
Where vegetarian menus are required, a sample menu has been provided as a guide. It is important to discuss each individual child’s vegetarian diet with parents and carers. Details of the foods and ingredients that can and can’t be eaten should be recorded in the child’s care plan to support menu planning.
A range of foods should be provided to ensure that children who follow a vegetarian diet get the variety of nutrients required. To ensure this, cheese should only be served as the main protein source twice per week across lunch and tea.
Vegetarian diets can be perfectly healthy for growing children providing they are carefully planned, offer a variety of foods, and include sufficient protein, iron, vitamin B12, calcium and iodine. The sample menus, which are nutritionally analysed to meet nutrient standards, and the accompanying recipes provided with this guidance give examples of vegetarian choices.
A vegan diet excludes meat, fish, poultry, eggs, honey, dairy products and any other animal products. As animal products are the main sources of some nutrients (e.g. vitamin B12 and iodine), it can be difficult to ensure children following a vegan diet meet their nutritional needs. It is important that a vegan diet is carefully planned to make sure children get all the nutrients they need.
First Steps Nutrition, Eating well: vegan infants and under 5s provides further information about catering for children who follow a vegan diet.
Frequency and variety of menu options
Some children will only attend a setting for part of the week and on the same days each week, and some children may attend more than one ELC setting. To ensure that these children have variety in menu options, it is best practice to vary the days that menu items are provided from week to week. For example, if a fried item is offered every Monday and a child only attends that day, they will always have the fried item and not have the opportunity to have other foods. Similarly, the meal occasions where items like sweetened and baked goods are provided should be varied.
Portion sizes
Children’s appetites can vary for a number of reasons; some children will eat more, and some will eat less. It is normal for a child’s appetite to vary across a week and as they grow. Portion sizes should be varied to meet the needs of each child.
The sample recipes include indicative portion sizes. These portion sizes have been calculated based on the full menu providing 90% of energy requirement for a child in full-time care, as stated above. However, some children may require more or less than this, dependent on their appetite.
Suggested portion sizes for fruit and vegetables can be found in Standard 1.
Relevant HSCS:
1.37 My meals and snacks meet my cultural and dietary needs, beliefs and preferences.
Food variety and textures
It is important to include a variety of sensory qualities, e.g. taste, texture, flavours, colours and temperature. Encouragement from an early age and offering new foods regularly can help to increase the diversity of a child’s diet.
Offering children unfamiliar fruit and vegetables, including those with bitter flavours, on multiple occasions (as many as 10 times or more) can help develop and support their regular consumption. Offering a wide range of foods, textures and flavours can help increase the variety of accepted foods and encourage healthier eating habits later in childhood.
Children should be given the chance to try different foods through regular changes to menus. Regular menu changes give the opportunity for seasonality to be incorporated too.
Children’s cultural backgrounds should also be considered, and inclusion of dishes which reflect these cultures is encouraged. Section 4.2 provides further information on food for religious faiths and beliefs.
Guidelines for snacks and drinks
Snacks and drinks form an important part of a young child’s diet. Having a variety of choices can help young children to make their own decisions and make snack time a learning experience. Section 5 provides more information on how to put this into practice.
Make sure your snack choices are varied to ensure that children who are not attending full-time care, i.e. one or two days only or part days each week, are offered a variety of choices.
Snacks and drinks should be nutritious and lower in fat, salt and free sugars, to ensure children in your care are provided with the right balance of nutrients for health and growth. Fruit and vegetables are healthy snacks but should be combined with other nutritious foods to ensure variety is included and that a range of nutrients and sufficient energy are provided. See sample menus for examples.
Foods (including snacks) that are energy dense and high in saturated fat, salt or free sugars should be limited in children aged from 1 to 5 years.
Shop-bought foods and drinks marketed specifically for infants and young children are not needed for children to meet their nutritional requirements.
The food and drink standards section outlines information about what should and should not be available as snacks, and general guidance for planning healthier menus, snacks and drinks for young children in your care. The sample menus provided include examples of snacks.
All pre-school children spending two hours or more in the care of a participating, regulated daycare provider and/or childminder are entitled to funding for a daily portion of milk (189mls), or specified non-dairy alternative, and a healthy snack of fresh fruit or vegetables through the Scottish Milk and Healthy Snack Scheme (SMHSS). Semi-skimmed milk should be provided for children over 1 year old unless otherwise advised by a parent/carer or healthcare professional.
Understanding food labels
Meeting the food and drink standards may mean that you need to substitute some products for similar ones that are lower in fat, salt and/or free sugar, or contain more fibre. To do this you will need to be able to understand and compare food labels. The Eatwell Guide Booklet provides more information on how to interpret food labels.
Advice on non-sugar sweeteners
All non-sugar sweeteners that are used in the UK and EU undergo a rigorous safety assessment by the European Food Safety Authority (EFSA). Any foods provided in childcare settings containing non-sugar sweeteners should be carefully considered to ensure that we do not simply replace sugary products with sweetened products. This teaches children’s palates to expect sweet-tasting food and drink and may lead to them making less healthy choices in the future.
3.4 Food and drink standards
Standard 1: Fruit and vegetables
Main meal
At least two portions of vegetables should be provided.
Where a dessert is provided, a portion of fruit should always be an option.
Light meal
A fruit and/or vegetable portion should be provided.
Snack
A fruit and/or vegetable portion should be provided.
Dried fruit should not be provided at snack occasions.
Guidance on portion sizes
A portion of fruit or vegetables should be around 40g. A practical measurement for young children is that a portion should be able to fit in their hand.
A portion of dried fruit should be no more than 15g. Dried fruit should be limited to once per day, either at main meal or light meal, and an alternative fruit should always be provided.
Why is this standard important?
It is desirable to increase fruit and vegetable intake because:
- Fruit and vegetables provide a wide range of vitamins, minerals and fibre and can help us stay healthy.
- Current recommendations are to eat at least five portions of a variety of fruit and vegetables each day as part of a healthy, balanced diet. The table below outlines approximate portions for children aged 1 to 5 years.
- Very few children in Scotland currently eat the recommended amount of five or more portions of fruit and vegetables a day. Supporting children to eat more will have long-term health benefits.
- When possible, choose fruit and vegetables that are grown locally and are in season.
Low consumption of fruit and vegetables remains one of the most concerning features of the Scottish diet. Low fruit and vegetable consumption is linked to poor health and increased risk of certain diseases, including heart disease and some cancers. Increased consumption of fruits and vegetables as part of a healthy diet may reduce the risk of these diseases in later life.
What vegetables are included?
All fresh, frozen and canned (in plain water) vegetables are included, whether offered as a salad, raw, cooked or as part of a dish (e.g. soups, stews and sandwiches).
Vegetables that are added to dishes such as soups, stews, casseroles, pasta-based dishes and sandwiches can only count as a portion if the vegetables are added in sufficient amounts (40g) per portion.
Pulses, such as baked beans, kidney beans, lentils and chickpeas can be classified as both a protein food or vegetable. However, they can only be counted as one portion of vegetables regardless of how much is offered. This is because pulses don’t give the same range of vitamins, minerals and other nutrients as other vegetables.
What foods are not counted as a vegetable portion?
Potatoes, including sweet potatoes, do not count as a vegetable portion because they are classified as starchy foods and are usually eaten as part of a meal in place of other sources of starch, such as pasta, rice and bread.
Spaghetti, hoops or pasta shapes in tomato sauce cannot be counted as a vegetable portion. This is because they are starchy foods and not vegetables, and tomato sauce does not contain the same mix of vitamins, minerals and fibre as a standard portion of vegetables.
Similarly, condiments such as tomato ketchup and pickled vegetables such as gherkins, onions and olives don’t count as a vegetable because they almost always have added salt and/or sugar.
What fruits are included?
All types of fruits whether fresh, frozen, canned (in natural juice) or dried are included.
Dried fruit can count as one of the fruit portions on offer across the day, but an alternative should always be available. Dried fruit should only be provided as part of a meal and not as a snack, to promote good oral health practices.
What foods are not counted as a fruit portion?
Fruit flavoured jelly does not count as a portion of fruit as it is unlikely to contain any or enough real fruit. Whole or chopped fruit added to jelly can be counted as a portion as long as it contains a minimum of 40g per portion.
What foods should not be offered?
Fruit juices and smoothies should not be made available at any point over the day. While sugars found in whole fruit don’t have a negative effect on our health, the free sugars found in fruit juice can be harmful to teeth. Fruit juice is acidic, and the fibre is also lost in processing.
Processed fruit products such as fruit bars, shapes and laces or fruit and vegetable crisps should not be served.
Include a variety of fruit and vegetables on the menu every day.
Different fruits and vegetables contain different combinations of vitamins, minerals, fibre and other nutrients. The menu should include a variety of fruit and vegetables over the week for children to get the most benefit and increase exposure to different types of tastes and textures. For example, peas should not be on the menu every day and, if serving salads regularly, try to include different types of fruit and vegetables.
Practical guidance
A typical portion of fruit or vegetables for 1 to 5 year olds should be around 40g. The serving sizes listed below should be used as a guide. Smaller children may need smaller servings, i.e. one serving is what a young child can hold in their hand.
Each portion can be made up of a variety of fruit and/or vegetables, for example four quarter portions of fruit as a fruit salad or two half portions of vegetables as a vegetable curry main dish.
Be aware of choking guidance. Always serve food appropriate to the age and stage of the child, and never leave children unattended while eating. See Section 5.6 for more information on choking and to access other relevant guidance.
| Food | Portion |
|---|---|
| Vegetables (fresh, frozen or canned) | 1-2 tablespoons of cooked vegetables |
| Salad | Small bowl, or 4-6 raw vegetable sticks |
| Vegetable-based soup | Small bowl |
| Pulses such as beans and lentils, when cooked | ½ -1 tablespoon |
| Vegetables in composite dishes, such as vegetable chilli or tomato pasta | 1-2 heaped tablespoons per serving of the recipe |
| Small-sized fruit, such as plums | 1-2 fruits |
| Medium-sized fruit, such as apples | ½ fruit |
| Large-sized fruit, such as melon | ½ -1 small slice |
| Bananas | ½ -1 small |
| Very small fruit such as blackberries | 1-2 tablespoons |
| Dried fruit | ½ -1 tablespoon or 2-5 pieces of dried fruit |
| Fruit in composite dishes, such as stewed fruit in desserts | 1-2 heaped tablespoons |
| Frozen fruit or canned fruit | 1-2 heaped tablespoons |
How to increase fruit and vegetable intake
- Add extra vegetables and pulses to stews, casseroles or other dishes, and add fresh, frozen, canned fruit in natural juice or dried fruit into desserts and puddings.
- Offering a variety of colours and options and presenting them in different ways can support their acceptance, for example, vegetable sticks with dip or fruit wedges with plain yoghurt.
- Offer unfamiliar vegetables or fruits on multiple occasions over time to encourage children to keep eating these. Pair vegetables with dishes that children are familiar with e.g. curry, pasta, soups and casseroles.
- Adding vegetables to soups can be a useful way of increasing vegetable intake. Vegetable-based soup should contain a minimum of one portion of vegetables (40g) per serving.
- Ensure that fruit crumbles and other composite fruit-based desserts contain at least one portion (40g) of fruit per serving.
- Adding fruit to breakfast cereal, or serving vegetables on crackers or toast, can provide alternatives to increase intake and acceptance.
Maximising desirable nutrients
Some vitamins and minerals can be lost easily when fruit and vegetables are prepared, cooked or stored, so bear the following in mind:
- Use fresh fruit and vegetables soon after purchase as the vitamin content will decrease the longer they are stored, or use frozen fruit and vegetables. This can help to reduce food waste too.
- Cook fruit and vegetables as soon as possible after cutting. If this is not possible, cover and chill them.
- Use cooking methods which use the minimum amount of water such as steaming, microwaving or boiling in minimal water.
- Serve fruit and vegetables as soon after cooking as possible.
Minimising less desirable nutrients
- Only use fruits canned in natural fruit juice and drain off the fruit juice before serving.
- Use vegetables and pulses canned in plain water and without added salt or sugar.
- If using manufactured soups, it is important to make sure they are varieties lower in fat, saturated fat and salt.
Standard 2: Oily fish
Main meal
Oily fish should be provided at least once every three weeks.
Light meal and snack
Oily fish should be provided once a week across light meal or snack on the weeks when it is not provided as a main meal.
Oily fish should be limited to a maximum of twice per week.
Why is this standard important?
Oily fish is a rich source of omega-3 fatty acids which have several health benefits including helping maintain a healthy heart. In Scotland and other parts of the UK we do not eat enough oily fish and need encouragement to consume more in our diet. Childcare settings can play a significant role in promoting oily fish consumption.
What are oily fish?
Oily fish are those fish which contain omega-3 fatty acids in their flesh. White fish only have very small amounts of these fats in their flesh, so do not count as oily fish. Tuna is no longer classed as an oily fish as it does not contain high enough levels of omega-3 fatty acids.
Examples of oily fish include fresh, canned or frozen salmon, mackerel, trout, herring, sardines or pilchards.
Practical guidance
- Offer regular small taster portions to introduce children to fish dishes they may not have tried before. Small tasters are a good way of helping children to accept new foods.
- Offer a variety of dishes over time to encourage children to keep eating oily fish. Try fish in dishes that children are familiar with such as curry, pasta and pizza.
- Use oily fish as a filling for sandwiches, wraps, kebabs and baked potatoes. It can also be used to make pâté or served as a salad choice.
- Fishcakes made with oily fish can be a popular choice. To begin with, try mixing oily fish with white fish to increase acceptability, and then gradually increase the amount of oily fish.
- Ensure that all practitioners are aware of the benefits of eating oily fish and get them to encourage children to eat these dishes.
- Try to avoid buying fish rated as ‘fish to avoid’ by the Marine Conservation Society and buy fish from sustainably managed stocks which is Marine Stewardship Council (MSC) certified.
- Shark, swordfish and marlin should be avoided until 16 years old due to mercury levels, which affects a growing nervous system, .
- If purchasing manufactured fish products, it is important to make sure they are varieties that are lower in fat, saturated fat and salt.
Standard 3: Red and red processed meat
Main meal and light meal
Red and red processed meat should be limited to a maximum of three times per week, one of which can be red processed meat, but at no more than one meal occasion per day.
Snack
These foods should not be provided at snack occasions.
Why is this standard important?
Red meat is a good source of nutrients, in particular iron, so can be part of a healthy diet, but we don’t need to eat it every day. Processed red meat can be high in fat and salt. Eating too much red and red processed meat can cause bowel cancer in later life.
This standard aims to reduce how often red and red processed meat are served to protect the health of children and set positive eating habits for the future.
What is red and red processed meat?
Red meat includes beef, lamb, mutton, pork, veal, venison, goat and offal from those sources.
Red processed meat includes sausages, hotdogs, ham, burgers and deli meats (e.g. salami, pâtés and corned beef). It also includes meats which have been cured, smoked or salted.
The term ‘processed meat’ refers to red meat that has been preserved by smoking, curing, salting or adding preservatives. The addition of ingredients such as egg, breadcrumbs, flour, seasoning and spices to red meat does not constitute processing and therefore would not be referred to as a processed meat product, provided it has not undergone any of the processes listed above or had preservatives added.
In addition, red meat which has undergone processing such as mincing or slicing is not classed as processed meat, provided it has not undergone further processing as outlined above.
Processed white meat and processed meat alternatives
Whilst processed white meat, such as chicken or turkey products and meat alternative products, are not restricted in the same way as red processed meat, these products can be high in fat and salt and should be carefully considered as part of any provision.
Practical guidance
To reduce red meat intake to three times per week or less, red and red processed meats can be swapped for beans, pulses, eggs, fish or white meat (including chicken and turkey) or meat alternatives (e.g. tofu and soya) to offer variety to the menu.
Meat alternatives should be as low in fat, salt and sugar as possible.
Any meat served should be as lean, and as low in fat and salt, as possible. You should take steps to reduce the fat content of your meat dishes as far as possible, for example, by trimming visible fat from meat before cooking, using leaner cuts of meat and draining any visible fat from dishes such as mince.
When cooking, consider whether grilling or oven baking instead of frying could be used to reduce the amount of fat used.
Consider reducing the meat content of dishes by substituting it with lentils, beans and/ or vegetables.
Vary fillings for sandwiches and baked potatoes. Alternatives to meat options, such as egg, beans, tuna or houmous could be used.
Standard 4: Yoghurts and fromage frais (including non-dairy alternatives)
All meals and snacks
Only plain and unsweetened yoghurts or fromage frais can be provided.
Why is this standard important?
Plain, unsweetened yoghurts and fromage frais (including fortified non-dairy alternatives) are good sources of calcium, which is important for good bone development.
They do not contain any added (free) sugar. Provision of these unsweetened products also aims to improve the overall diet by restricting foods high in sugar and limiting the provision of sweet-tasting foods.
Sweetened yoghurts and fromage frais (including non-dairy alternatives) should not be provided. This includes those that contain non-sugar sweeteners.
Practical guidance
Serve plain, unsweetened yoghurt and fromage frais (including non-dairy alternatives) with fruit or use to make dips for crudités.
When offering non-dairy alternatives these should be calcium-enriched whenever possible.
Standard 5: Sweetened and baked products, puddings, and desserts (including dairy and non-dairy alternatives)
Main meal and light meal
Sweetened and baked products, puddings and desserts (including dairy and non-dairy alternatives based desserts) should be limited to a maximum of three times per week, but no more than one meal occasion per day.
If combination dishes are provided, e.g. crumble and custard, this would be classed as one serving. It is important that the serving size reflects one portion.
Snack
These foods should not be provided at snack occasions.
Why is this standard important?
These types of products tend to contain high amounts of sugar, especially free sugars, as well as fat and saturated fat.
It is important that children are taught to see this type of product as one that should be enjoyed occasionally as part of a balanced diet.
Limiting the frequency that these products are available means that children could be encouraged to choose other items on offer such as fruit. For the products listed here this also applies to all sugar-free varieties.
What foods are included?
- Baked goods (including home baked and commercially produced), such as cookies, scones, muffins, bagels, traybakes, cakes, pancakes, waffles and brownies.
- Desserts, such as sponge pudding, cheesecake, crumbles and jelly (including sugar-free jelly).
- Other dairy-based and non-dairy alternatives desserts, such as custard, rice pudding and milk whip.
- Frozen desserts, such as ice cream and ice-lollies.
- Plain biscuits (including pre-packed), such as digestives and rich tea biscuits.
- Cereal bars, including breakfast bakes and bars (including home baked products).
- Sweet pastry products, such as croissants, Danish pastries, choux pastry, fruit pies and brioche.
Practical guidance
Focus on offering products which are generally lower in fat and sugar, such as plain scones and plain pancakes with fruit.
Serve with fruit to add variety.
Products such as jam, marmalades, syrup and honey should only be available at main meals and light meals, and used infrequently and sparingly. Refer to Standard 12.
Where possible, choose toppings and spreads that are low in fat, salt and sugar such as cream cheese spread and chopped or mashed fruit.
Ensure that spreads meet the standard for oils and spreads. Refer to Standard 11.
Confectionery should not be included on or in these products. Refer to Standard 13.
Baking recipes can be modified to make them healthier i.e. by reducing fat and sugar content or adding fibre rich ingredients such as oats or fruit.
Standard 6: Breakfast cereals
All meals and snacks
Only breakfast cereals meeting the following criteria can be provided:
- No more than 15g of total sugar per 100g.
- No more than 440mg sodium per 100g.
- No more than 1.1g of salt per 100g
- At least 3g of fibre per 100g.
Information on cereal bars is included in Standard 5.
Why is this standard important?
Breakfast cereals are often provided in early years settings. Most are fortified with added vitamins and minerals and can be a source of fibre[1]. However, some of these items are too high in sugar and salt and do not contain enough fibre.
What is an appropriate breakfast cereal?
Any breakfast cereal which meets all the above criteria.
Practical guidance
Focus on plain breakfast cereals and porridge without added sugar. Fruit could be used to add a variety of taste and textures. Sugar and products such as honey and syrups should not be added to breakfast cereals.
Check breakfast cereal packaging to ensure they meet the nutrition criteria in the standard.
Offer a variety of cereals to include different tastes and textures and to benefit from the range of nutrients provided within these.
Products with confectionery on or in them should not be available. Refer to Standard 13 for information on confectionery.
Standard 7: Fried foods
Main meal and light meal
Fried foods should be limited to a maximum of once per week. This includes any product which is fried in the manufacturing process.
Chips, if provided, should be served as part of a meal.
Deep frying should not be used as a cooking method.
Snack
These foods should not be provided at snack occasions.
Why is this standard important?
This standard is important in challenging the culture in Scotland of regularly eating chips and other fried foods. It aims to reduce fat intake by encouraging children to eat a healthy, balanced diet containing a variety of types of foods, and to only eat chips and fried foods occasionally as part of a meal.
What foods are included?
Any foods which are fried, either when cooking or during the manufacturing process. These foods can include chips, potato waffles, potato wedges, pakora, spring rolls and pre-prepared coated, battered and breaded products, e.g. chicken nuggets, fish fingers, vegetable fingers, potato shapes and battered vegetables. Deep-frying should not be used as a cooking method.
Practical guidance
Oven baked or air fried products are preferable as they are usually lower in fat. However, if you are frying always use clean oil and ensure that the oil is hot before frying. Using the right temperature and timing helps prevent too much fat being absorbed by the food.
If purchasing oven-baked products it is important to check these have not been fried in the manufacturing process. This information can be found on the labelling, look for terms such as ‘pre-fried’. These products are still considered to be fried and can only be served as the standard specifies.
Only use permitted oils for frying, e.g. rich in polyunsaturated or monounsaturated fats like sunflower oil or a mixed vegetable oil (refer to Standard 11 for guidance on fats and oils).
If purchasing manufactured products, it is important to make sure they are lower in fat, saturated fat and salt. Section 3.3 provides information on how to identify the fat, saturated fat and salt content of products.
Baked home-made products such as potato wedges, using a minimal amount of oil, could be a suitable alternative to fried products.
Stir frying is not included in this standard, as this involves cooking with minimal oil.
Standard 8: Savoury snacks
All meals and snacks
Only the following savoury snacks can be provided:
- Plain oatcakes.
- Plain savoury crackers.
- Plain rice cakes.
- Plain breadsticks.
Plain means those without the addition of other ingredients, seasonings, coatings or flavours such as cheese or yoghurt.
These should be limited to a maximum of once per day.
Why is this standard important?
Children need to be encouraged to eat a healthy, balanced diet. Savoury snacks such as crisps tend to be high in fat and salt and can often replace foods in the diet which may contain important nutrients.
What foods should not be served?
Any pre-packed snack items which can be eaten without preparation and consist of or include as a basic ingredient, potatoes, other root vegetables and cereals such as crisps, corn puff or corn snacks, cornmeal snacks, tortilla chips, pretzels, popcorn, prawn crackers, flavoured rice cakes and Bombay mix.
Practical guidance
Consideration should be given to suitable accompaniments to permitted snack products. Suitable suggestions include cheese, cream cheese spread, houmous or salmon pâté. Ensure accompaniments meet the relevant criteria.
Standard 9: Bread and bread rolls
All meals and snacks
Only bread and bread rolls which contain a minimum of 3g fibre per 100g can be provided.
Why is this standard important?
Bread is a starchy food which provides energy, a range of vitamins and minerals, and is a good source of fibre[2].
What types of bread are included?
All bread and rolls: pre-packed, part-baked, and freshly baked white, brown, malted grain, wholemeal and 50:50 bread or rolls including seeded products, French bread, ciabatta, focaccia, pitta, naan, panini roll, chapattis, flour tortillas (or wraps) with or without additions such as cheese, garlic or other flavourings such as herbs.
The form of the bread does not matter, e.g. sliced bread, home-made bread, baguettes and chapattis can all be used if this meets the minimum 3g fibre per 100g.
Practical guidance
Provide wholegrain, wholemeal or brown bread varieties regularly as they have more fibre and encourage children to eat a variety.
Higher fibre options (those with 6g or over per 100g) should be gradually introduced to young children’s diets. Higher fibre foods can be bulky and may fill children up, quickly displacing other important foods.
Ensure that spreads meet the standard for oils and spreads Standard 11. When possible, use toppings that are low in fat, salt and sugar.
Some breads have a lot of fat added to them and this makes them unsuitable to offer every day, for example, garlic bread.
Bread is one of the main sources of salt in the diets of people in the UK. Work is ongoing with the food industry to encourage reductions in the levels of salt in a wide range of processed foods, including bread. If purchasing bread, it is important to make sure that you select breads with the lowest salt content.
Standard 10: Savoury pastry and pastry products
Main meal and light meal
Savoury pastry and pastry products should be limited to a maximum of once per week.
Snack
These foods should not be provided at snack occassions.
Why is this standard important?
Pastry items often contain large amounts of fat, and some contain high amounts of saturated fat. Saturated fats contribute to the risk of heart disease by raising blood cholesterol levels.
This standard aims to improve the diet by restricting opportunities to over-consume items high in fat which can contribute to overall poorer nutrition. This will help to teach children to see these products as ones to be enjoyed occasionally as part of a balanced diet rather than every day.
What foods are included?
This includes all savoury pastry-based items including but not limited to:
- pies, sausage rolls, quiche and butteries.
Practical guidance
Alternatives to pastry-top pies may be to use sliced or mashed potatoes or vegetables.
When using pastry, use smaller portions.
Relevant HSCS:
1.19 My care and support meets my needs and is right for me.
1.34 If I need help with eating and drinking, this is carried out in a dignified way and my personal preferences are respected.
3.15 My needs are met by the right number of people.
5.17 My environment is secure and safe.
Standard 11: Oils and spreads
All meals and snacks
Oils should contain a saturated fat content of no more than 16g per 100g.
Fat spreads should contain a saturated fat content of no more than 20g per 100g.
Why is this standard important?
To ensure a healthy diet, it is not only important to limit the amount of total fat eaten, but to replace saturated fats with unsaturated fats (i.e. polyunsaturated and monounsaturated fats), which are a healthier alternative.
Saturated fats contribute to the risk of heart disease by raising blood cholesterol levels. Both polyunsaturated and monounsaturated fats have less of an effect on blood cholesterol levels and therefore help in reducing the risk of heart disease.
This means that butter, hard margarines, lard and certain cooking oils are not appropriate for use in childcare settings as they contain high levels of saturated fat. All oils and spreads used should meet the standards set above to restrict saturated fat and encourage the use of polyunsaturated and monounsaturated fats.
What types of oils are likely to be suitable?
Oils which are rich in monounsaturated and/or polyunsaturated fats are likely to include: olive, vegetable, rapeseed (canola), safflower, sunflower, corn, soya and linseed.
What types of spreads are likely to be suitable?
Spreads which are rich in monounsaturated and/or polyunsaturated fats are likely to include vegetable, rapeseed (canola), olive, sunflower and soya-based choices.
Practical guidance
Use oils and fats spreads sparingly by:
limiting the amount of oil in cooking and dressings.
limiting the amount of fat spread added to bread, sweetened baked products, sandwiches, potatoes and vegetables.
grilling or oven baking food instead of frying.
Standard 12: Salt, other condiments and preserves
Main meal and light meal
No salt should be used in cooking.
No salt should be provided to add to food after the cooking process is complete.
Other condiments, preserves, syrups and honey should only be provided infrequently and sparingly to add to the acceptability of a meal. When provided, these should be lower fat, salt and sugar varieties where possible.
Snack
These foods should not be provided at snack occasions.
Why is this standard important?
Most children consume more salt than they need. Eating too much salt increases the risk of high blood pressure, which may then lead to heart disease and stroke in later life.
Too much salt, too often will give children a taste for salty food and they will be more likely to continue eating too much salt when they grow up.
It is the sodium in salt that can have harmful effects on health. Some foods contain other forms of sodium, such as those used as flavour enhancers (e.g. monosodium glutamate) and raising agents (e.g. sodium bicarbonate).
Too much sugar will give children a taste for sugary foods. Foods high in sugar, especially free sugars, can be damaging to health, particularly our teeth. Foods high in sugar, such as preserves provide very few nutrients.
Condiments and preserves are often high in fat, salt and/or sugar (including free sugars).
What is included?
- All salts and condiments including but not limited to table salt, sea salt, tomato ketchup, brown sauce, mayonnaise, salad cream, French dressing, mustard, soy sauce, Worcestershire sauce, barbecue sauce, tabasco sauce, plain and creamed horseradish sauce, mint sauce, mint jelly, tartare sauce, pickles and relishes.
- Preserves are made with fruit preserved in sugar, including but not limited to jams, chutney, conserve, fruit butter, fruit curd, fruit spread and marmalade.
- Syrups and honey.
Practical guidance
Do not use salt in the cooking process, e.g. salting potatoes or vegetables.
Products which have a higher salt content, for example soy sauce and stock cubes, should be used very occasionally and ideally replaced with other flavourings such as garlic, lemon juice, herbs and spices.
Choose foods that have a lower salt content when purchasing manufactured foods. Foods such as bread products, prepared meals and sauces often contain high amounts of salt.
Limit the use of condiments. These should only be used when required to enhance flavour or add moisture, for example tomato ketchup with a burger/meat alternative, which may otherwise be too dry without it.
Use healthier alternatives such as dressings or sauces made with plain yoghurt enhanced with suitable flavourings such as herbs.
Use lower fat, salt and sugar versions of condiments and preserves where possible and use sparingly and infrequently.
Do not have condiments and preserves on the table for children to help themselves, this is likely to lead to increased portions.
Standard 13: Confectionery
All meals and snacks
Confectionery should not be provided at any time.
Why is this standard important?
Confectionery items contain large amounts of free sugars, and some also contain high amounts of fat. These foods are high in energy but provide very few nutrients such as protein, vitamins and minerals, and fibre. Sugar-free sweets also provide little nutritional value and could displace other more nutritious food from the diet.
This standard aims to improve oral health by reducing the frequency that children consume sugars. It also aims to improve the overall diet by restricting foods high in sugar and fats.
What is included?
The term confectionery refers to the following groups of products:
- Chocolate in any form, any product containing or wholly or partially coated with chocolate and any chocolate flavoured substance e.g . bars of milk, plain or white chocolate, chocolate flakes, chocolate buttons, chocolate chips , chocolate filled eggs, chocolate drizzled products such as biscuits or chocolate covered products such as choc ices but excludes cocoa powder used in sweetened and baked products and drinks.
- Non-chocolate confectionery (whether or not containing sugar) e.g. boiled, gum/gelatine, liquorice, mint and other sweets, lollipops, fudge, tablet, toffee, sherbet, marshmallows, sprinkles, chewing gum or processed fruit sweets and bars.
- Any sugared, or wholly or partially yoghurt-coated products e.g. sugared or yoghurt coated fruit and nuts, or yoghurt drizzled cereal bars and biscuits.
What is not included?
Cocoa powder (not drinking chocolate) can be used in cakes, biscuits and puddings to allow flexibility in developing menus.
Practical guidance
The use of any sweetened items should be limited. Any cakes, biscuits, ice-cream, etc. which are included as part of the menu should not contain confectionery.
Cakes and biscuits should not be used as a substitute for confectionery.
Standard 14: Drinks
All meals and snacks
The only drinks that should be provided are:
- Still, plain water.
- Plain milk or unsweetened fortified non-dairy alternative.
Why is this standard important?
It is important that young children are well hydrated. They have a higher proportion of body water than adults, are less heat tolerant and may be more likely to get dehydrated.
Water and milk are the preferred drinks for children to quench thirst. Cows’ milk can be a good source of protein, vitamins and minerals, especially calcium which is needed to build healthy bones and teeth. Milk contains a high percentage of water and is therefore also good for hydration.
What is included?
Semi-skimmed milk should be provided to children aged 1 year unless otherwise advised by a parent/carer or healthcare professional. Skimmed or 1% fat milk is not suitable for children aged under 5 years.
- Where children cannot drink cows’ milk for medical, ethical or religious reasons, plain goats’ or sheep’s milk can be provided. If these types of milk are unsuitable for medical, ethical or religious reasons, an unsweetened non-dairy alternative drink can be provided. These are defined as a drink which is an unsweetened, calcium-enriched liquid and is commonly used as a substitute for milk.
- Unsweetened calcium-enriched soya drinks are the closest nutritional equivalent to plain cows’ milk, and these should be the first option for children who cannot drink dairy milks. Other unsweetened, calcium-enriched non-dairy alternative drinks may be offered only where a child cannot drink an unsweetened, calcium-enriched soya milk. A guide to support choosing an unsweetened, calcium-enriched, soya drink is included in Appendix 2.
What is not included?
Rice drinks should not be given to children under 5 years of age due to concerns about the levels of arsenic in the milk.
Fruit juice, vegetable juice, smoothies, flavoured milk, fruit juice combinations and diluting juice (including no added sugar or sugar free versions) should not be provided at any time in childcare settings due to their high free sugar content and/or sweet taste.
Practical guidance
Water should be freely available throughout the day.
Semi-skimmed milk should be provided for this age group, unless otherwise advised by a parent/carer or healthcare professional.
Milk and water can be provided at each meal and snack occasion but is only shown at snack times and some breakfast occasions on the sample menus. However, large volumes of milk after 1 year are discouraged (i.e. more than 600ml) as it may reduce appetite for other foods.
3.5 Sample menus for 1 to 5 year olds
The following menu samples provide an example of how menus can be planned to meet the nutritional requirements of young children. It is not compulsory to implement these menus, but they can be used to inform your menu planning process, along with the food and drink standards.
These menus have been developed to meet the food and drink standards in Section 3.4. They have also been nutritionally analysed against the nutrient standards, which can be found in Appendix 1. There is no expectation that settings will nutritionally analyse their menus, however some may choose to do so.
You can use below menus as a guide to help provide a varied menu in your setting. The recipes, which include average portion sizes can be found online.
Consider the Eatwell guide when planning your menus.
Sample menu week 1
| Monday | Tuesday | Wednesday | Thursday | Friday | |
|---|---|---|---|---|---|
| Breakfast | Toast with spread, plain yoghurt and pineapple slices Milk |
Malted wheat cereal with milk, toast with spread and sliced plum | Toast with spread, scrambled egg, and tomatoes Milk |
Wheat biscuits with milk, toast with spread and banana | Porridge, toast with spread and blueberries |
| Mid- Morning Snack | Crackers with sliced banana | Carrot sticks with cheese dip Milk |
Rice cakes and mandarin segments Milk |
Hard-boiled egg quarters and tomatoes Milk |
Plain fromage frais with sliced peaches |
| Lunch | Roast chicken with gravy, mashed potatoes and a vegetable medley Baked apple with custard or fruit selection |
Pork and vegetable noodles Plain fromage frais with pear slices or fruit selection |
Beef casserole Cheese & crackers with sliced grapes or fruit selection |
Salmon fish cake with potato wedges, peas & sweetcorn Plain yoghurt with mixed berries or fruit selection |
Pasta with tomato and lentil sauce and wholemeal garlic bread Lemon shortbread with strawberries or fruit selection |
| Mid- Afternoon Snack | Pepper sticks with houmous dip Milk |
Pesto pasta and blueberries | Cucumber sticks with mint yoghurt dip | Rice salad and strawberries | Wholemeal pitta strips with spread and melon slices Milk |
| Tea | Carrot and butter bean soup with a wholemeal roll Peaches in juice or fruit selection |
Tuna and cucumber wrap Fruit platter |
Cous cous with chickpeas and tomatoes Apricot and raisin flapjack with banana slices or fruit selection |
Vegetable sticks with houmous dip Muffin pizza faces with pasta twists |
Baked potato with baked beans Fruit salad with plain yoghurt or fruit selection |
|
|||||
Sample menu week 2
| Monday | Tuesday | Wednesday | Thursday | Friday | |
|---|---|---|---|---|---|
| Breakfast | Wheat biscuits with milk, toast with spread and blueberries | Toast with spread, plain yoghurt and peach slices Milk |
Porridge, toast with spread and mixed berries | Malted wheat cereal with milk, toast with spread and melon slices | Toast with spread, scrambled egg and tomatoes Milk |
| Mid- Morning Snack | Hard boiled egg quarters with cucumber sticks | Rice cakes and strawberries | Fruity rice and melon slices | Plain fromage frais with sliced plums Milk |
Pepper sticks with cream cheese dip Milk |
| Lunch | Mixed beans and tomato sauce with cous cous Plain fromage frais with pineapple in juice or fruit selection |
Creamy chicken and vegetable pasta Apple and pear oat crumble with custard or fruit selection |
Vegetable sticks with houmous dip Pork sausage with mashed potatoes and baked beans |
Beef mince and vegetables with boiled potatoes and broccoli Rice pudding with raisins or fruit selection |
Fish curry with rice Plain yoghurt with sliced plum or fruit selection |
| Mid- Afternoon Snack | Wholemeal pitta strips with spread and sliced grapes Milk |
Carrot sticks with houmous dip Milk |
Plain yoghurt with pear slices Milk |
Crackers with sliced banana | Pasta salad and apple slices |
| Tea | Macaroni cheese with spinach Fruit platter |
Baked potato with tuna and sweetcorn Sliced mandarins in juice or fruit selection |
Vegetable frittata with pasta twists Fruit platter |
Mackerel pâté and pepper wrap Fruit salad with plain yoghurt or fruit selection |
Vegetable and lentil soup with a wholemeal roll Chocolate orange cupcake with sliced apple or fruit selection |
|
|||||
Vegetarian sample menu
| Monday | Tuesday | Wednesday | Thursday | Friday | |
|---|---|---|---|---|---|
| Breakfast | Wheat biscuits with milk, toast with spread and blueberries | Toast with spread, plain yoghurt and peach slices Milk |
Porridge, toast with spread and mixed berries | Malted wheat cereal with milk, toast with spread and melon slices | Toast with spread, scrambled egg and tomatoes Milk |
| Mid- Morning Snack | Hard boiled egg quarters with cucumber sticks | Rice cakes and strawberries | Fruity rice and melon slices | Plain fromage frais with sliced plums Milk |
Pepper sticks with cream cheese dip Milk |
| Lunch | Mixed beans and tomato sauce with cous cous Plain fromage frais with pineapple in juice or fruit selection |
Chicken style pieces and vegetable pasta Apple and pear oat crumble with custard or fruit selection |
Vegetable sticks with houmous dip Vegetarian sausage with mashed potatoes and baked beans |
Vegetarian mince and vegetables with boiled potatoes and broccoli Rice pudding with raisins or fruit selection |
Tofu curry with rice Plain yoghurt with sliced plum or fruit selection |
| Mid- Afternoon Snack | Wholemeal pitta strips with spread and sliced grapes Milk |
Carrot sticks with houmous dip Milk |
Plain yoghurt with pear slices Milk |
Crackers with sliced banana | Pasta salad and apple slices |
| Tea | Macaroni cheese with spinach Fruit platter |
Baked potato with baked beans Sliced mandarins in juice or fruit selection |
Vegetable frittata with pasta twists Fruit platter |
Cream cheese & pepper wrap Fruit salad with plain yoghurt or fruit selection |
Vegetable and lentil soup with a wholemeal roll Chocolate orange cupcake with sliced apple or fruit selection |
|
|||||
3.6 Menu checklist
Use this checklist to help with your menu planning.
| Light Meals | Has this been achieved? (√) | |
|---|---|---|
| Yes | No | |
| A fruit and/or vegetable portion should be provided. (Standard 1) | ||
| Oily fish should be provided once a week across light meal or snack on the weeks when it is not provided as a main meal. | ||
| Oily fish should be limited to a maximum of twice per week. (Standard 2)* | ||
| Red and red processed meat should be limited to a maximum of three times per week, one of which can be red processed meat, but at no more than one meal occasion per day. (Standard 3) ** | ||
| Only plain and unsweetened yoghurts or fromage frais can be provided. (Standard 4) | ||
Sweetened and baked products, puddings and desserts (including dairy and non-dairy alternatives based desserts) should be limited to a maximum of three times per week, but no more than one meal occasion per day. If combination dishes are provided e.g. crumble and custard, this would be classed as one serving. It is important that the serving size reflects one portion. (Standard 5) ** |
||
Only breakfast cereals meeting the following criteria can be provided:
(Standard 6) |
||
Fried foods should be limited to a maximum of once per week. This includes any product which is fried in the manufacturing process. Chips, if provided, should be served as part of a meal. Deep frying should not be used as a cooking method. (Standard 7)** |
||
Only the following savoury snacks can be provided:
Plain means those without the addition of other ingredients, seasonings, coatings or flavours such as cheese or yoghurt. These should be limited to a maximum of once per day. (Standard 8)^ |
||
| Only bread and bread rolls which contain a minimum of 3g fibre per 100g can be provided. (Standard 9) | ||
| Savoury pastry and pastry products should be limited to a maximum of once per week. (Standard 10) ** | ||
Oils should contain a saturated fat content of no more than 16g per 100g. Fat spreads should contain a saturated fat content of no more than 20g per 100g. (Standard 11) |
||
No salt should be used in cooking. No salt should be provided to add to food after the cooking process is complete. Other condiments, preserves, syrups and honey should only be provided infrequently and sparingly to add to the acceptability of a meal. When provided, these should be lower fat, salt and sugar varieties where possible. (Standard 12) |
||
| Confectionery should not be provided at any time. (Standard 13) | ||
The only drinks that should be provided are:
(Standard 14) |
||
* Maximum applicable across week for main meal, light meal and snack combined.
** Maximum applicable across week for main meal and light meal combined.
^ Maximum applicable across the day for main meal, light meal and snack combined.
| Main Meals | Has this been achieved? (√) | |
|---|---|---|
| Yes | No | |
At least two portions of vegetables should be provided. Where a dessert is provided, a portion of fruit should always be an option. (Standard 1) |
||
| Oily fish should be provided at least once every three weeks. | ||
| Oily fish should be limited to a maximum of twice per week. (Standard 2)* | ||
| Red and red processed meat should be limited to a maximum of three times per week, one of which can be red processed meat, but at no more than one meal occasion per day. (Standard 3)** | ||
| Only plain and unsweetened yoghurts or fromage frais can be provided. (Standard 4) | ||
Sweetened and baked products, puddings and desserts (including dairy and non-dairy alternatives based desserts) should be limited to a maximum of three times per week, but no more than one meal occasion per day. If combination dishes are provided e.g. crumble and custard, this would be classed as one serving. It is important that the serving size reflects one portion. (Standard 5)** |
||
Only breakfast cereals meeting the following criteria can be provided:
(Standard 6) |
||
Fried foods should be limited to a maximum of once per week. This includes any product which is fried in the manufacturing process. Chips, if provided, should be served as part of a meal. Deep frying should not be used as a cooking method. (Standard 7)** |
||
Only the following savoury snacks can be provided:
Plain means those without the addition of other ingredients, seasonings, coatings or flavours such as cheese or yoghurt. These should be limited to a maximum of once per day. (Standard 8)^ |
||
| Only bread and bread rolls which contain a minimum of 3g fibre per 100g can be provided. (Standard 9) | ||
| Savoury pastry and pastry products should be limited to a maximum of once per week. (Standard 10) ** | ||
Oils should contain a saturated fat content of no more than 16g per 100g. Fat spreads should contain a saturated fat content of no more than 20g per 100g. (Standard 11) |
||
No salt should be used in cooking. No salt should be provided to add to food after the cooking process is complete. Other condiments, preserves, syrups and honey should only be provided infrequently and sparingly to add to the acceptability of a meal. When provided, these should be lower fat, salt and sugar varieties where possible. (Standard 12) |
||
| Confectionery should not be provided at any time. (Standard 13) | ||
The only drinks that should be provided are: Still, plain water. Plain milk or unsweetened fortified non-dairy alternative. (Standard 14) |
||
| Snacks | Has this been achieved? (√) | |
|---|---|---|
| Yes | No | |
A fruit and/or vegetable portion should be provided. Dried fruit should not be provided. (Standard 1) |
||
| Oily fish should be provided once a week across light meal or snack on the weeks when it is not provided as a main meal. | ||
| Oily fish should be limited to a maximum of twice per week. (Standard 2)* | ||
| Red or red processed meat should not be provided. (Standard 3) | ||
| Only plain and unsweetened yoghurts or fromage frais can be provided. (Standard 4) | ||
| Sweetened and baked products, puddings, and desserts (including dairy and non-dairy alternatives) should not be served. (Standard 5) | ||
Only breakfast cereals meeting the following criteria can be provided:
(Standard 6) |
||
| Fried foods should not be provided. (Standard 7) | ||
Only the following savoury snacks can be provided:
Plain means those without the addition of other ingredients, seasonings, coatings or flavours such as cheese or yoghurt. These should be limited to a maximum of once per day. (Standard 8)^ |
||
| Only bread and bread rolls which contain a minimum of 3g fibre per 100g can be provided. (Standard 9) | ||
| Savoury pastry and pastry products should not be provided. (Standard 10) | ||
Oils should contain a saturated fat content of no more than 16g per 100g. Fat spreads should contain a saturated fat content of no more than 20g per 100g. (Standard 11) |
||
| Salt, other condiments, and preserves should not be provided. (Standard 12) | ||
| Confectionery should not be provided at any time. (Standard 13) | ||
The only drinks that should be provided are:
(Standard 14) |
||
* Maximum applicable across week for main meal, light meal and snack combined.
** Maximum applicable across week for main meal and light meal combined.
^ Maximum applicable across the day for main meal, light meal and snack combined.
Contact
Email: elc@gov.scot
There is a problem
Thanks for your feedback